Blood banking:- part 1- Blood Groups ABO and Rh System, Blood Grouping Procedures
Blood Groups ABO and Rh System
What sample is needed for the ABO Blood Group and Rh System?
- This can be done on whole blood or even on clotted blood.
- The sample can be stored at 4 °C and is stable for 5 days.
- Sometimes weak subgroups may result in mistyping, where Coombs’ test may be helpful.
What are the indications for Blood Groups ABO and Rh System?
- ABO blood grouping and Rh typing are done before donating the blood.
- Blood grouping is done for the donor and the recipient (Crossmatch).
- Blood grouping is done in the expectant mother and newborn to rule out Rh-incompatibility.
ABO system:
What is the history of blood groups?
- German scientist Karl Landsteiner (an Austrian-born pathologist) first described blood groups having inherited differences in 1900.
- These antibodies were originally discovered in the early 1900s and are now known to comprise the immunoglobulin classes IgM, IgG, and IgA.
- Karl Landsteiner opened the door to blood banking.
- He took his blood sample and the blood samples of 6 of his colleagues in 1901.
- Separated the serum and prepared the RBCs’ saline suspension.
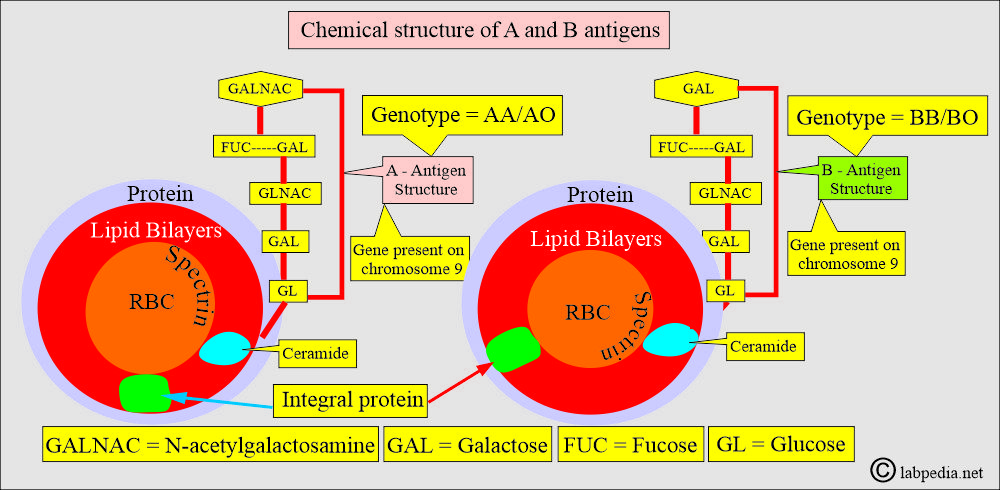
What is the inheritance of ABO-RBC genes and the chemical structure of antigens A and B?
- The theory for the inheritance of the ABO blood groups was first time described by Bernstein in 1924.
- He postulated that each individual inherits one ABO gene from each parent; these 2 genes decide which ABO antigens are present on the RBC membrane.
- One locus on each chromosome 9 is occupied by an A, B, or O gene.
- It has three alleles: A, B, and O.
- Codominants are A and B.
- While O is recessive.
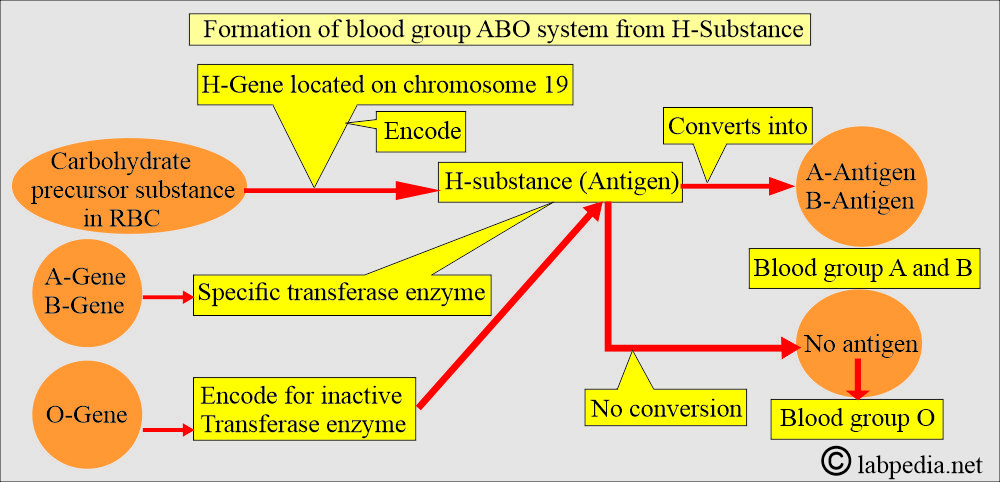
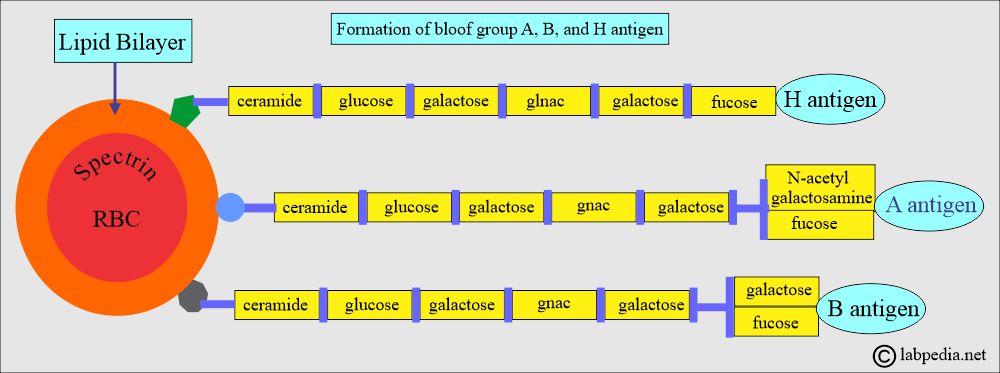
- H-antigen plays major role in the ABO blood group system. H-antigen is the precursor for the A and B antigens.
- H-antigen is the basic carbohydrate structure present on the red blood cells.
- H-antigen is the foundation upon which A and B antigens form.
- ABO genes do not code for the production of ABO antigens but rather produce specific glycosyl-transferases that add sugars to the basic precursor substance (H-antigen).
- The inheritance of the H- gene is independent of the inheritance of ABO genes. Still, A, B, and H antigens are formed from the same basic precursor material, genetic products.
- The basic material is a glycoprotein or glycolipid that serves as the backbone to which sugars are added in response to specific enzyme transferases, as indicated by the inherited genes of the parents.
What are the enzymes on the H-antigen leading to A and B antigen formation?
| Enzyme | Type of sugar added | Antigen formation |
| A transferase, from the A gene | N-acetylgalactosamine | A- antigen |
| B transferase, from the B gene | Galactose | B-Antigen |
| No transferases, O allele | No sugar added | H-antigen acts as the O group |
- Tests for the ABH secretion may help establish the true ABO group of an individual whose red blood cell antigens are poorly developed.
- The presence of A, B, and H substances in the saliva is evidence of the inheritance of an A gene, a B gene, and an H gene.
- The presence of the A, B, and H antigens in the saliva and body fluids is called secretors.
- The O gene is considered an amorphous, silent gene.
- The designation A or B refers to phenotypes, whereas AA, BO, and OO refer to genotypes.
What is the role of H-substance on ABO system formation?
- H-gene is present on chromosome 19. It encodes carbohydrate precursor substances in red blood cells (RBCs).
- Antigens A and B are controlled by specific genes present on chromosome 9 (9q34).
- A and B genes have specific transferase enzymes that act on H-substances.
- There is the formation of A and B antigens.
- While the O-gene encodes for an inactive transferase enzyme and ultimately leads to the formation of blood group O.
How will you summarize the ABO system?
| Clinical features | A-antigen | B-antigen |
| It is controlled by | ABO gene = A allele | ABO gene = B allele |
| Chromosome for the A and B antigens | Chromosome 9 | Chromosome 9 |
| Type of the enzyme | A transferase | B transferase |
| Addition of the sugar | N-acetylgalactosamine | Galatose |
What is the mechanism of ABO antibodies formation?
- Blood group ABO system antibodies are stimulated by the bacteria and the other substances in our surroundings.
- These antibodies result from cross-reactivity and are initiated at birth upon exposure to foreign substances. These are usually low (titer) at birth, detectable until the infants are 3 to 6 months old. It is logical to perform only forward grouping in newborn babies.
- The peak level occurs between 5 and 10 years of age, and then progressively declines with advancing age.
- Patients older than 65 will have low titer; antibodies in the reverse grouping may be undetectable.
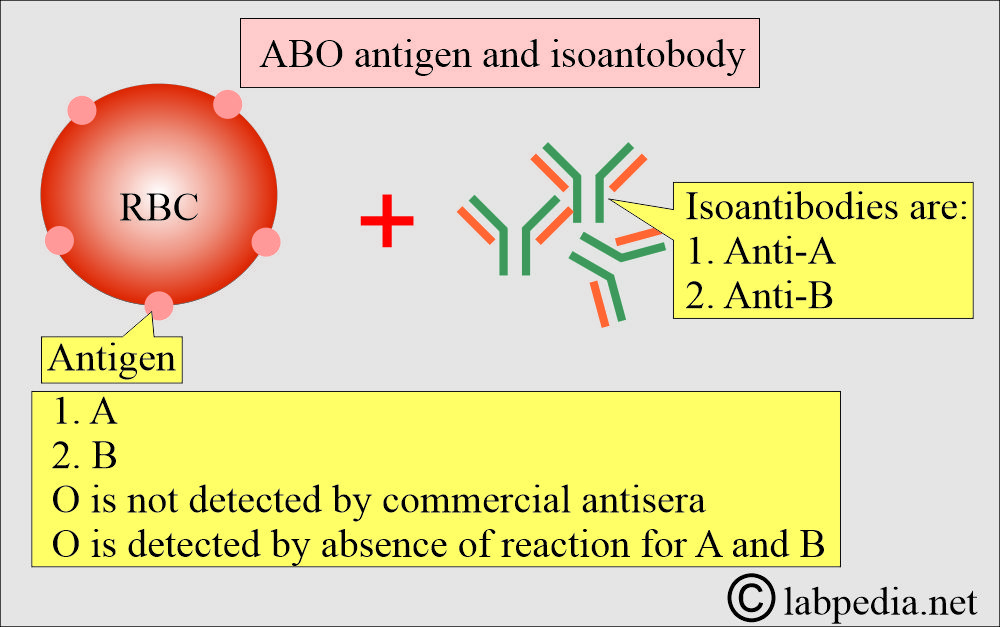
What is the basic principle for Blood group antigens?
- Blood grouping is done based on the presence of antigens on the surface of RBCs.
- There are two major antigens, A and B.
- So the basic principle of blood donation is that there should be no antibody to match the RBCs’ surface antigen.
- In the USA, blood group frequency is:
- Blood group O = 45%
- Blood group A = 41%
- Blood group B = 10%
- Blood group AB = 4%
What is the possibility of ABO phenotypes in the various population?
| The phenotype of the ABO system | Asian | Mexican | Blacks | Whites |
| O | 43% | 56% | 49% | 45% |
| A1 | 27% | 22% | 19% | 33% |
| A2 | Rare | 6% | 8% | 8% |
| B | 25% | 13% | 19% | 10% |
| A1B | 5% | 4% | 3% | 3% |
| A2B | Rare | Rare | 1% | 1% |
Where will you find A, B, and H substances?
- Saliva.
- Teras.
- Milk.
- Amniotic fluids.
- Digestive juices.
- Bile.
- Urine.
- Pathological fluids like pleural, peritoneal, pericardial fluids, and ovarian cysts.
What is the presence of ABH substances in the saliva?
| Blood group ABO system | A-antigen Substance in saliva | B-antigen Substance in saliva | H-Substance in saliva |
| A antigens | High concentration | None | Scanty |
| B antigen | None | High concentration | Scanty |
| A B antigen | High concentration | High concentration | Scanty |
| Blood group O | None | None | High concentration |
Blood groups A, B, and O system:
What are the Blood group antigens and types?
- Only two antigens, known as A and B antigens, explain the four blood groups.
- Later, it was found that an individual who does not have either A or B or both antigens possesses antibodies against these missing antigens and is called blood group O.
- The A, B, and O antigens are present in most human body cells, including white blood cells and platelets.
- Later on, was found subgroups of the ABO system:
- Blood group A = A1 and A2.
- Blood group B = A1B and A2B.
- Other subgroups of A are A3, Ax, and Am.
- Blood Group B also has subgroups, but these are very rare.
What is the inheritance of the blood groups?
- The ABO system of inheritance was first suggested in 1908 and subsequently proven in 1910.
- There are three allelic genes = A, B, and O.
- Each individual inherited two genes, one from each parent.
- The O gene does not produce a product and is therefore called amorphic (having no defined shape).
- The expression of genes A and B is dependent upon gene H.
- In 1930, Thompson postulated 4 allelic genes:
- A1, A2, B, and O.
- The 4 alleles give rise to 6 phenotypes and 10 genotypes.
- In 80% of the population that possesses the secretor gene, these antigens are also soluble in secretions and body fluids, such as plasma, saliva, sweat, and semen.
- 75% of the individuals secrete substances in their saliva with the same specificity as the ABO antigens on the RBCs.
- All the secretors secrete H substance.
- A and B substances are secreted in addition to H substances by groups A and B individuals, while group AB secretes A, B, and H substances.
- It depends on the presence of two antigens on the surface of RBCs, specifically antigen A and antigen B.
What is the structure of antigens A, B, and H?
- The ABO genes do not code for the production of the ABO antigens. However, it produces specific glycosyltransferases that add sugar to the basic precursor substances.
- The A and B genes control the specific enzymes responsible for adding single carbohydrate residues for groups A and B to basic antigenic glycoproteins or glycolipids with terminal sugar fucose on the RBCs known as H substance.
- The action of the H gene substance ultimately gives rise to ABO antigens.
- The O gene is amorphous and does not transform the H substance.
- Blood group O is considered the universal donor, as it can be transfused to all other blood groups. It should be done only in an emergency.
- While the blood group AB is a universal recipient that can receive blood from all other groups.
What are the types of blood groups?
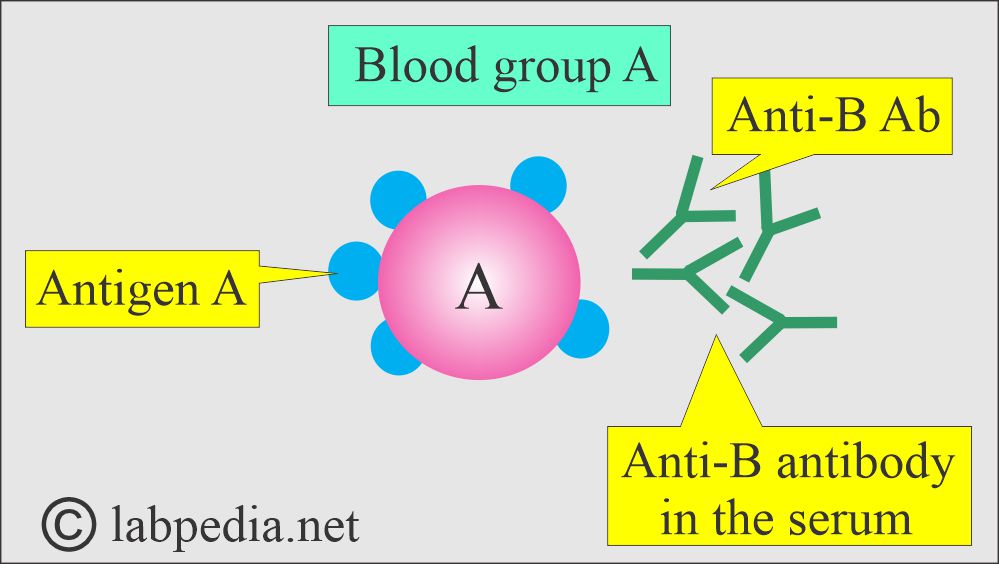
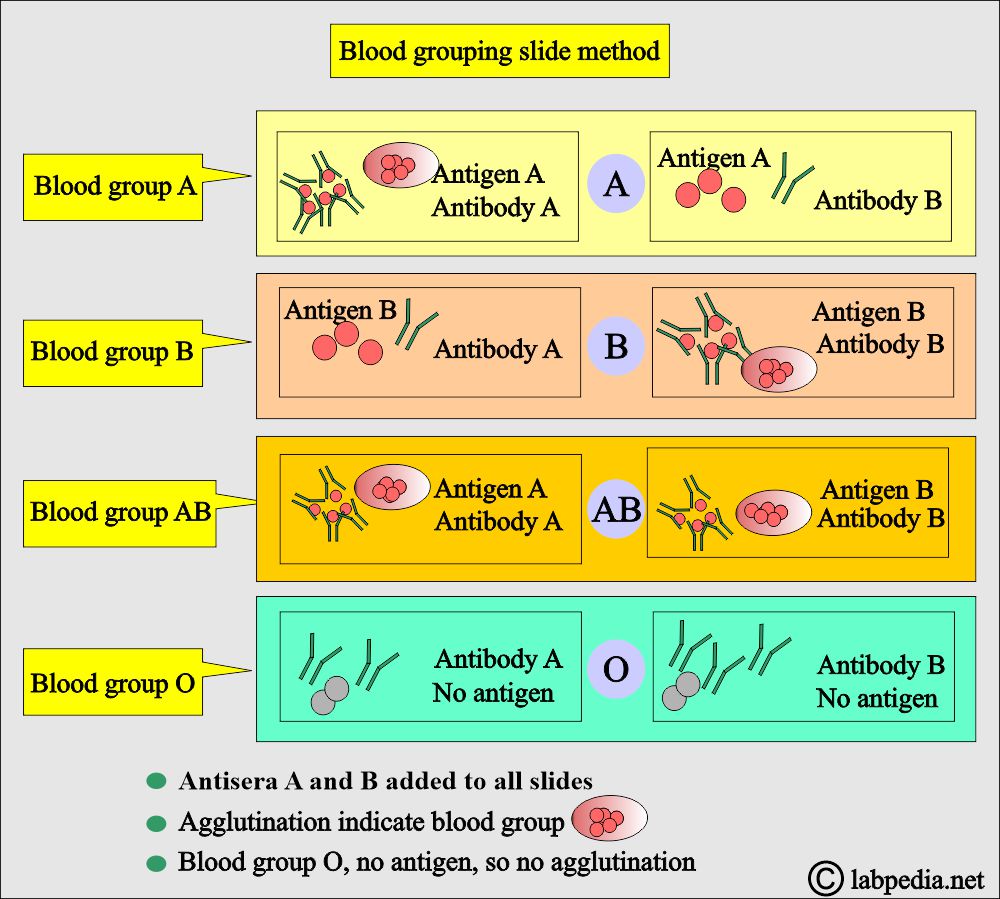
Blood group A:
- It has antigen-A and antibody-B.
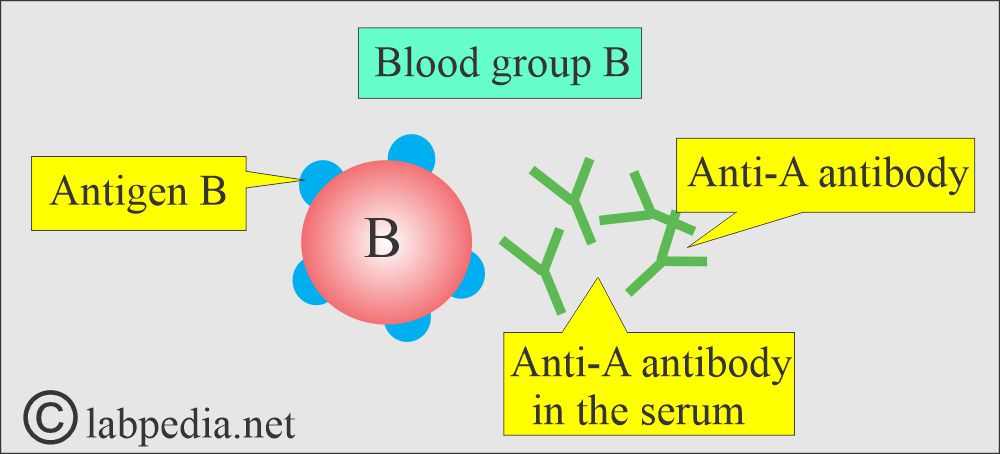
Blood group B:
- It has B-antigen and antibody-A.
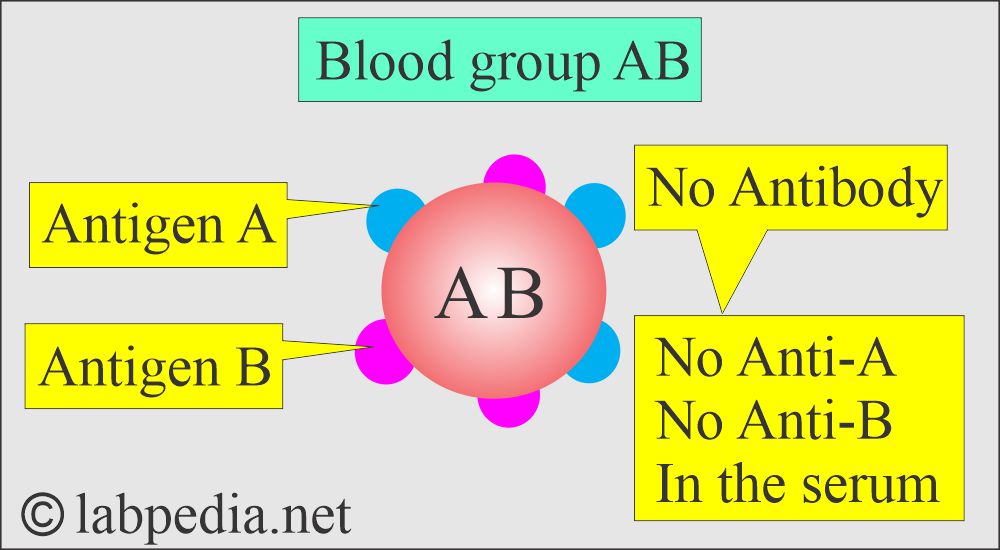
Blood group AB:
- It has both antigen-A and antigen-B, and no antibodies are present in the serum.
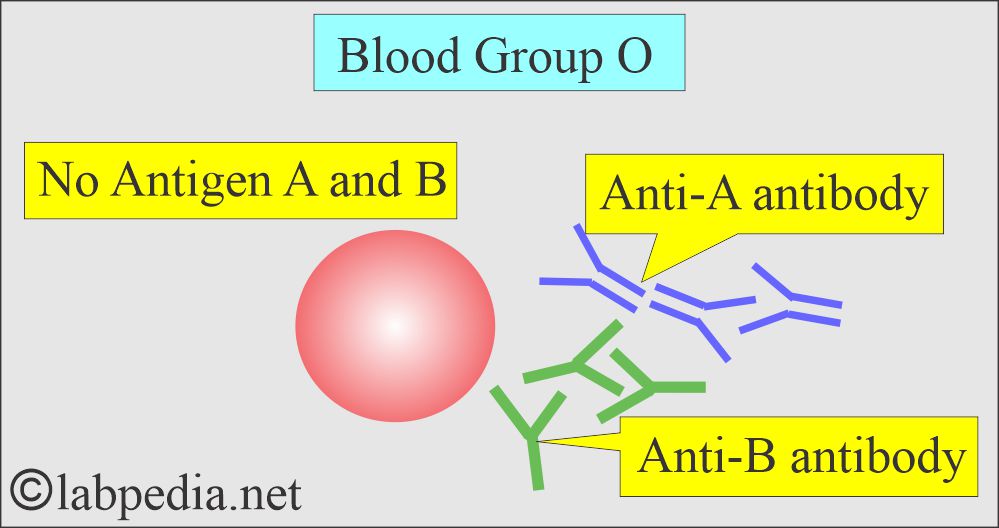
Blood group O:
- It has no antigen and has antibodies anti-A and anti-B.
What are the ABO system phenotypes and genotypes?
| Phenotypes of the blood groups | Genotypes of the blood groups |
|
|
|
|
|
|
|
|
|
|
|
|
What are the antigen and antibody in the ABO system?
| Blood group | Antigen on RBC | Antibody in blood |
|
|
|
|
|
|
|
|
|
|
|
|
How will you perform Blood grouping based on history?
- Karl Landsteiner performed the forward grouping and reverse grouping:
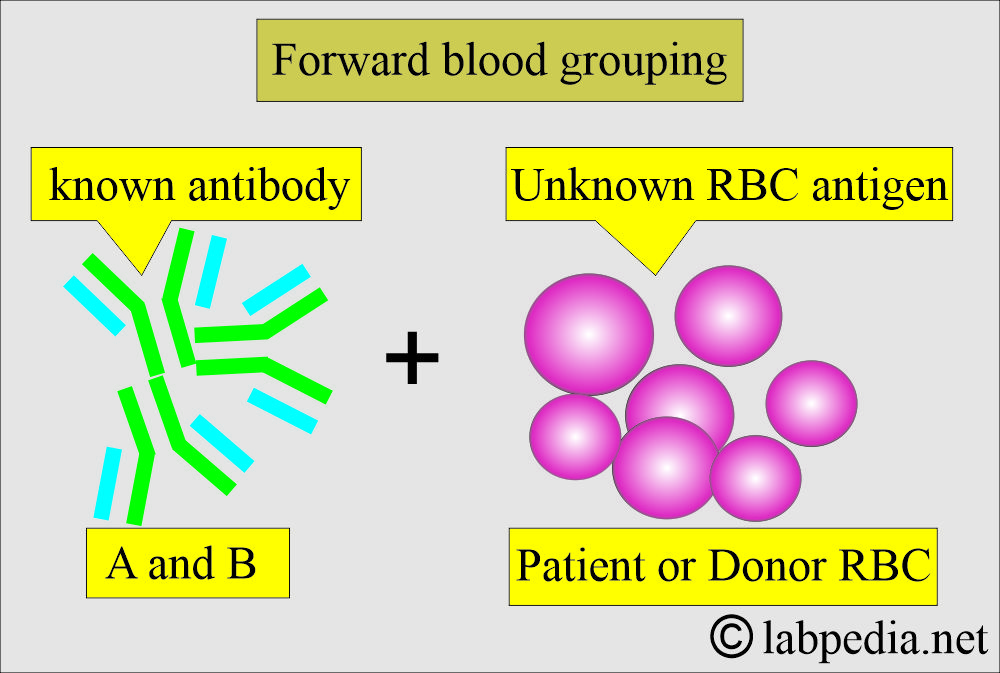
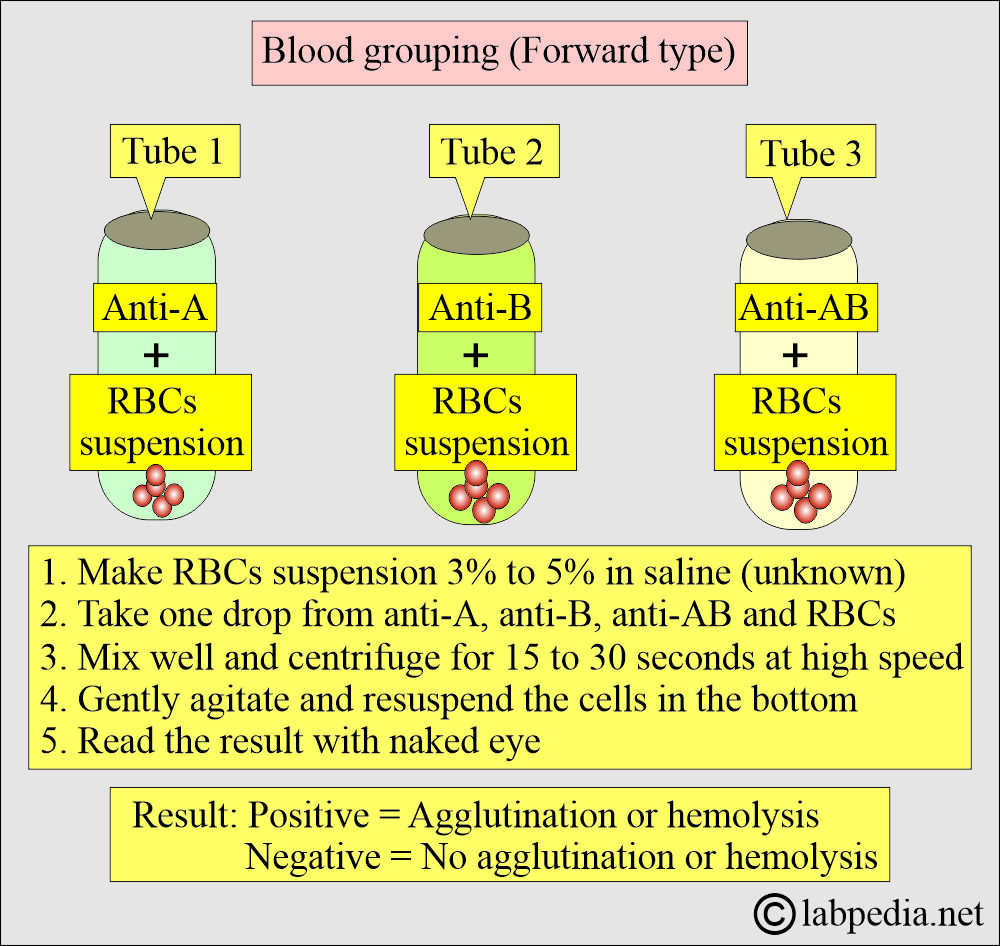
What is Forward grouping?
- It is defined as using a known source of antibodies to detect the antigens in the red blood cells.
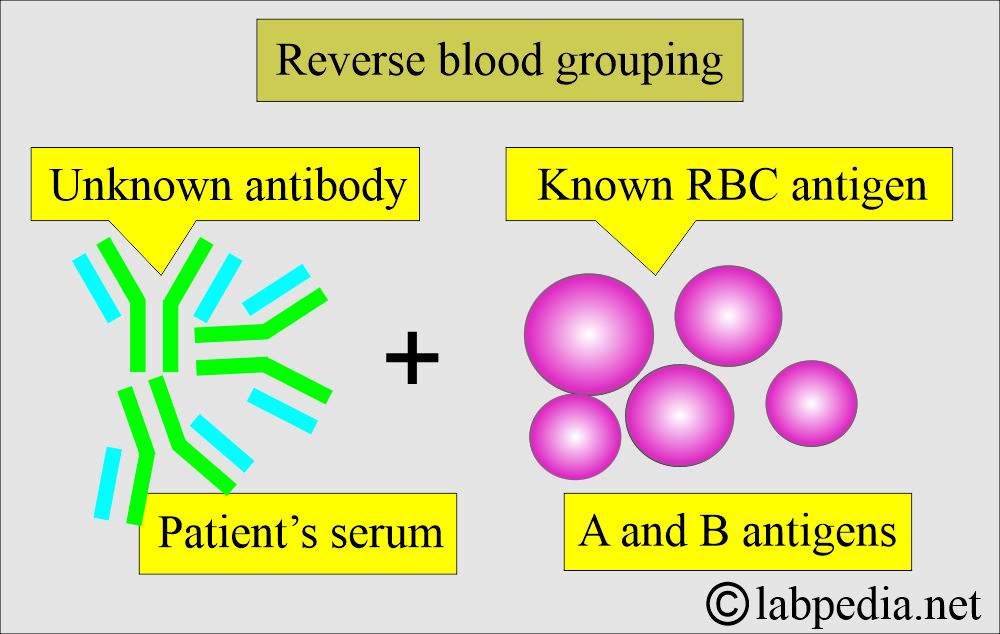
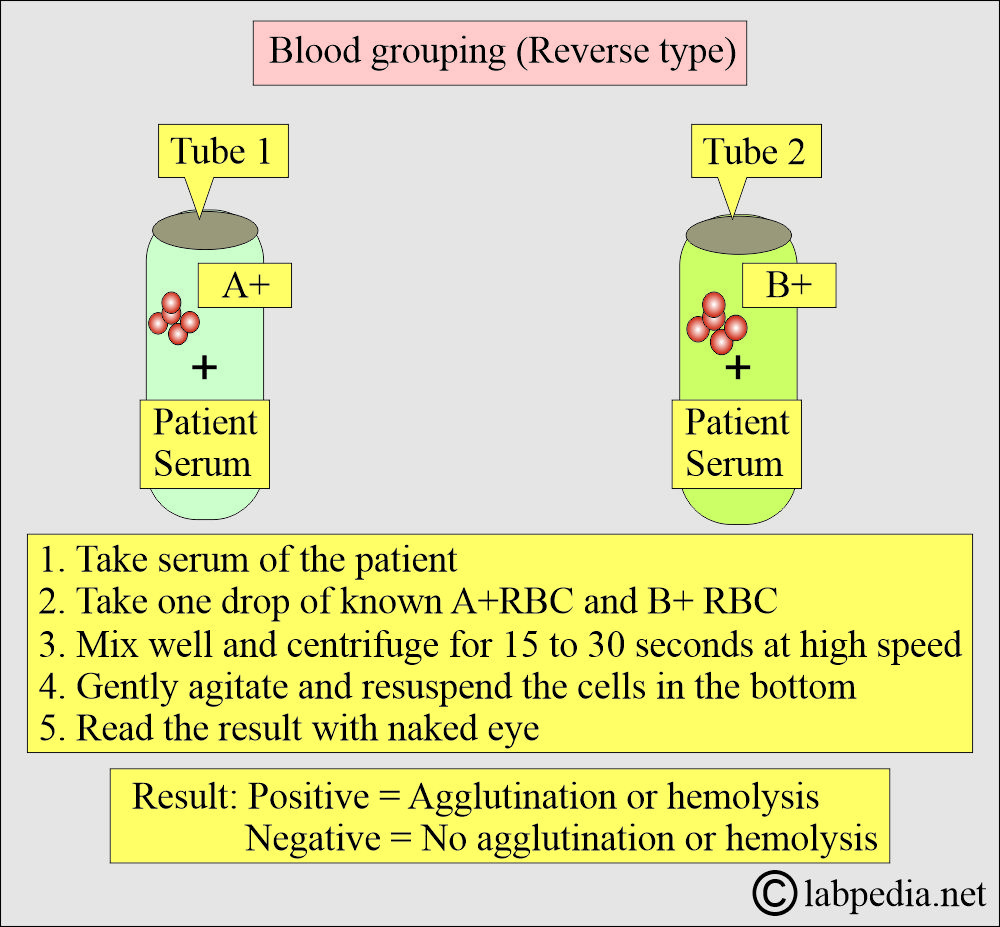
What is Reverse grouping?
- It is defined as using the reagent cells with known ABO antigens and testing the patient’s serum for ABO group antibodies.
- The RBC suspension was mixed with the serum.
- He found agglutination in some and, while in others, no agglutination.
- He concluded that RBCs possess antigens that react with the corresponding antibody in the serum.
- He postulated that there are three blood groups.
- Land Steiner described blood groups A, B, and O.
- His pupils, Von Decastello and Sturle, discovered the fourth blood group, blood group AB, in 1902.
What are the possibilities of the Forward blood grouping?
| Patient’s RBC | Reaction with anti-A | Reaction with anti-B | Blood group |
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
What are the possibilities of Reverse blood grouping?
| Patient’s serum | Reaction with A1 cells | Reaction with B cells | Blood group |
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
What are the Blood grouping procedures?
- Establishing an individual’s blood group requires both forward and reverse grouping.
- Forward grouping antisera source:
- In this case, human sera are needed. This serum is collected from individuals with a very high antibody titer.
- Anti-A is from blood group B, anti-B is from blood group A, and anti-A and anti-B are from blood group O individuals.
- Reverse grouping RBC source:
- RBCs for the reverse grouping are also from the human source of the A and B groups.
- A1 and A2 RBCs can be used, but A1 is sufficient in most routine procedures.
How will you perform the Slide or tile method?
- In this procedure, known antibodies and unknown antigens are used.
- This is elaborated in the following diagram.
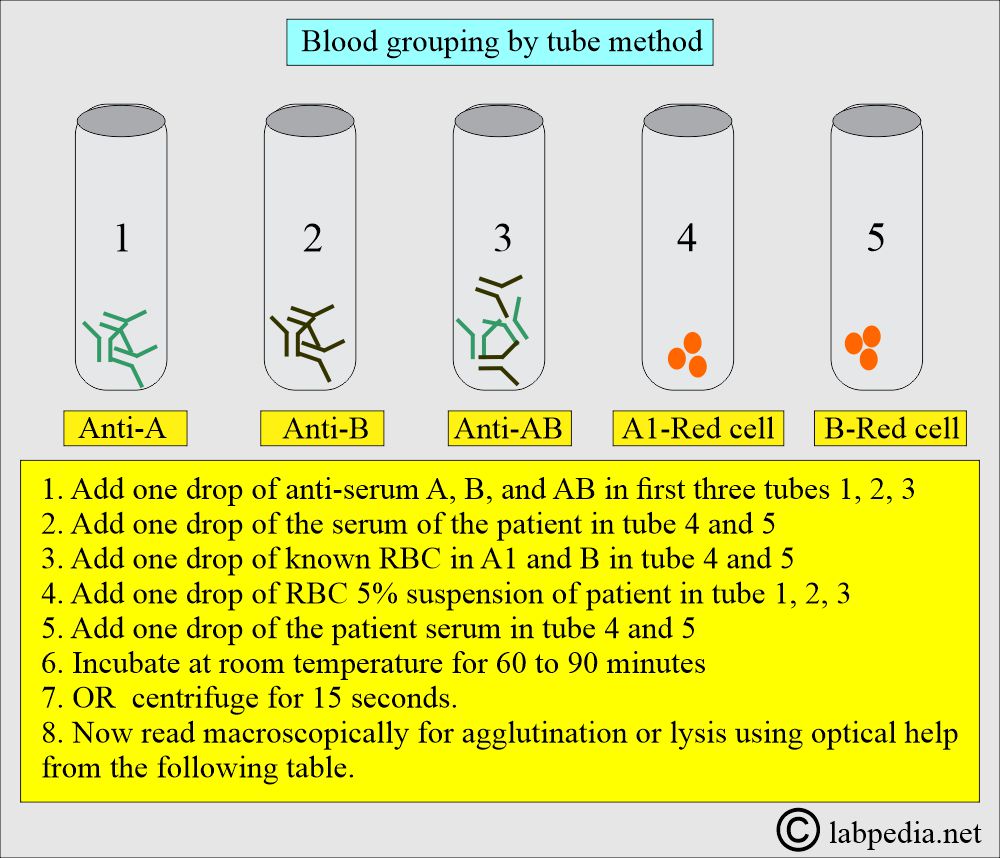
How will you perform the Tube method for blood grouping?
- Put five test tubes on the rack.
- Follow the instructions outlined in the diagram below, and the interpretation is presented in the accompanying table.
How will you interpret the Blood grouping tube method?
| Tube 1 | Tube 2 | Tube 3 | Tube 4 | Tube 5 | Blood group |
| anti-A | anti-B | anti-AB | A1- red blood cells | B-red blood cells | |
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
What are the possibilities of False results in ABO blood grouping?
Procedural mistakes are:
- In the case of dirty glassware.
- If there is an improper cell-to-serum ratio, it will give a false-positive or false-negative result.
- If reagents are contaminated or expired, they will give a false-positive result.
- If you do over-centrifugation, it will give a false-positive result.
- If you do it under centrifugation, it will give a false-negative result.
- If you miss the hemolysis, a positive result will change into a negative result.
- If you do careless reading, the result will be interpreted as a negative one.
- The optical aid may be read as a false-negative result if it is not used.
- Inaccurate identification of the sample or the reagents will give false-positive or false-negative results.
- In the case of an incorrect reading of the results, the interpretation will give false-positive or false-negative results.
What are other possible causes of false-positive results?
- Antibody-coated RBCs in the patient may agglutinate in a medium with high protein content.
- Ask about the history of the recent blood transfusion, which may have introduced a mixture of cell types, resulting in a mixed cell appearance during testing.
- A or B is expressed weakly if there is an unusual genotype antigen.
- Blood groups A2B and A3B may react weakly with reagents anti-sera anti-A. If anti-A1 is present, the sample may be misdiagnosed as Blood group B. Sera from the sample thought group B should be tested with red blood cells A1 and A2 to differentiate with anti-A1, but no anti-A in their serum.
- May get false results in diseases like acute leukemia or non-malignant hemolytic disorder. In these cases, the ABO antigens are weak.
- RBCs may have genetic abnormalities or acquired surface abnormalities that make them polyagglutinable.
- Gram-negative bacteria may give group B-like activity.
- High levels of proteins and fibrinogen may cause rouleux formation, which may be mistaken as agglutination.
- There are blood group-specific substances in high concentration under certain conditions, as seen in ovarian cysts, which may neutralize the anti-A and anti-B antibodies when unwashed RBCs are used.
- Unwashed RBCs in the case of multiple myeloma may give false-positive results because of rouleux formation.
- Drugs like dextran and contrast media may cause cellular aggregation and look like agglutination.
- There is the effect of age, e.g.
- Newborns who have not yet developed antibodies. They may have the antibodies from the mother.
- Older adults may not have strong enough antibody levels.
It is advisable to follow the rules strictly to avoid these mistakes; otherwise, it will put you at risk.
What are the Blood groups, Genotypes, and phenotypes of the baby?
Rh system:
What is the history of the Rh system?
- The Rh system is second in importance to the ABO system.
- In 1939, Levine and Stetson discovered an unusual agglutinin in the serum of a stillborn fetus’s mother that agglutinated 80% of random ABO-compatible donors.
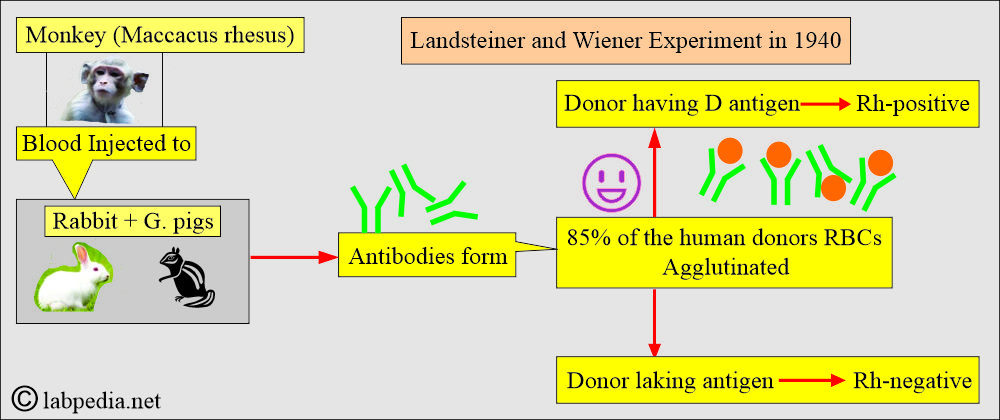
- In 1940, Landsteiner and Weiner injected Blood from the monkey Maccacus rhesus into rabbits and guinea pigs, which resulted in the production of antibodies. These antibodies agglutinated RBCs of around 85% of human donors.
- These two antibodies were the same.
- The person who possessed the corresponding antigens was called Rh-positive.
- The person who lacked the antigens was called Rh-negative.
- The rabbit anti-rhesus was named anti-LW after Landsteiner and Weiner.
- The human antibodies are named the same as anti-Rh.
- The Rh system consists of two allelic genes:
- RhD
- RhCE
- Basically, there are 6 antigens and 6 corresponding antibodies:
- The anti-d antibody does not exist, so the existence of the antigen-d is also disputed.
- Factors C, D, E, and e are all antigenic proteins.
- These antigens will elicit antibodies in individuals whose RBCs are exposed to them.
What are the Rh-system components?
| Antigen | Antibody |
|
|
|
|
|
|
|
|
|
|
|
|
- This gene complex R or CDe is directly passed on from generation to generation.
- An individual who is R r = CDe/cde will pass either R (CDe) or r (cde) to his/her generation.
How will you compare the Fischer-Race and Wiener gene theory?
| Wiener gene Agglutinogen | Fisher-Race gene Agglutinogen |
| r rh | cde c, d, e |
| r’ rh’ | Cde C,d,e |
| r” rh” | cdE c,d, E |
| ry rhz | CdE C,d, E |
| R° Rh0 | cDe c, D,e |
| R1 Rh1 | CDe C, D,e |
| R2 Rh2 | cDE c, D, E |
| Rz Rhz | CDE C, D,E |
- The Rh system is assigned to chromosome number 1.
- These will encode the membrane proteins that carry:
- Antigen D.
- Antigen Cc.
- Antigen Ee.
- The weak expression of antigen D, Du, is also important in blood banking.
- Approximately 1% of D-positive individuals are of the weak D-antigen type, known as Du, characterized by weak or absent RBC agglutination by anti-D antibodies during serologic testing.
- In these individuals, the weak D antigen (Du) will only be detected by the anti-human globulin (Coombs test) reagent.
- The RhD gene may be either present or absent. So phenotypically, the possibilities are:
- RhD positive (RhD+).
- RhD negative (RhD–).
What are the Rh-Antibodies?
- Rh-antibody rarely occurs naturally due to immune stimulation resulting from previous transfusion or pregnancy.
- Most of the clinical issues are due to the RhD-antibody.
- Anti-C, anti-c, anti-E, and anti-e are occasionally seen, and both may cause transfusion reactions and the newborn’s hemolytic disease.
What are Rh nomenclature systems?
- The most commonly used is Fischer-Race is the CDE system.
| Fisher-Race CDE system | Wiener Rh system | Rosenfield et al. system |
| Antigen | Antigen | Antigen |
| D | Rho | Rh1 |
| C | rh´ | Rh2 |
| E | rh´´ | Rh3 |
| d | Hr | Rh4 |
| c | hr´ | Rh5 |
| e | hr´´ |
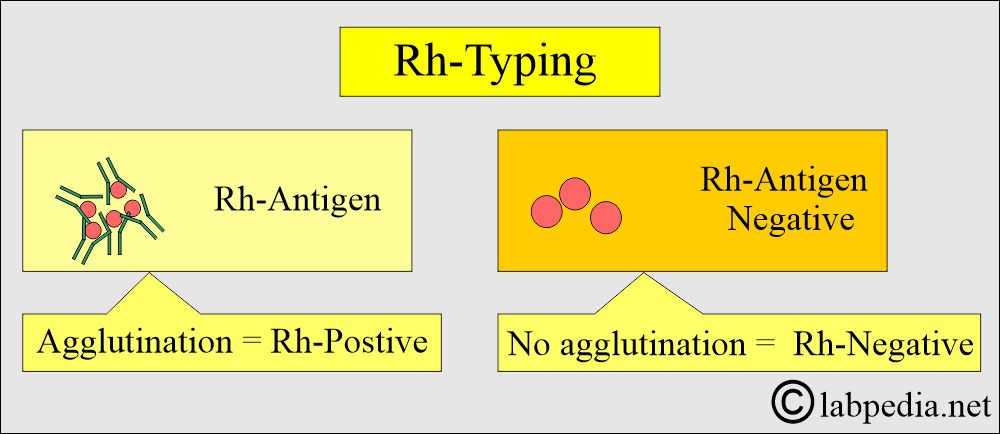
How will you discuss the Rh-positive and Rh-negative groups?
- The presence of the Rh antigen on the surface of RBC is called the Rh-positive group, and the absence of the Rh antigen is called the Rh-negative group.
- Individuals whose RBCs contain the D antigen (Rh0) are either D/D or D/d and are referred to as Rh-positive. The Rh-positive group represents 85% of the population.
- The D (Rh0) antigen is the strongest antigen, leading to immunization if introduced to someone else.
- So, Rh-positive means the presence of D-antigen and is unrelated to other Rh factors.
- It is necessary to check for the D-antigen before administering a blood transfusion.
- Always avoid Rh-positive blood transfusions into an Rh-negative person. If this is done by mistake, there is an 80% chance of the transfused person developing anti-D antibodies.
- The first transfusion may not cause a problem in such cases, but it can lead to a blood transfusion reaction in subsequent transfusions.
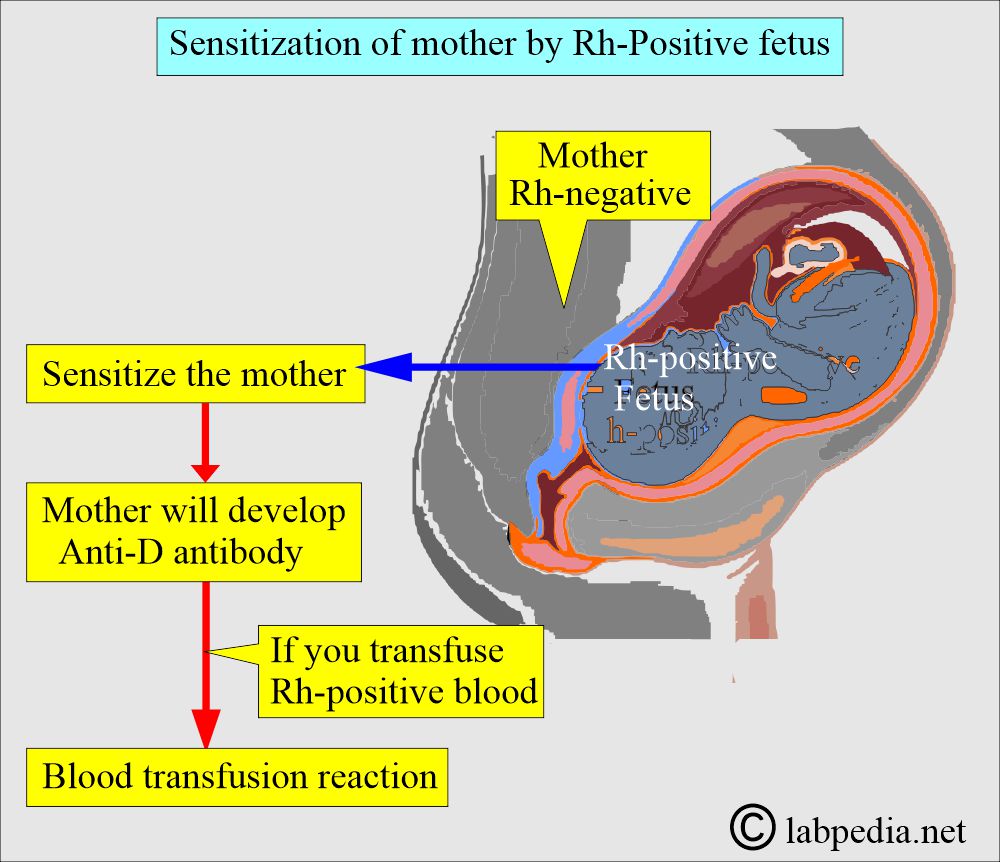
Can the Rh-positive fetus sensitize the Rh-negative mother?
- The first-time exposure to the Rh-D antigen will sensitize the mother’s immune system.
- Later on, if given Rh-positive blood, in that case, the mother will develop a blood transfusion reaction.
- The individual whose RBCs lack the D antigen (Rh0) is called the Rh-negative group, which is 15% of the population.
- Most of the Rh-negative persons are cde/cde; this genotype is truly an Rh-negative individual.
- All pregnant mothers should have blood typing and Rh factor typing.
- In the case of the Rh-negative mother, it should determine the father’s blood group.
If the father is Rh-positive, perform an indirect Coombs test on the mother’s serum.
- The Coombs test is repeated at 28, 30, and 38 weeks of gestation.
- If all tests are negative, then the fetus is not at risk.
- If these tests are positive, the fetus is at risk and may develop hemolytic anemia (Erythroblastosis fetalis).
- When the mother is Rh-negative and the fetus is Rh-positive, the mother may be sensitized at delivery due to feto-maternal blood mixing.
- The mother’s sensitization can be prevented by administering RhoGAM, Rh Immunoglobulin, which neutralizes the Rh antigen.
- RhoGAM prevents future pregnancy from hemolytic anemia.
- Rh-negative blood groups can develop Rh-antibodies when exposed to Rh-positive blood because of blood transfusions or feto-maternal blood mixing.
How will you perform Rh-Typing?
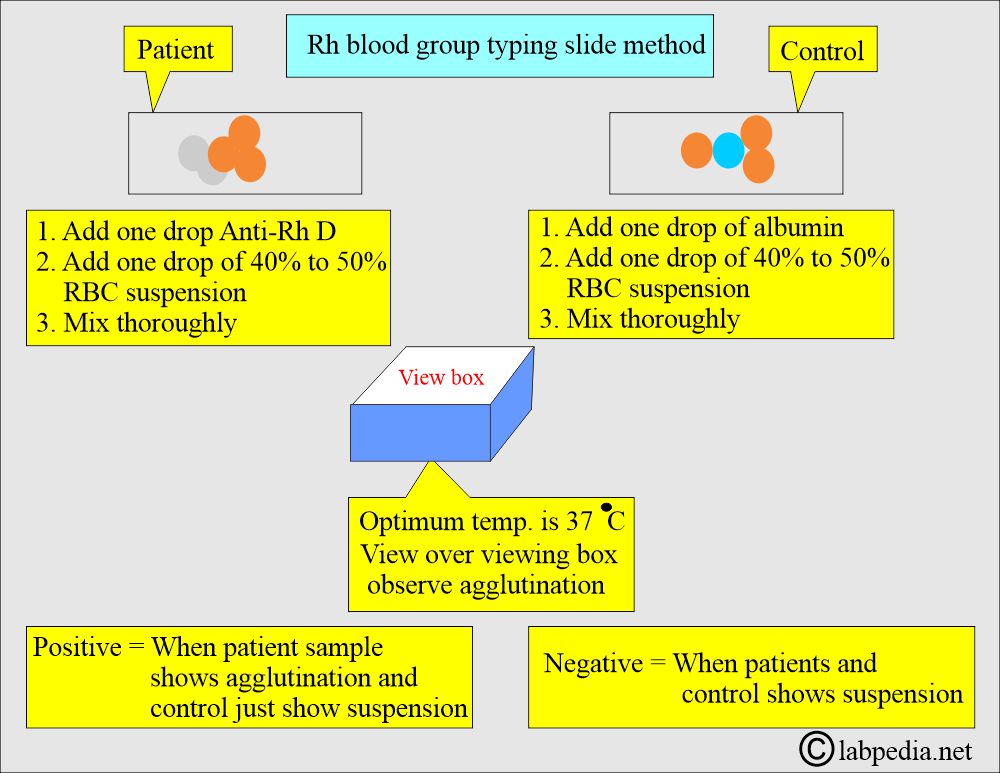
How will you perform the slide method?
- The slide method is easy to perform.
- This method is described diagrammatically.
What are the possibilities of a False-positive result in the slide method?
- In the case of drying the slide, it may mimic agglutination.
- Rule out the presence of microclots, and these may mimic agglutination.
- Inadequate amount of the anticoagulant.
What are the possibilities of a false-negative result in the slide method?
- A saline suspension of the RBCs may react poorly or yield a weak reaction.
- In the case of anemic patients, there may be fewer RBCs to be tested.
- Reading the result in less than 2 minutes may yield a false result in cases of weak RBCs.
- If you use the wrong reagents.
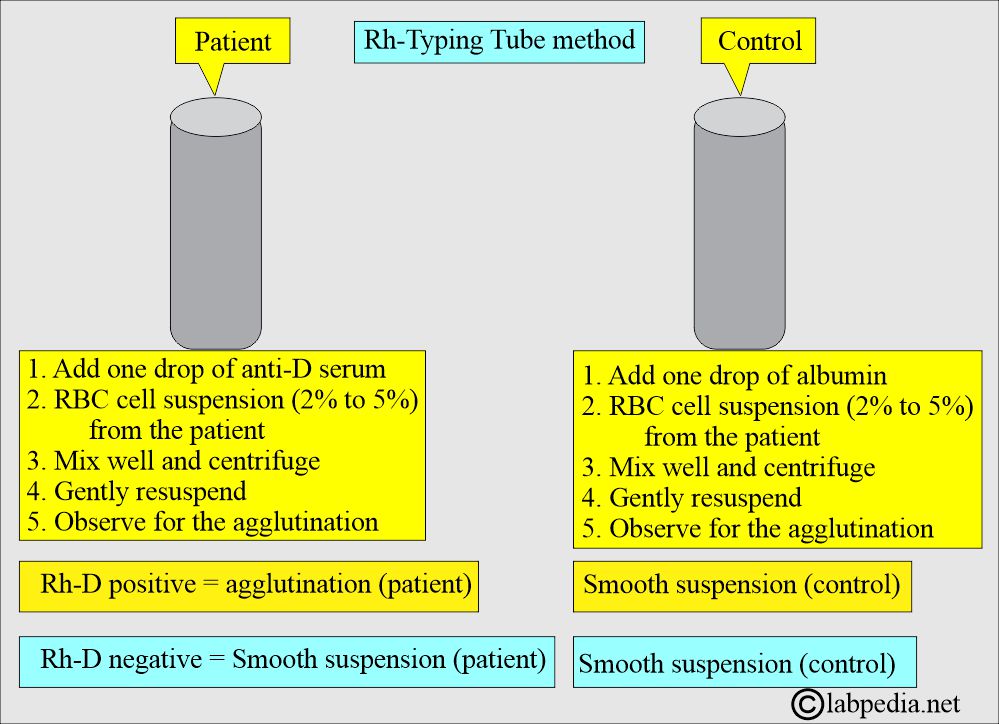
How will you perform the Tube method for Rh-Typing?
- The tube method is more accurate than the slide method.
- This method is described diagrammatically.
What are the possibilities of False-positive results in the tube method?
- If you keep serum and RBCs for a long time, you may see false agglutination, which is essentially rouleaux formation due to the high protein medium.
- The anti-Rho (D) serum may contain other antibodies with different specificities.
- If there are contaminating antibodies with a specificity other than indicated in the literature.
- If there are polyagglutinable RBCs that may agglutinate with any serum protein reagents.
- In case the patient has abnormal proteins in the serum.
What are the possibilities of a False-negative result in the tube method?
- In the case of improper reagents used in the test.
- If serum and cells are left for a long time, they will give rise to rouleaux formation, which may be mistaken for agglutination.
- RBCs with variant antigens, e.g., Cw, ces, may fail to react with standard reagents.
What are the clinically significant blood groups?
| Blood group system | Presence of antibody | Possibility of transfusion reaction | Hemolytic episodes in newborns |
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
Questions and answers:
Question 1: In case of Rh-negative mother, can the first pregnancy give a hemolytic reaction?
Question 2: Do H substances exist in tears?


great reference guide
Thanks a lot for encouraging remarks.
Great content!! May i please use your work as reference for a class presentation?
Thanks for the comment. You can use my website for teaching .
Thanks a lot for the comments.
Dear Prof Riaz,
Thank you for this wonderful reference and guide. With your permission, I would like to use some components of this work, to curate a in-laboratory algorithm based tool to, assist the naive medical technologist (and perhaps even junior physicians) in the investigation of ABO discrepancies.
Warmest regards
Omar
Dear Omar
I have sent you email, please reply to that. Thanks for your comments.
Hi Dr. Riaz are you the author?
You are right. I am the author, and this is my hobby in my retired life.
Hi prof. Riaz, thank you for this wonderful piece of knowledge, i will like to have a copy of this through email if possible.
regards
Mustapha Omar
Thanks for the comments. I think you can follow the topic from my website.
Good afternoon
From where you are Sir ?
If From India Kindly send your contact no.
Thanks for the contact. I live in the USA. I will be glad to reply to your queries.
Greetings! Can i get your references, sir?
You are welcome.
I am using references and these are in consolidated form.
Please email me the references.
this website is the best and goodies and i think he is website goodies in the world an thank you so much sir !!!!!!
Thanks a lot.
can you give more explanation about anti-human globulin
Please see this link:
https://labpedia.net/coombs-test-part-1-coombs-direct-direct-anti/
helped a lot in my project work. thank you.
This is honor for me, if labpedia.net helped in your work. You are welcome.