TORCH Profile:- Part 2 – Cytomegalovirus (CMV)
Cytomegalovirus (CMV)
What sample is needed for the TORCH profile?
- Venous blood is collected to prepare the serum.
- The other samples used are blood, urine, and spinal fluid for evidence of the infections for TORCH.
- Diagnosis can be confirmed by the culture of one of the specific pathogens or by increased levels of IgM against the specific pathogen.
What are the indications for the TORCH profile?
- TORCH profile is done to find the cause of premature birth or abortion.
- TORCH screens infants for toxoplasmosis, cytomegalovirus, herpes simplex, rubella, and syphilis.
What are the tests included in the TORCH profile?
- TORCH profile includes the following tests:
- Toxoplasmosis antibody.
- Rubella antibody.
- Herpes Simplex.
- Cytomegalovirus
- Some people include syphilis as well.
- These infections may lead to birth defects, growth delays, and problems in the baby’s brain and nervous system.
- If TORCH screening on infants is positive, more testing will be needed to confirm the diagnosis. The mother will also need to be checked.
- The test is ordered when a pregnant woman is suspected of having any of the TORCH infections.
- These infections can be serious during pregnancy because they can cross the placenta from the mother to the developing fetus and cause congenital defects in the newborn.
- The TORCH infections cause a syndrome characterized by:
- Microcephaly.
- Sensorineural deafness.
- Chorioretinitis.
- Hepatosplenomegaly.
- Thrombocytopenia.
- TORCH infection signs/symptoms are:
- Fever and poor feeding.
- The newborn is often small for gestational age.
- A petechial rash on the skin may be present, with small reddish or purplish spots due to bleeding from capillaries under the skin.
- An enlarged liver and spleen (hepatosplenomegaly) are common, such as jaundice.
- Hearing impairment, eye problems, mental retardation, autism, and death can be caused by TORCH infections.
- The mother often has a mild infection with few or no symptoms.
- The examiner may test blood, urine, and spinal fluid for evidence of the infections for TORCH.
- Diagnosis can be confirmed by the culture of one of the specific pathogens or by increased levels of IgM against the pathogen.
Cytomegalovirus (CMV)
What sample is needed for Cytomegalovirus (CMV)?
- Culture is the choice of method.
- The patient’s blood is used to get the serum.
- Urine.
- Saliva.
- Biopsy material.
- White blood cells.
What is the History of Cytomegalovirus (CMV)?
- 1904, the first histologic changes characteristic of CMV were published.
- In 1966, the actual isolation of the virus following blood transfusion and raised antibody titer was noted.
- CMV is a DNA virus and a member of the herpesvirus family.
- This is the most common intrauterine infection, affecting 1% of newborns in the United States of America.
- 90% of these babies are asymptomatic at birth.
- Isolation of the CMV from urine or saliva or detecting IgM-CMV antibodies is the marker of congenital infection.
How will you define Cytomegalovirus (CMV)?
- CMV is one of the herpesvirus groups.
- The Herpesvirus group consists of the following:
- Herpes simplex I.
- Herpes simplex II.
- CMV.
- Epstein-Barr virus.
- Varicella-Zoster.
- CMV is a relatively harmless virus, only infecting immunocompromised patients and newborns.
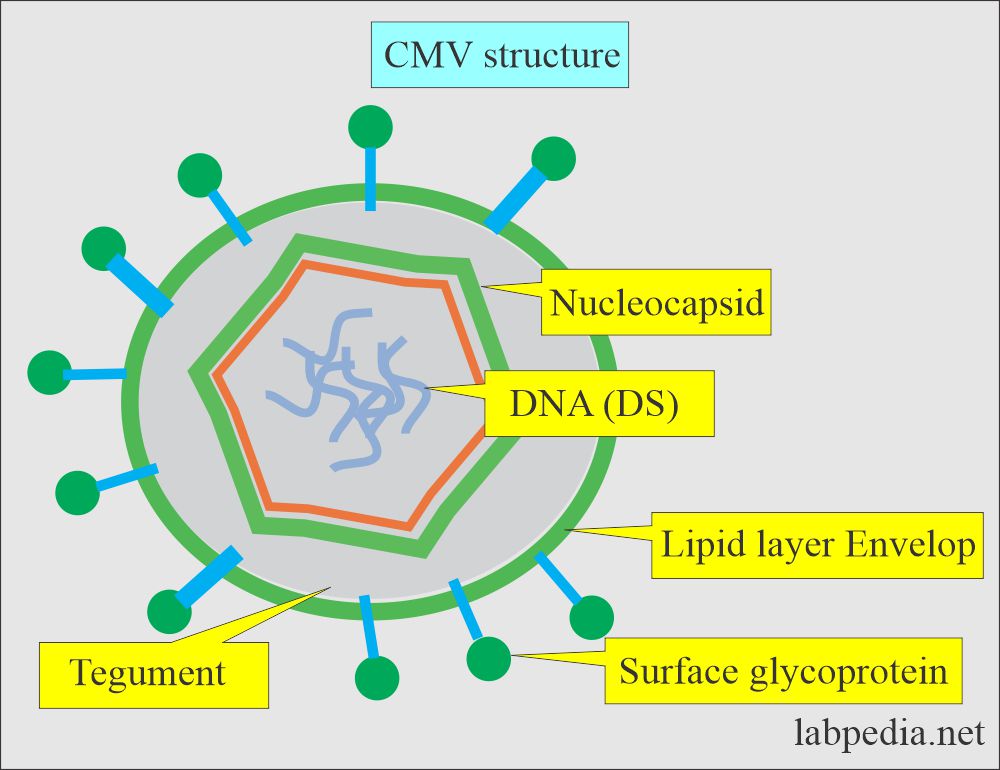
What is the structure of the Cytomegalovirus (CMV)?
- CMV can survive for variable times in the urine, saliva, blood, breast milk, cervical secretions, and semen.
- All these viruses are relatively large, enveloped DNA viruses.
- A central core containing double-stranded DNA.
- It is surrounded by icosahedral capsid.
- A bilayer lipids envelope around the virus is derived from the host cell nuclear membrane.
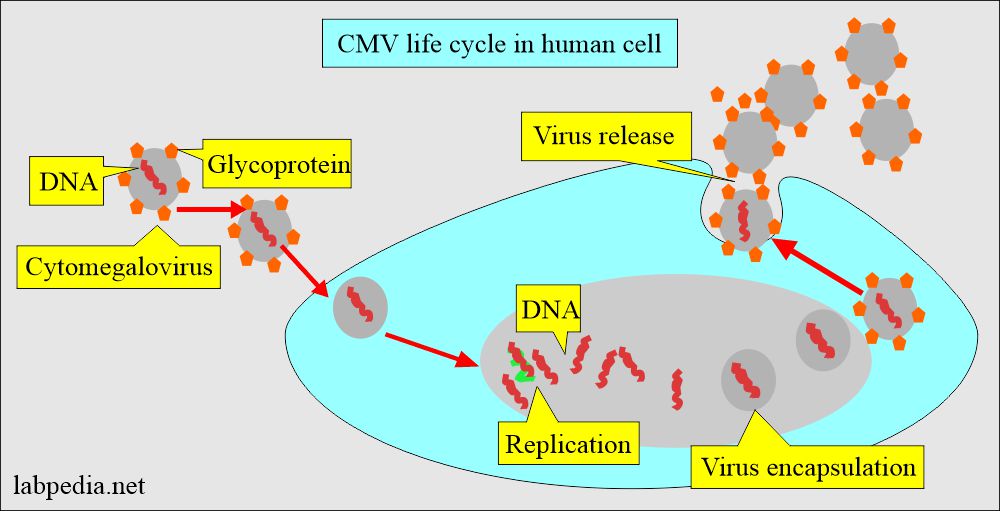
- These DNA viruses undergo a replicative cycle involving DNA expression and nucleocapsid assembly within the nucleus.
- The viral structure gains an envelope when the virus buds through the nuclear membrane, which is altered to contain specific viral proteins.
- All these viruses spread from cell to cell, most likely via intercellular bridges and antibodies in the extracellular phase.
- These viruses produce subclinical infections that can be reactivated under appropriate stimuli.
How will you describe the Epidemiology of Cytomegalovirus (CMV)?
- CMV infection is endemic worldwide.
- CMV infection is widespread because serologic evidence ranges from 30% to >90% in different geographic areas.
- There is a lower incidence in some parts of Western Europe and some of the USA.
- CMV is considered the most important cause of congenital infection in the United States of America.
- Acquired CMV infection is usually asymptomatic and can persist in the host as a chronic or latent disease.
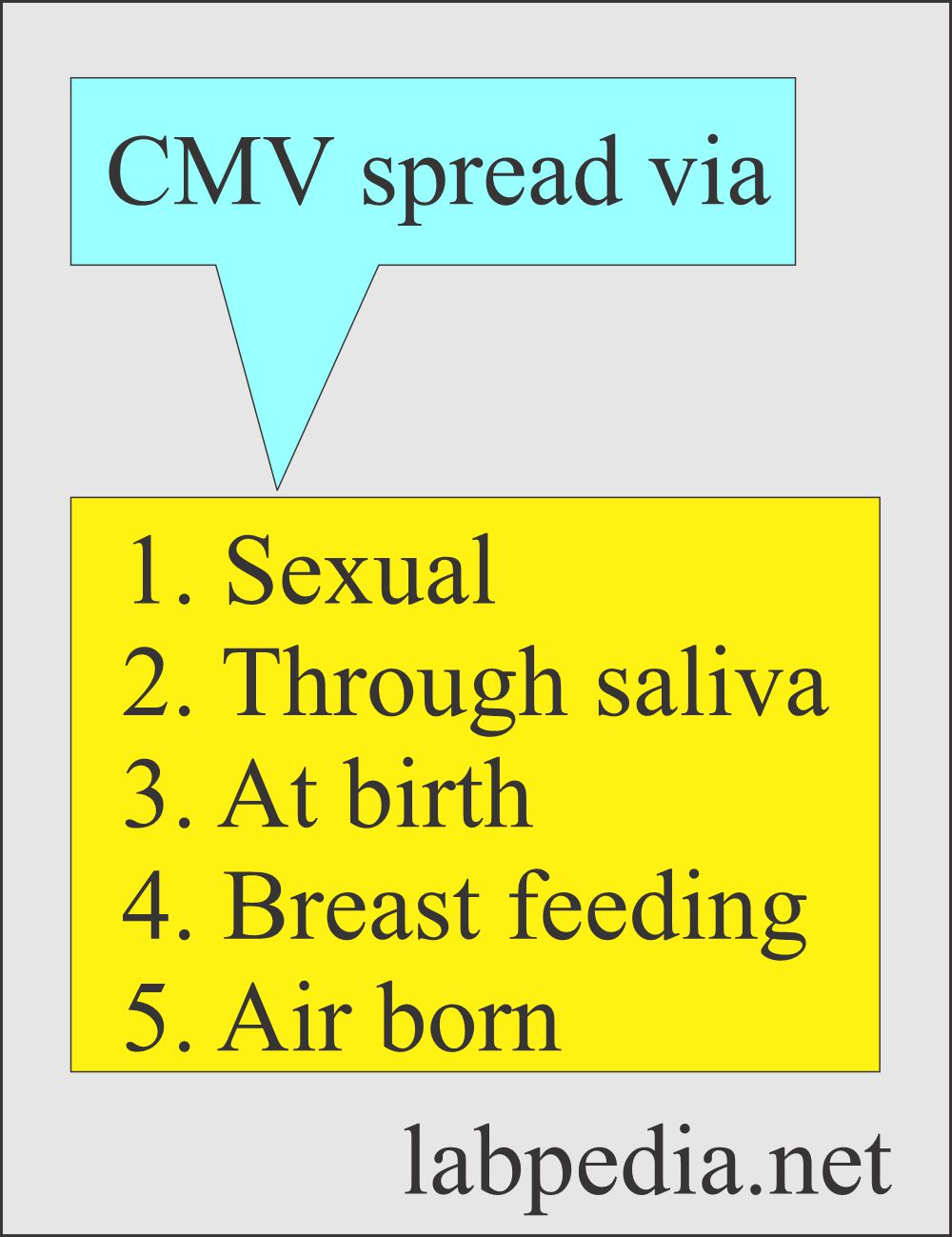
- Dissemination of the virus may be:
- Oral.
- Respiratory.
- Venereal.
- By organ transplantation.
- By fresh Blood transfusion.
- CMV needs intimate contact with secretions or excretion of:
- Urine.
- Respiratory system.
- Genital secretion.
- Tears.
- Feces of an infected person.
- The most common is the venereal route through contact with infectious viruses in body secretion.
- The seropositive population is 60% to 80% positive in the Western world, while it is much more in developing countries.
- Seropositive cases increase with age and in the lower socioeconomic group.
- The percentage is high for the people employed in the childcare facility.
- After the neonatal period, infection occurs through contact with saliva or urine.
How will you describe CMV signs and symptoms?
- 90% of these babies are asymptomatic at birth.
- 10% of symptomatic newborns present with jaundice, hepatosplenomegaly, pancytopenia, and compensatory cutaneous hematopoiesis
- Approximately 10% of these babies will die, and the remainder will suffer permanent neurological defects.
- The incubation period is 6 to 8 weeks (4 to 12 weeks).
- In this stage, we can find CMV antigens.
- You can confirm viremia by the culture of the blood.
- Now, the virus is shed in secretion for months or years.
- CMV infection is seen in two different age groups:
- Fetal life.
- Early childhood or late adolescence (or young adults).
- There is increased risk in the following groups:
- Homosexuals.
- HIV-patients.
- Transplant patients.
- The majority of the patients with acute CMV infection are asymptomatic.
- The patients who develop symptoms are sick for 2 to 3 weeks.
- (CMV) may have flu-like symptoms that are not easily differentiated from other illnesses.
- This is seen in infants and is contracted in utero.
- CMV causes serious and life-threatening infections in neonates and immunocompromised patients.
- Congenital infection is acquired in utero during passage through the infected birth canal.
- CMV may be isolated from the throat.
- Immunocompromised patients have more severe illnesses.
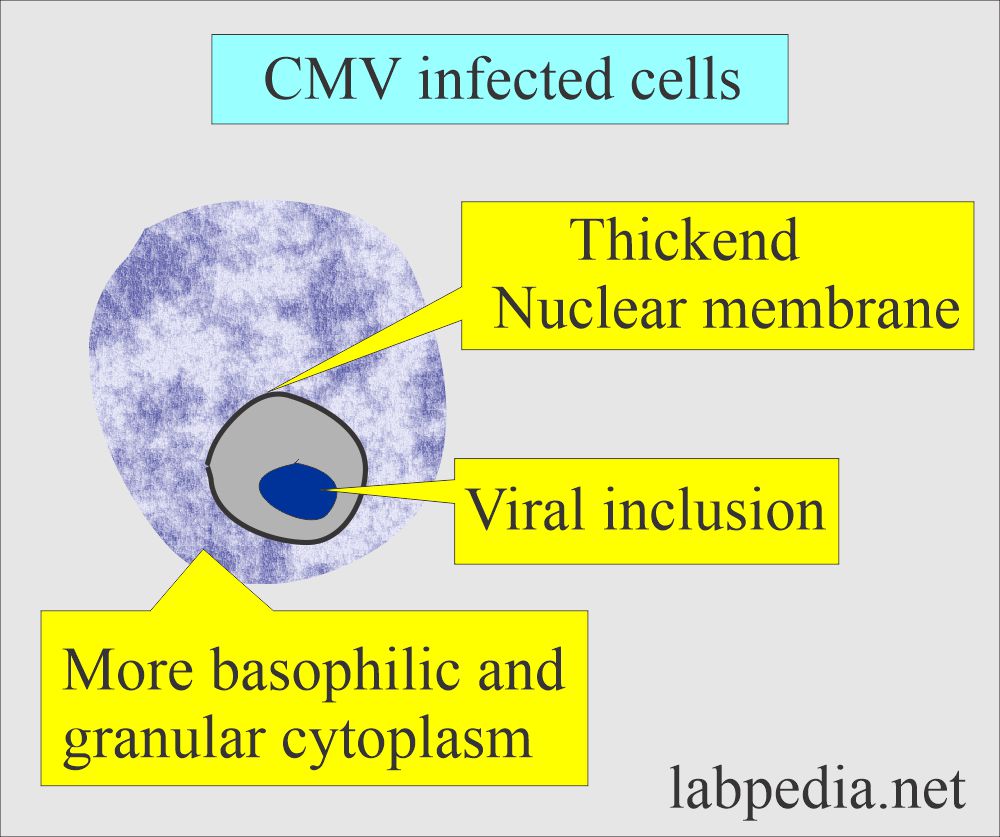
What is the presentation of the Cytomegalovirus (CMV) inclusion in the cells?
- The affected cells typically show nuclear and cytoplasmic inclusion.
- These inclusions, which are basically renal epithelial cells with inclusions, are seen in urine sediments of newborns and young children.
- These inclusions are an intermittent phenomenon, so several samples must be needed.
- Staining the fresh urine sample instead of 24 hours urine is advised, where the cells may integrate.
- Biopsies are better than a urine sample.
How will you discuss the Immunology of Cytomegalovirus (CMV)?
- CMV increases the absolute number of suppressor cells (CD8+) lymphocytes and decreases the number of helper cells (CD4+) lymphocytes.
- This lymphocyte picture persists for months.
- There are atypical lymphocytes in the peripheral blood smear.
- Is there any role of CMV as an oncogenic virus?
- Viral antigens or nucleic acid have been found in human malignancies like adenocarcinoma of the colon, carcinoma of the cervix, Kaposi’s sarcoma, and cancer of the prostate.
- Substantial direct evidence of CMV for Kaposi’s sarcoma exists, but a direct cause-and-effect relationship has not been established.
What is the disease pattern of Cytomegalovirus (CMV)?
- The pattern of the CMV disease is as follows:
- Acquired infection. This is usually asymptomatic and can persist as a chronic or latent infection in the host.
- Latent infection. This persistent infection characterized by the period of reactivation is called latent infection.
- Congenital infection.
- CMV infections are asymptomatic. After the infection, the virus may remain latent in the body.
- Subclinical disease may be seen in early infants.
- Disseminated or fulminant disease is seen in infants, and infection is contracted in utero.
- Late acute disseminated disease is seen in patients with leukemia and malignant diseases.
- Liver disease is a chronic, slow CMV infection that occurs in children between the ages of 6 months and 8 years.
- Post-natal infection may lead to hepatitis.
- In short, there are three groups:
- Perinatal disease (Congenital infection).
- In an immunocompetent person with mononucleosis syndrome.
- In immune-compromised patients, they are at risk of solid organs and bone marrow transplantation.
- Antibody testing on the mother will help the physician diagnose an infection that may harm the unborn baby.
What is the presentation of Congenitally infected infants?
- The test may be ordered on newborns when the infant shows signs of Congenital disease infections.
- The congenitally infected babies show:
- The exceptionally small size of a newborn was relative to the gestational age (low birth weight).
- Deafness.
- Mental retardation.
- Seizures.
- Heart defects.
- Cataracts.
- Enlarged liver or spleen (Hepatomegaly and splenomegaly).
- Low platelet levels Lead to hemorrhagic pneumonitis and petechiae.
- Jaundice due to hemolytic anemia.
- Cerebral calcification.
- Microencephaly.
How will you diagnose Cytomegalovirus (CMV)?
A complete blood count shows leucocytosis.
- There is relative lymphocytosis.
- There are atypical lymphocytes in the peripheral blood smear.
- In infants, there is thrombocytopenia. It is seen in 10% to 15% of the cases.
- Splenomegaly was seen in 35% of the cases.
- Lymphadenopathy was seen in 15 % of the cases.
Liver function tests are abnormal.
The biopsy is useful in diagnosing pneumonitis and gastrointestinal disease due to CMV.
- Biopsy shows typical intranuclear (owl eye) and intracytoplasmic inclusions.
Virus culture can be done from various body samples:
- Urine.
- Saliva.
- Leucocytes.
- Biopsy material.
- Urine, sputum, or mouth swabs are preferred, and fresh samples are taken.
- Freezing of the sample must be avoided, as it will inactivate the virus.
- If you keep the sample in the fridge, the sample may be used for up to one week.
- The urine sample is diluted with an equal alcohol volume (70% to 90%).
- Urine positive for CMV indicates:
- Acute infection.
- Asymptomatic patient.
- Active disease.
- The urine sample is the best sample for the recovery of CMV.
- There are inclusion bodies in leucocytes of urine sediments.
- Washings, swabs, and biopsies are kept in sorbitol diluent or at -70 °C. (Another reference says that freezing the sample is not good in the case of CMV. It prefers to refrigerate the sample.)
- CMV culture can not differentiate between acute infection, reinfection, or reactivation of the latent virus.
- CMV culture has three exceptions, and it will indicate a congenital infection:
- Positive culture of the blood suggests transient viremia.
- Positive culture of fetal amniotic fluid.
- Positive culture of the newborn or neonates.
Serological tests:
- A fourfold increase in the titer indicates acute infection when the samples are taken 1 to 2 weeks apart.
- The antibody to early antigen undergoes a relatively rapid decline after the recovery but can persist for up to 250 days.
- This antibody can detect recent and active infections.
- Antibodies to the early antigen are strongly associated with viral shedding.
- The prevalence of CMV antibodies varies with age and geographical location but ranges from 40% to 100%.
- Detect antibody IgM for acute infection indicates primary infection.
- The positive serological test in infants’ first three weeks indicates congenital infection.
- Positive after the 4th week indicates an infection of postpartum or intrapartum infection.
- IgG indicate convalescent stage.
- The increasing titer of IgG antibody indicates acute infection.
- The most common methods used are:
- Enzyme immunoassay (EIA).
- Indirect immunofluorescence (IIF).
- ELISA.
- Complement fixation test.
- Anticomplement immunofluorescence.
- Indirect hemagglutination.
- Serological tests are positive in a population after the age of 30, between 40% and 100%.
What is the Policy for pregnant mothers?
- Test the pregnant mother in the first trimester.
- If positive, then test for viremia every three months.
- The fetal blood or amniotic fluid can confirm congenital infection from the IgM antibody.
- Amniocentesis is not helpful before 21 weeks of gestation because of inadequate urine released by the fetus.
- PCR may be advised on the newborn blood sample.
- False-positive serological tests are seen in patients with Rh-factor, heterophil antibodies, and varicella.
How will you treat Cytomegalovirus (CMV)?
- There is no cure for CMV infection, but antivirals may be tried.
- For congenital CMV, treat with Ganciclovir or Valganciclovir for six months.
- Other CMV conditions are treated with Ganciclovir and Foscarnet.
- Cidofovir is reserved for resistant cases.
How will you summarize the diagnosis of CMV?
- Check mother IgM and IgG antibodies for CMV.
- Culture mother blood for CMV.
- Culture newborn urine, saliva, and blood in the first 2 weeks of the newborn.
- Try to find CMV nuclear inclusions.
- CMV-PCR can be done on amniotic fluid and cord blood.
- CMV-PCR can be done on newborn urine and blood in the first 2 weeks of life.
Questions and answers:
Question 1: What is the best sample for the diagnosis of CMV?
Question 2: What is the significance of the serology for the diagnosis of acute CMV?