Red Blood Cell (RBC):- Part 4 – Red Blood cell Indices
Red Blood cell Indices
Sample for Red Blood cell Indices
- For Blood indices, the best sample is EDTA blood.
- Collect the blood in the lavender top tubes.
- Transport the blood to the lab where blood is run in the hematology analyzer for the calculation of blood indices.
- Blood is stable for 6 hours at 25 °C and for 24 hours at 4 °C.
- Fetal blood is collected percutaneous from the umbilical area.
Purpose of the test (Indications) for Red Blood cell Indices
- These tests are useful for the diagnosis of the various types of Anemia.
Precautions for Red Blood cell Indices
- The abnormal size of RBC may affect indices.
- An increased count of WBC will affect the indices.
- Increased reticulocytes count leads to abnormally high MCV.
- Cold agglutinins give false increased values of MCH, MCHC, and MCV.
Definition of Red Blood cell Indices
- Red cell indices define the size and contents of hemoglobin in Red cells.
Mean corpuscular volume (MCV):
Definition of MCV:
- This is the best index for classifying anemia.
- This is the average volume of red blood cells measured in cubic micrometers (µ3, femtoliter fL).
- This indicates the cell size of RBCs.
Indication of MCV:
- It helps in the classification and differential diagnosis of anemia.
- It is a useful screening test for occult alcoholism.
Interference of various factors for MCV:
- In the case of leucocytosis, there is increased MCV.
- Marked hyperglycemia increases MCV.
- Cold antibodies increase MCV.
- Methanol poisoning increases MCV.
- In the case of increased reticulocytes, there is increased MCV.
- Hemolysis leads to a decrease in MCV.
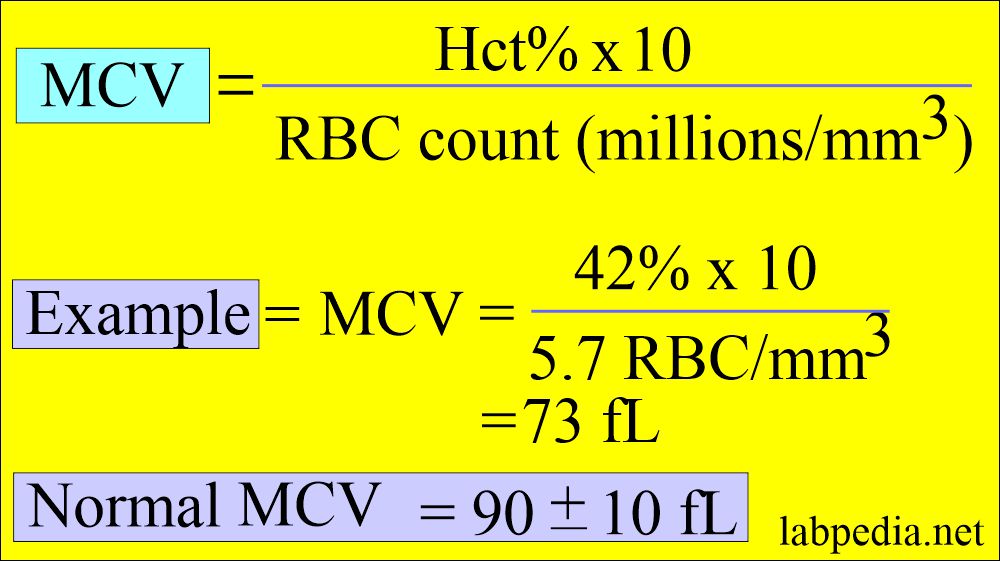
Calculation of MCV:
- MCV is calculated by dividing hematocrit by the total RBC count.
Normal MCV
- Adult (all ages) = 80 to 95 fL
- Newborn = 96 to 108 fL
On the basis of MCV:
- Macrocytes when MCV value is high, e.g., in Megaloblastic anemia, due to vit B and folic acid deficiency.
- Microcytes, when the MCV is decreased seen in iron deficiency anemia and thalassemia.
- In microcytic anemia, MCV is 50 to 82 fL.
- In normochromic normocytic anemia, MCV is 82 to 98 fL.
- In macrocytic anemia, MCV is 100 to 150 fL (>100 fL).
- In normocytic anemia = MCV 80 to 94 fL MCHC >30 g/dL.
Mean corpuscular hemoglobin (MCH):
Definition of MCH:
- This is the mean of the average amount of hemoglobin in red blood cells or the average weight of hemoglobin in absolute units in the RBCs.
- The result gives the average hemoglobin content per RBC in picograms (pg).
- The MCH value is usually higher in newborns and infants because their MCV is higher than that of adults.
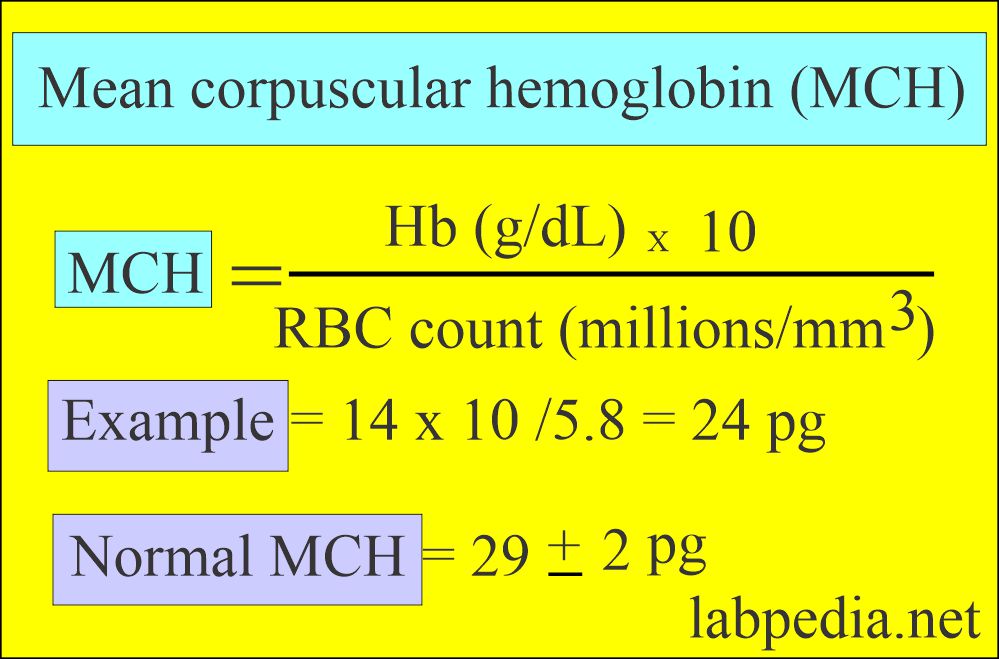
Calculation of MCH:
- MCH is calculated by multiplying Hb g/dl x 10 and dividing by the RBC count.
- Generally, macrocytes will have more hemoglobin, and microcytes will have less hemoglobin. So the values resemble those of MCV.
Indications of MCH:
- It has limited value in the differential diagnosis of anemia.
- It is instrument calibration.
Interference for estimation of MCH:
- Increased white cell count increases the MCH value.
- Cold agglutinins increase the MCH value.
- Lipemia increases the MCH value.
- High concentrations of heparin increase the MCH value.
- Monoclonal immunoglobulin increases the MCH value.
- In vivo hemolysis increases the MCH value.
Normal MCH
- Adult (all ages) = 27 to 31 pg
- Newborn = 32 to 34 pg
Mean corpuscular hemoglobin concentration (MCHC):
Definition of MCHC:
- This is the average concentration or percentage of hemoglobin in each individual red blood cell.
- It is the ratio of the weight of hemoglobin to the volume of the RBCs.
- MCHC is the most useful for monitoring the treatment of anemia.
Indication of the MCHC:
- It is better than MCH to identify hypochromasia.
- Changes in the MCHC appear late in iron deficiency anemia (severe cases).
- It is instrument calibration.
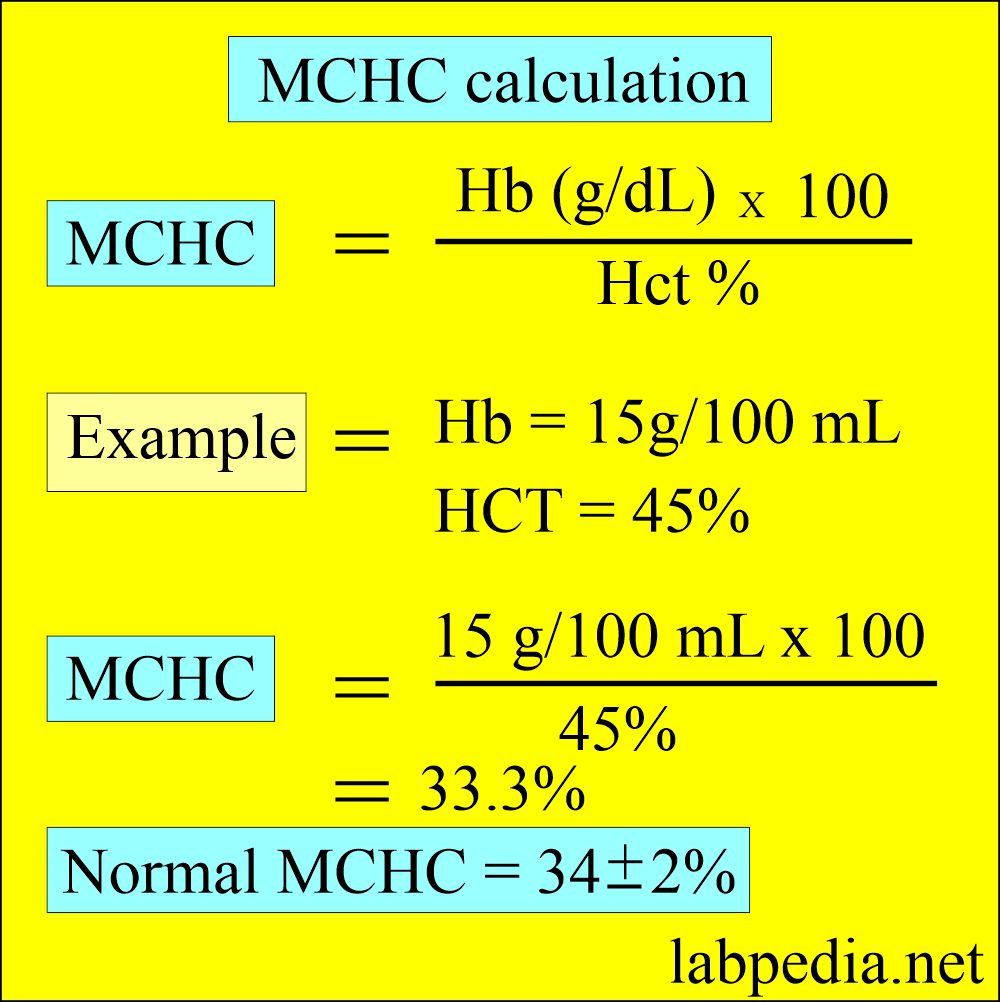
Calculation of MCHC:
- This is calculated by hemoglobin x 100 divided by hematocrit.
- It is the average amount of Hemoglobin per RBcs (33 to 37 g/dL).
Interference of the estimation of MCHC:
- MCHC is decreased in leucocytosis.
- MCHC is increased in Hemolysis, like sickle cell anemia, hereditary spherocytosis, and autoimmune hemolytic anemia.
- Cold agglutinins increase the MCHC.
- Increased concentration of heparin increases the MCHC.
- Rouleaux or RBC agglutination increases the MCHC.
Normal MCHC
- Adults of all ages = 32 to 36 g /dl (32 to 36%)
- Newborn = 32 to 33 g /dl (32 to 33%)
Interpretations of MCHC:
- Hypochromic When MCHC is decreased, there is a hemoglobin deficiency, e.g., in iron deficiency anemia and thalassemia.
- Normochromic when the values are normal (In hemolytic anemia).
- Hyperchromic when MCHC value is increased, and RBC cannot accommodate more than 37 g/dl (seen in spherocytosis, newborns,s and infants).
Red blood cell distribution width (RDW):
Definition of RDW:
- RDW is the quantitative measure of anisocytosis.
- This is the coefficient of the RBC volume distribution.
- This indicates variation in the size of RBC.
- This is calculated by the machine using MCV and RBC values.
- This is helpful for the diagnosis of hematological disorders and monitoring the response to therapy.
- This is also helpful in distinguishing iron-deficiency anemia (RDW increased) from hemoglobinopathies (RDW normal).
Indications for RDW:
- RDW is used to classify the anemias based on MCv and RDW.
- RDW is more sensitive in microcytic than macrocytic RBC conditions.
- RDW is not helpful in cases without anemia.
Calculation of RDW:
Normal RDW
- Adult = 11.5% to 14.5%
Anemias are defined based on cell size (MCV), amount of Hb, and (MCH):
| Parameter | Interpretation | Diagnosis |
| MCV fL | Less than the lower limit of normal | Microcytic anemia |
| Within normal range | Normocytic anemia | |
| Greater than the normal | Macrocytic anemia | |
| MCH pg | Less than the lower limit of normal | Hypochromic anemia |
| Within the normal limit | Normochromic anemia | |
| Greater than the upper limit of normal | Macrocytic anemia |
Classification of anemia on the basis of MCV and MCHC:
| Type of anemia | MCHC% | MCV fL | Causes |
| Normocytic/normochromic | 32 to 36 | 80 to 100 |
|
| Microcytic/hypochromic | <32 | <80 |
|
| Microcytic/normochromic | 32 to 36 | <80 |
|
| Macrocytic/normochromic | 32 to 36 | >100 |
|
MCV:
MCV Increased in:
- Pernicious anemia (vit B12 deficiency or folate deficiency).
- Folic acid deficiency.
- Antimetabolite treatment.
- Chronic liver disease.
- Alcoholism.
- Sprue likes steatorrhea, celiac disease, and intestinal resection or fistula.
- Fish tapeworm infestation.
- Carcinoma of the stomach following total gastrectomy.
- Drugs like oral contraceptives, anticonvulsants, anti-tumor agents, and antimicrobial agents.
- Anemia of hypothyroidism.
- Postspenectomy.
- Myelodysplastic syndrome.
MCV Decreased in:
- Microcytic anemia where MCV <80 fL and MCHC <30 g/dL).
- Iron deficiency anemia.
- Thalassemia.
- Chronic diseases.
- Iron deficiency anemia is usually seen in inadequate iron intake, poor absorption, and chronic blood loss.
- Sideroblastic anemia.
- Anemia of chronic diseases.
- Lead poisoning.
- Disorders of porphyrin synthesis.
MCV normal in:
- Normocytic anemia.
- Some hemolytic anemia.
- In some hemoglobinopathies.
- Hypoplastic and aplastic marrow.
MCH:
MCH Increased in:
- Macrocytic anemias.
- Newborn.
MCH Decreased in:
- Microcytic anemias.
- Hypochromic anemia.
MCHC:
MCHC Increased in:
- Spherocytosis.
- Newborns and infants.
MCHC Decreased in:
- Iron deficiency anemia.
- Thalassemia.
- Microcytic anemia with chronic blood loss.
Question 1: What is the definition of the MCV?
Question 2: What is MCV in microcytic anemia?


It is my choice