Rotor’s Syndrome
Rotor’s Syndrome
Sample for Rotor’s Syndrome
- The serum of the patient is needed.
- A urine sample can be used.
Precautions for Rotor’s Syndrome
- Avoid the hemolyzed sample.
- Avoid lipemic serum.
- Avoid serum from the light.
- Avoid urine from exposure to light.
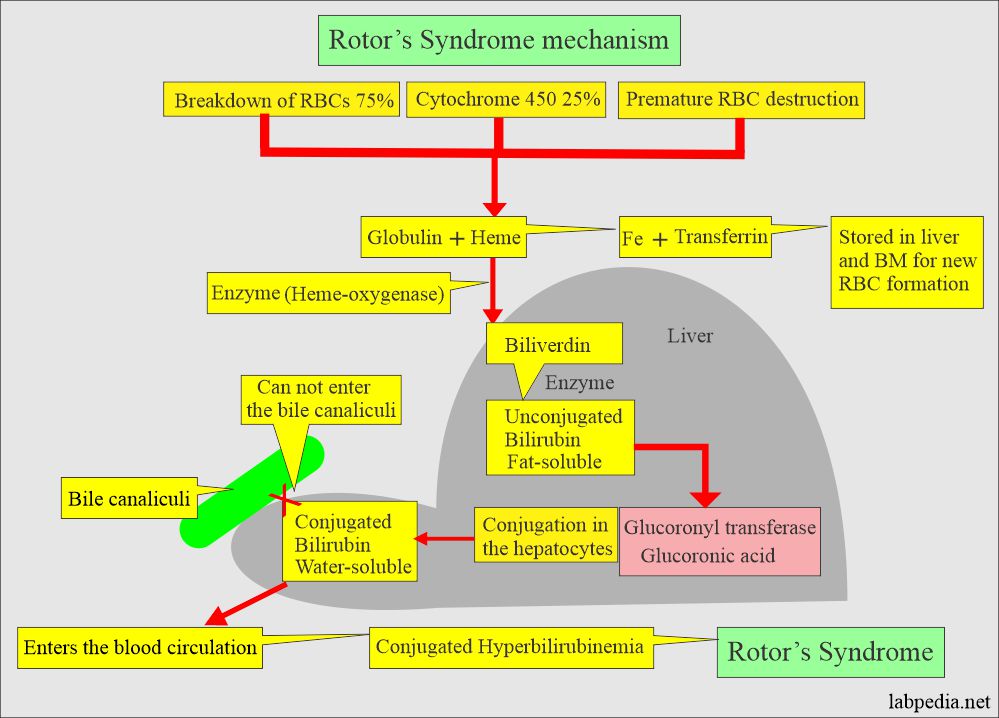
Pathophysiology of Rotor’s Syndrome
- This is a rare, relatively benign (mild) autosomal recessive disease of the liver.
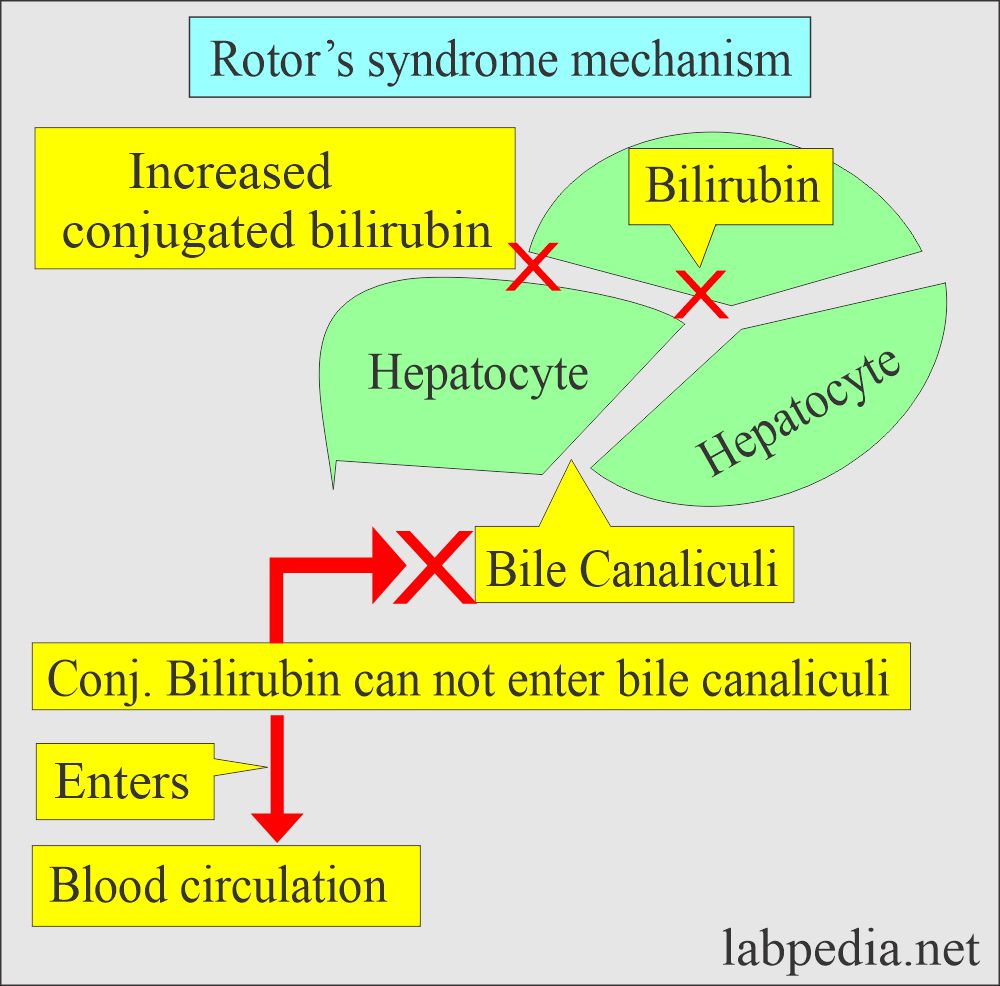
- This is similar to Dubin-Johnson syndrome, and both lead to increase conjugated (direct) bilirubin.
- There is an impairment in the excretion of bilirubin from hepatocytes into the canalicular bile lumen.
- This causes defective:
- Excretion of conjugated bilirubin.
- It’s reabsorption into the blood.
- Excretion in the urine.
- The difference between Rotor’s syndrome from the Dubin-Johnson syndrome is:
- There is no hepatic pigmentation.
- Oral Cholecystography also differentiates, which is normal in this condition.
- Ultrasound shows no abnormality.
- Liver biopsy shows no pigmentation.
Signs and symptoms of Rotor’s Syndrome
- This disease is usually seen in infancy or childhood.
- There is chronic jaundice without any evidence of hemolysis.
- Sometimes these patients may have intermittent epigastric discomfort and abdominal pain.
- There may be an attack of fever.
| Signs and symptoms | Rotor’s syndrome | Dubin-Johnson syndrome |
| Incidence |
|
|
| Inheritance mode |
|
|
| Age at onset of jaundice |
|
|
| Signs and symptoms |
|
|
| Bilirubin level |
|
|
| Mechanism of rotor’s syndrome |
|
|
| BSP (Impaired excretion of dye) |
|
|
| Oral cholecyctogram |
|
|
| Liver biopsy |
|
|
| Treatment |
|
|
Diagnosis of Rotor’s Syndrome
- There is jaundice with increased conjugated bilirubinemia.
- Liver biopsy is normal in histology.
- The gallbladder can be visualized by cholecystography. This differentiates it from Dubin-Johnson syndrome.
Treatment of Rotor’s Syndrome
- This is a benign disease, and no active intervention is needed unless another cause of liver disease exists.
How will you describe different types of inherited jaundice?
| Clinical parameters | Unconjugated Hyperbilirubinemia | Conjugated Hyperbilirubinemia | |||
| Gilbert’s disease | Type 1 Criggler-Najjar | Type II Criggler-Najjar syndrome | Rotor’s syndrome | Dubon-Jhonson syndrome | |
| Inherited mode | Autosomal dominant | Autosomal recessive | Autosomal dominant | Autosomal recessive | Autosomal recessive |
| Incidence | <7% of the population | Very rare | Uncommon | Rare | Uncommon |
| Age at onset | In adolescence | In infancy |
|
Early adulthood |
|
| Pathogenesis | Glucoronyl transferase enzyme deficiency (GTE) | GTE decreased | Marked decrease | Impaired conj. bilirubin excretion | Impaired cong. bilirubin excretion |
| Bilirubin level |
|
Mainly indirect | Mainly indirect |
|
|
| Clinical signs/symptoms |
|
|
|
Asymptomatic jaundice in young adults | Asymptomatic jaundice |
| Effect of phenobarbitone | Decreased to normal | There is no effect | Marked decrease | —– | —– |
| BSP (Dye excretion) test | May be mildly impaired in <40% of cases | It is absent | _____ | Positive, Initial rapid fall and then rise in 40 to 90 minutes | Positive, Slow clearance and no rise |
| Oral cholecyctography | Normal | Normal | Normal | Normal | GB usually not visualized |
| Liver biopsy | Normal | —- | —- | No pigments | Characteristic pigments |
| Treatment | Not needed | There is no treatment | Not needed | ||
Questions and answers:
Question 1: What is the main difference between Rotor's syndrome and Dubin Johnson syndrome?
Question 2: What is the treatment of Rotor's syndrome?