TORCH Profile:- Part 4 – Toxoplasmosis (Toxoplasma gondii)
Toxoplasmosis
The sample for the TORCH profile
- Venous blood is collected to prepare the serum.
- The other sample used is blood, urine, and spinal fluid for evidence of the infections for TORCH.
- Diagnosis can be confirmed by the culture of one of the specific pathogens or by increased levels of IgM against the specific pathogen.
Purpose of the test (Indications)
- TORCH profile is done to find the cause of premature birth or abortion.
- TORCH is used to screen infants for infections such as toxoplasmosis, cytomegalovirus, herpes simplex, rubella, and syphilis.
Pathophysiology of TORCH
- TORCH profile includes the following tests :
- Toxoplasmosis antibody.
- Rubella antibody.
- Herpes Simplex.
- Cytomegalovirus
- some people include syphilis as well.
- These infections may lead to birth defects, growth delay, and brain and nervous system problems in the baby.
- If TORCH screening on infants is positive, more testing will be needed to confirm the diagnosis. The mother will also need to be checked.
- The test is ordered when a pregnant woman is suspected of having any of the TORCH infections.
- These infections can be serious during pregnancy because they can cross the placenta from the mother to the developing fetus and cause congenital defects in the newborn.
- The TORCH infections cause a syndrome characterized by:
- Microcephaly.
- Sensorineural deafness.
- Chorioretinitis.
- Hepatosplenomegaly.
- Thrombocytopenia.
- TORCH infection signs/symptoms are :
- Fever and poor feeding.
- The newborn is often small for gestational age.
- A petechial rash on the skin may be present, with small reddish or purplish spots due to bleeding from capillaries under the skin.
- An enlarged liver and spleen (hepatosplenomegaly) are common, and jaundice.
- Hearing impairment, eye problems, mental retardation, autism, and death can be caused by TORCH infections.
- The mother often has a mild infection with few or no symptoms.
- The examiner may test blood, urine, and spinal fluid for evidence of the infections for TORCH.
- Diagnosis can be confirmed by the culture of one of the specific pathogens or by increased levels of IgM against the pathogen.
Toxoplasmosis (Toxoplasma Gondii)
Sample for Toxoplasmosis
- Blood to prepare the serum.
- Store the blood at 2 °C to 6 °C if the test is delayed for over 7 days.
- Serum should not be heat-inactivated because this may give false-positive results.
- This protozoan is a parasite of warm-blooded animals.
Definition of Toxoplasmosis:
- Toxoplasmosis is caused by a protozoan parasite Toxoplasma Gondii.
- Protozoan parasites are unicellular and eukaryotic.
Epidemiology of Toxoplasmosis:
- Antibody to T.gondii varies in different populations. It ranges from 96% in Western Europe to 10 to 40% in the united states of America.
- The patients with AIDs are seropositive for T. gondii, and roughly 25% to 50% will develop encephalitis.
- This is a protozoan that is present in all warm-blood animals.
- The Toxoplasma gondii was first discovered in North African rodents and has been observed in numerous birds and mammals around the world, including humans.
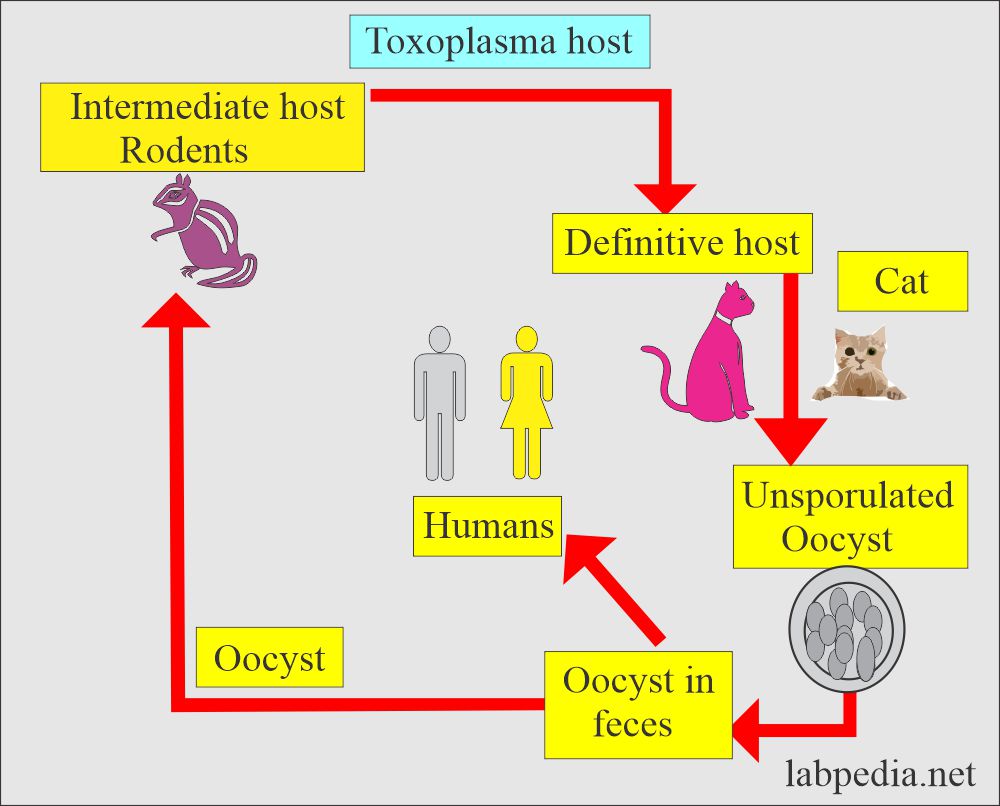
- The cat is the definitive host.
- Toxoplasma gondii is the most common causative agent of toxoplasmosis.
- This is found worldwide because so many animals harbor it.
- 15% to 20% of the American population has this infection.
- The highest record, 93%, is found in Parisian females who eat undercooked or raw meat, and 50% of cases are seen in their children.
- A number of babies are infected through the transplacental route.
- This is also seen in the USA due to undercooked meat.
- Oocyst is hardy and can survive for a longer period.
- These organisms have no flagella.
The life cycle of Toxoplasma Gondii
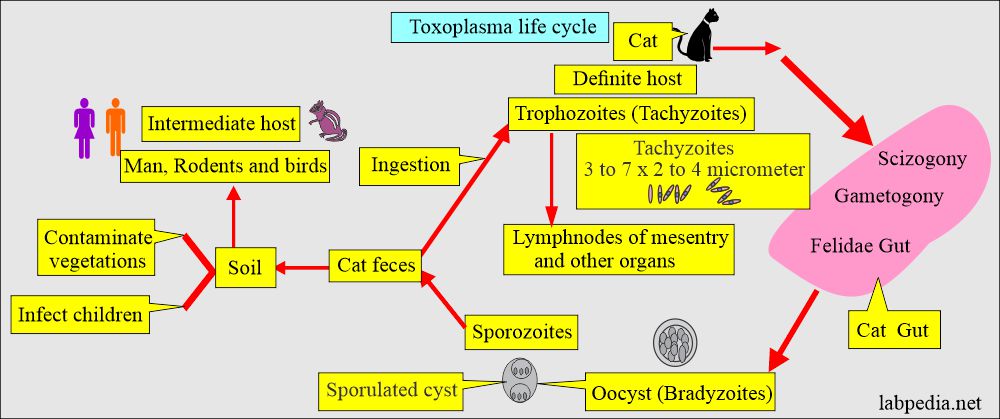
- Toxoplasma has a complete life cycle as coccidian in the filedae (carnivorous animals including cats and big cats).
- The definitive host:
- These are the house cats. Cats are the only definitive host.
- Domestic cats are the source of the disease because the oocysts are often present in their feces.
- Oocysts can survive in the soil for over a year.
- It can lead to infecting humans from the cat litter box that contains oocysts in the stool.
- In the cat, the parasite develops a sexual cycle, and oocysts are eventually excreted in the feces.
- Trophozoites are crescent-shaped and can spread in the cat’s organs and tissues.
- Later on, these develop into cysts.
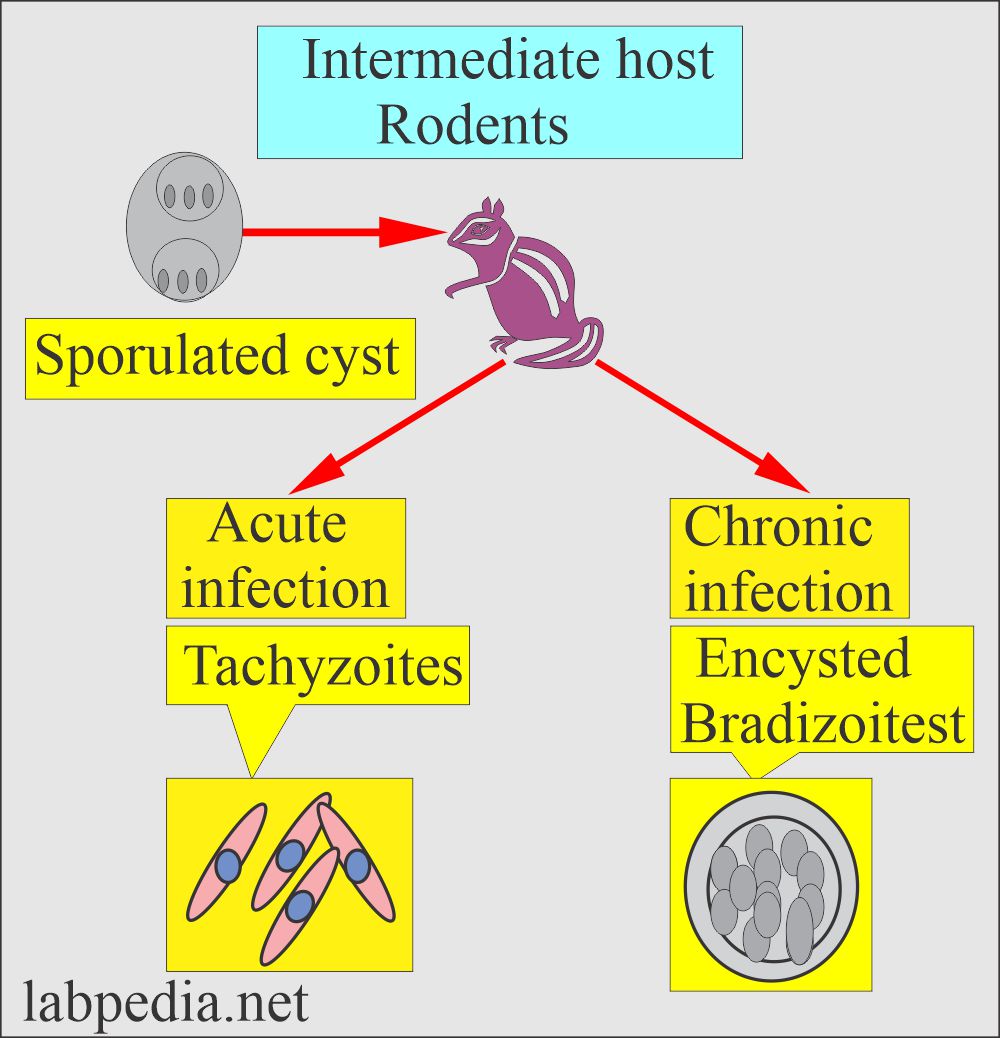
- The intermediate host:
- The intermediate host is a rat and a man.
- After ingestion, the parasite, which is an obligate intracellular organism, spreads widely via blood circulation.
- The ingested oocyst will encyst in various organs like muscles and remain dormant for many years or for the life of the host.
- Cysts may form in the brain, muscles, and eye.
Source of spread:
- Humans may acquire the disease by ingesting uncooked meat and contaminated material.
- There may be fecal contamination of:
- Food.
- Water.
- Soiled hands.
- Inadequate cooked or infected meat.
- Raw milk.
- Blood transfusion transmission of toxoplasmosis has been recently recognized, particularly with white blood cell concentrate.
- Patients at risk are those receiving immunosuppressive agents or corticosteroids.
- Exposure to feces of cats or other infected material.
- Toxoplasma Gondii spread due to:
- Hand-to-mouth contamination of infected oocyst in cat feces.
- Ingesting contaminated meat.
- Transplacental spread during delivery.
- Transplacental transmission usually takes place in the course of an acute or undiagnosed maternal infection.
- The expected incidence of congenital toxoplasmosis is 2.7 per 1000 live births.
Disease pattern of Toxoplasmosis:
- After ingesting the cysts, this protozoan is an obligatory intracellular parasite.
- This will spread through the blood, and cysts may form in the brain and muscles.
- These cysts may be seen in the eye.
- A congenital infection that shows:
- Hydrocephalus or microcephaly.
- Encephalomyelitis.
- Chorioretinitis.
- Cerebral calcification.
- There are lesions in the viscera.
- There may be acute enlargement of the lymph nodes.
- Severe illness leads to Myocarditis, Pneumonitis, Hepatitis, Meningoencephalitis, and ocular lesions.
- Types of toxoplasmosis are:
- Congenital toxoplasmosis.
- Cerebral toxoplasmosis.
- Toxoplasmosis in the immunocompromised patients.
- Cerebrospinal fluid is abnormal in 2/3 of the cases, showing positive xanthochromia, and raised protein levels.
Clinical presentation (Signs and Symptoms):
Primary infection:
- Many patients may remain asymptomatic, especially children.
- Later on, this results in generalized infection:
- The patient may have fatigue, and the initial presentation is an enlargement of the lymph nodes,
- Patients may have chills and fever.
- The Patient may have a headache and myalgia.
- Chronic cases may develop a maculopapular rash.
- Severe symptoms may be seen in patients with encephalomyelitis, myocarditis, or hepatitis.
- Spontaneous recovery follows acute febrile disease; the organism can localize and multiply in any organ of the body or circulatory system.
- Types of T.gondii infections are:
Acquired infection.
- This is frequently mild.
- Chills, fever, headache, enlarged lymph nodes, and extreme fatigue exist.
- A chronic form of toxoplasmic lymphadenopathy may exist.
- Reactivation of cerebral toxoplasmosis may be seen in AID patients.
- In AID patients, encephalitis is seen. In these patients, CD4+ cell numbers fall below 100 x 109/L.
Congenital infection:
- The Toxoplasma parasite is transferred to the fetus through the placenta, where the mother acquires active infection near the time of conception or during the pregnancy.
- Mothers, during the first trimester, infect 14% of the fetuses.
- During the second trimester, involve 29% of the fetuses.
- During the third trimester, it reaches 59% of the fetuses.
- About 90% of the ladies acutely infected are asymptomatic.
- Unlike toxoplasmosis in later life, it is very severe in these patients.
- It results in central nervous system malformation.
- There may be prenatal mortality.
- Typically these patients present with the following:
- Cerebral calcificationion.
- Chorioretinitis.
- Hydrocephalus or microcephaly.
- Infants who are serologically positive at birth may fail to display the following:
- Neurological abnormalities.
- Ophthalmic abnormalities.
- Generalized illness at birth.
- 75% of the cases of a congenitally infected newborn are not seropositive or not diagnosed at birth:
- The disease remains dormant.
- Or discover when the patients will develop:
- Chorioretinitis.
- Unilateral blindness.
- Neurological abnormalities.
- Congenitally infected babies also have general S/S like:
- Fever.
- Rashes.
- Jaundice.
- Hepatosplenomegaly.
- Acquired infection during pregnancy (in-utero) may lead to abortion or stillbirth.
- Late complications are:
- Chorioretinitis.
- There may be mental retardation.
- Palsy.
- Deafness.
- Serological findings for congenital toxoplasmosis:
- Raised level of IgM supports the congenital infection. There are other conditions to give IgM response.
- So raised levels of IFA-IgG support the diagnosis of toxoplasmosis.
- The rising titer of IgG is important to confirm the diagnosis to avoid maternal IgG antibodies.
Complications of congenital toxoplasmosis:
- Hydrocephalus.
- Microcephaly.
- Chronic retinitis.
- Convulsion.
How to prevent congenital toxoplasmosis:
- Avoid touching the mucous membrane of the mouth and eye while handling raw meat.
- Wash hands thoroughly after handling raw meat.
- Cook the meat at >66 °C.
- Wash the kitchen surfaces that come in contact with the raw meat.
- Wash the fruits and vegetables thoroughly before eating.
- Prevent access to flies, cockroaches, and other insects to vegetables and fruits.
- Avoid contact or wear gloves when handling cat feces-contaminated materials.
Interpretation of the serological tests in pregnant women:
| IgG antibody | IgM antibody | Interpretations of the serological test |
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
Diagnosis of Toxoplasmosis:
The culture:
- Often the culture of T. gondii is very difficult, so the diagnosis is supported by the serology.
Biopsy of the lymph nodes:
- Lymph node biopsy is suggestive by the small histiocyte groups involving the germinal centers.
- This pattern is not specific for the confirmation of toxoplasmosis.
- The presence of the organism is rarely seen in the lymph node.
Serology of Toxoplasmosis:
- Serologic tests make the backbone of the diagnosis of toxoplasmosis.
- The enzyme-linked immunofluorescent assay (EIA) is the method of choice for detecting IgM, indicating acute infection.
- The various methods or techniques used for T. gondii antibody are:
- Enzyme-linked immunoassay (EIA).
- Indirect hemagglutination (IHA).
- Indirect fluorescent antibody (IFA).
- Sabin-Feldman dye test. It is a methylene blue dye test.
- This dye test requires living toxoplasma organisms.
- Complement fixation test.
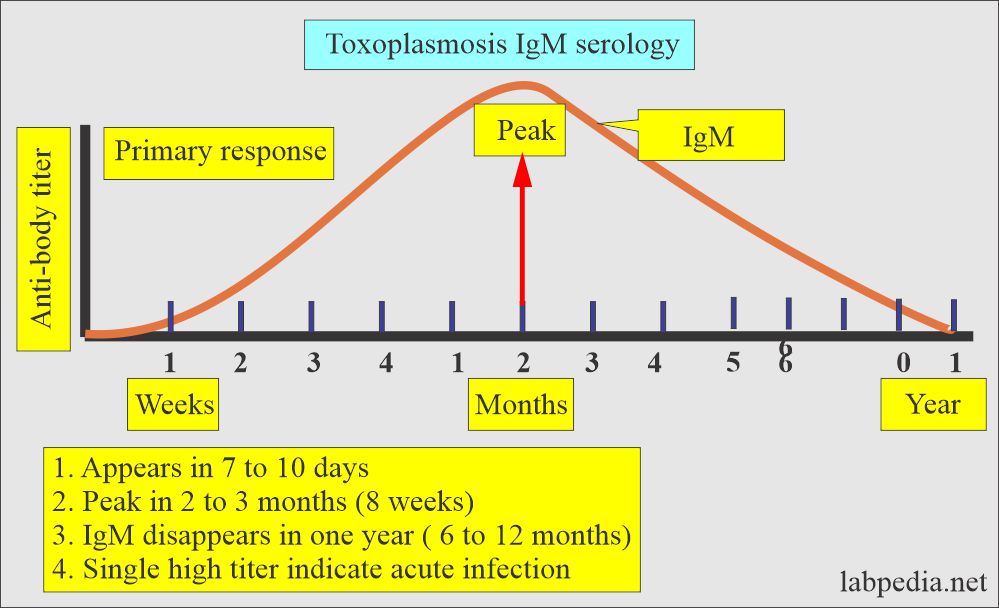
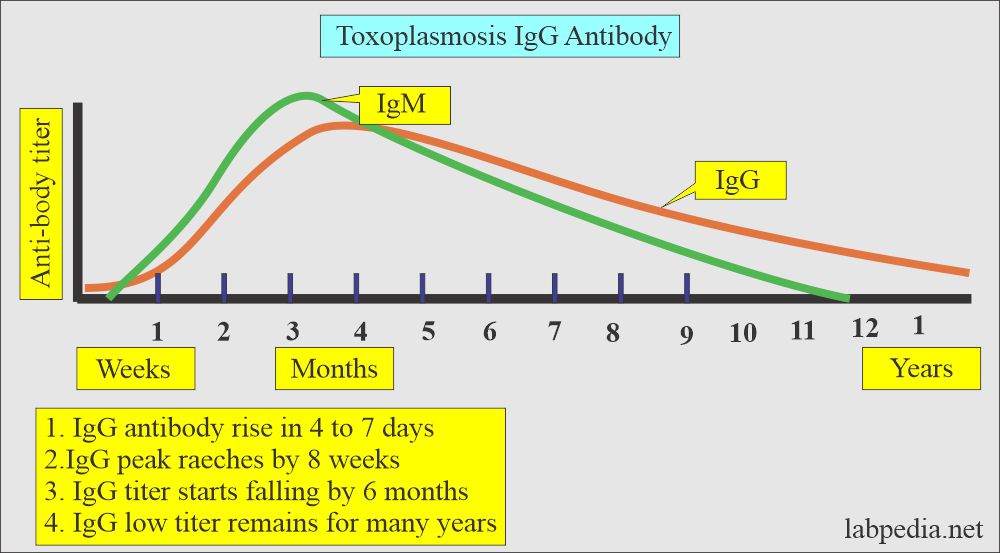
- IgM:
- It starts rising about 7 to 10 days after the infection.
- The peak level reaches around 8 weeks (the range is 4 to 10 weeks).
- It becomes nondetectable by 6 to 12 months after infection.
- IgM antibody is needed to confirm the present infection.
- Antibody IgM titer <1:16 = shows no exposure to the virus.
- Antibody IgM titer >1:4 to 1:256 = acquired infection in last 18 months.
- Antibody IgM >1: 1024 = Acquired infection in last 4 months.
- IgG:
- IgG antibody starts rising about 4 to 7 days after the infection.
- IgG reaches peak level in about 8 weeks (range is 4 to 10 weeks).
- It starts falling slowly by 6 months.
- While low titers persist for many years.
- The anti-nuclear antibody may produce a false positive result.
- IgG antibody titer represents present or past infection.
- The rise in the IgG or IgM antibody to toxoplasma is rapid.
- There is a significant rise by the end of the first week.
- ELISA and agglutination kits are commercially available.
Toxoplasma antibody interpretation:
| IgG antibody | IgM antibody | Interpretations |
| Negative | Negative | Susceptible to infection, take the history of the patient |
| Negative | Positive | Positive for early infection or false positive, so repeat the test |
| Positive | Negative | Past infection 6 months or more |
| Positive | Positive | Positive recent infection within the last 12 months |
Treatment of Toxoplasmosis:
- Most infections are self-limiting.
- Treatment of choice is a combination of Trisulfapyrimidines and Pyrimethamines (Daraprim) needed for chorioretinitis.
- Corticosteroids may be helpful.
Questions and answers:
Question 1: What are best tests for the diagnosis of toxoplasmosis?
Question 2: What is the significance of IgM for the diagnosis of toxoplasmosis?