Red Blood Cell (RBC):- Part 1 – Erythropoiesis and RBC maturation, RBC Counting Procedure
Erythropoiesis and RBC maturation
Sample for Red blood cell counting
- The blood sample is taken in EDTA.
- It is stable for 24 hours at 23 °C and 48 hours at 4°C.
Purpose of the test (Indications) for RBC counting
- This is advised for anemia or Polycythemia.
- It is a routine part of CBC.
- This is repeated in patients with repeated bleeding.
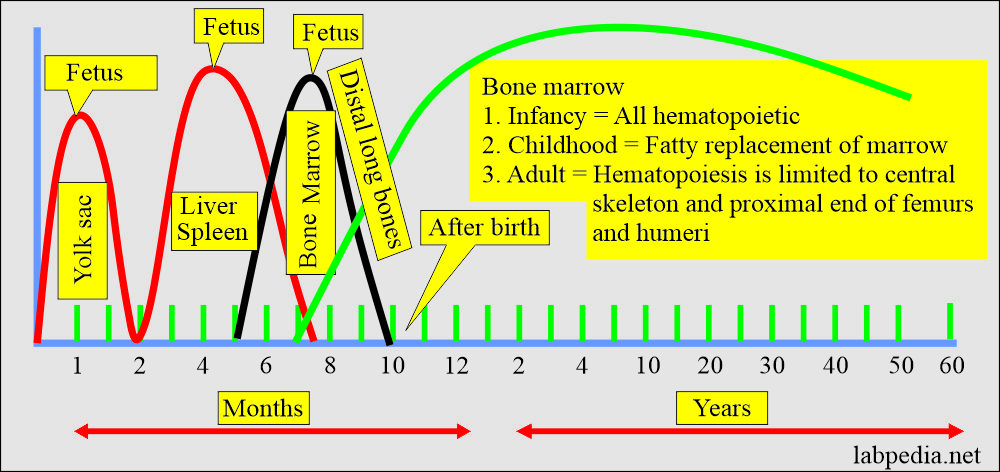
Erythropoiesis in early and adult life:
- In the first few weeks of intrauterine life, the yolk sac’s the primary site for erythropoiesis.
- The liver and spleen follow this from 6 weeks to 6 to 7 months of intrauterine life. These will continue to produce blood cells until about 2 weeks after the birth.
- Bone marrow also takes part and starts from 6 to 7 months of intrauterine fetal life.
- During childhood and adulthood, life bone marrow is the main site of erythropoiesis.
- The RBCs mature in the bone marrow microcirculation and then are released into circulation.
- In the case of increased demand, intramedullary hematopoiesis may be seen.
The various sites of erythropoiesis (Hematopoiesis):
| Stages of human development | Age | Site of the erythropoiesis |
| Fetus | 0 to 2 months | Yolk sac (mesoderm). (It declines by 6 weeks and ends by 2 months) |
|
|
|
|
|
|
|
|
|
|
|
Hematopoiesis is only found in the following:
|
|
|
Bone marrow consists of an equal amount of fat and hematopoietic tissue:
|
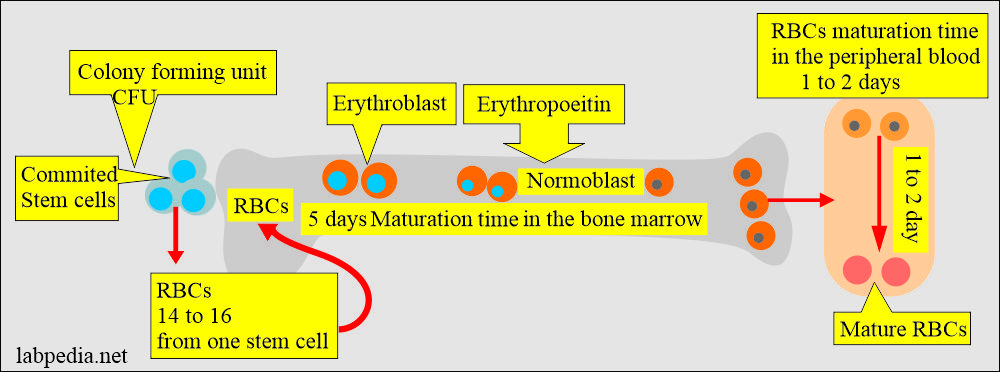
Erythropoiesis (RBC maturation):
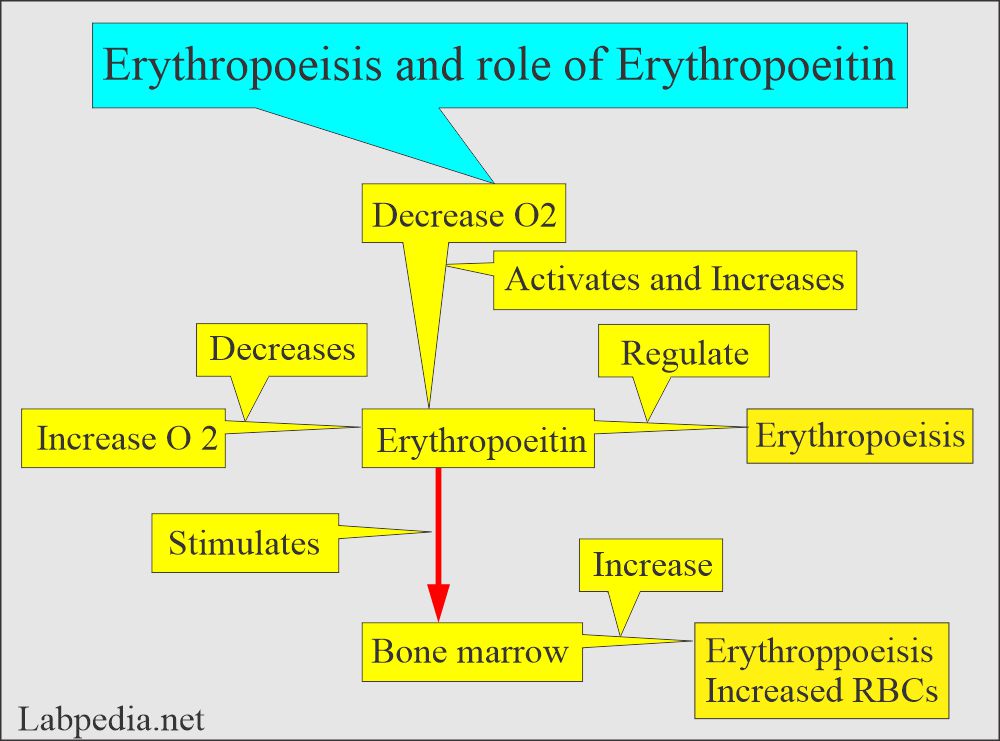
- It is the entire process of producing RBCs in the bone marrow in response to erythropoietin.
- Approximately 1012 new RBCs are produced each day.
- It takes roughly 5 days to cycle in the bone marrow.
- In the peripheral blood, it takes 1 to 2 days.
- By progressive cellular division, one stem cell gives rise to 14 to 16 RBCs.
- Stem cells have a self-renewal capacity, so the bone marrow cellularity remains constant in a normal healthy state.
- One stem cell can produce 106 mature blood cells after 20 subdivisions.
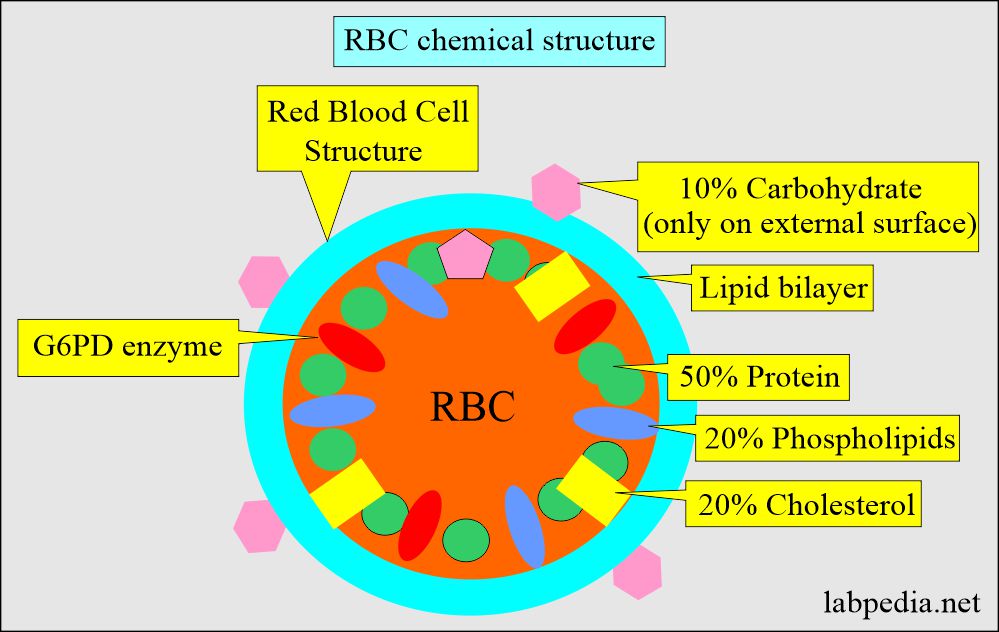
Structure of the red blood cells (RBCs):
- RBCs are biconcave and contain protein, mainly hemoglobin.
- This biconcave shape gives more surface area to combine with oxygen.
- RBCs can change their shape to pass through the smaller capillaries.
- RBC flexibility help to fulfill all the functions:
- The biconcave disc can generate energy as adenosine triphosphate (ATP) by the anaerobic glycolytic (Embden-Meyerhof) pathway.
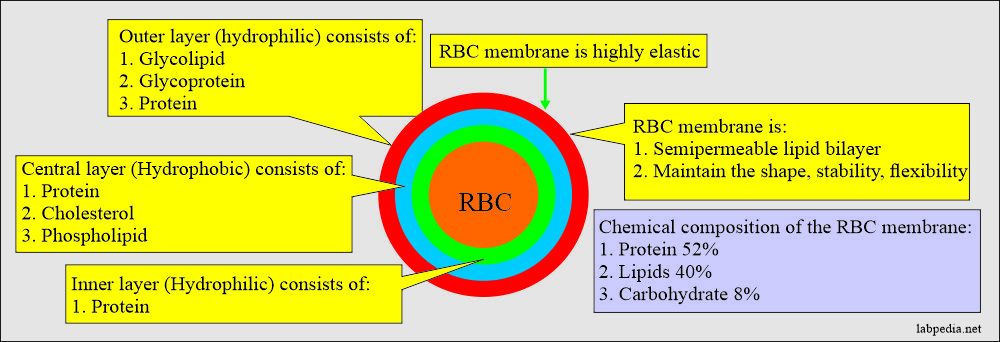
RBC membrane by E/M shows a trilaminar structure consisting of dark-light-dark layers. - These membranes indicate:
- Outer is a hydrophilic membrane consisting of glycolipids, glycoproteins, and protein.
- Central is a hydrophobic layer containing protein, cholesterol, and phospholipids.
- The inner layer is hydrophilic, consisting of protein.
- The RBC membrane is highly elastic, responds to the applied stress of fluid forces, and can undergo large membrane extension without undergoing any fragmentation.
- The biconcave disc can generate energy as adenosine triphosphate (ATP) by the anaerobic glycolytic (Embden-Meyerhof) pathway.
Erythropoiesis and RBC maturation:
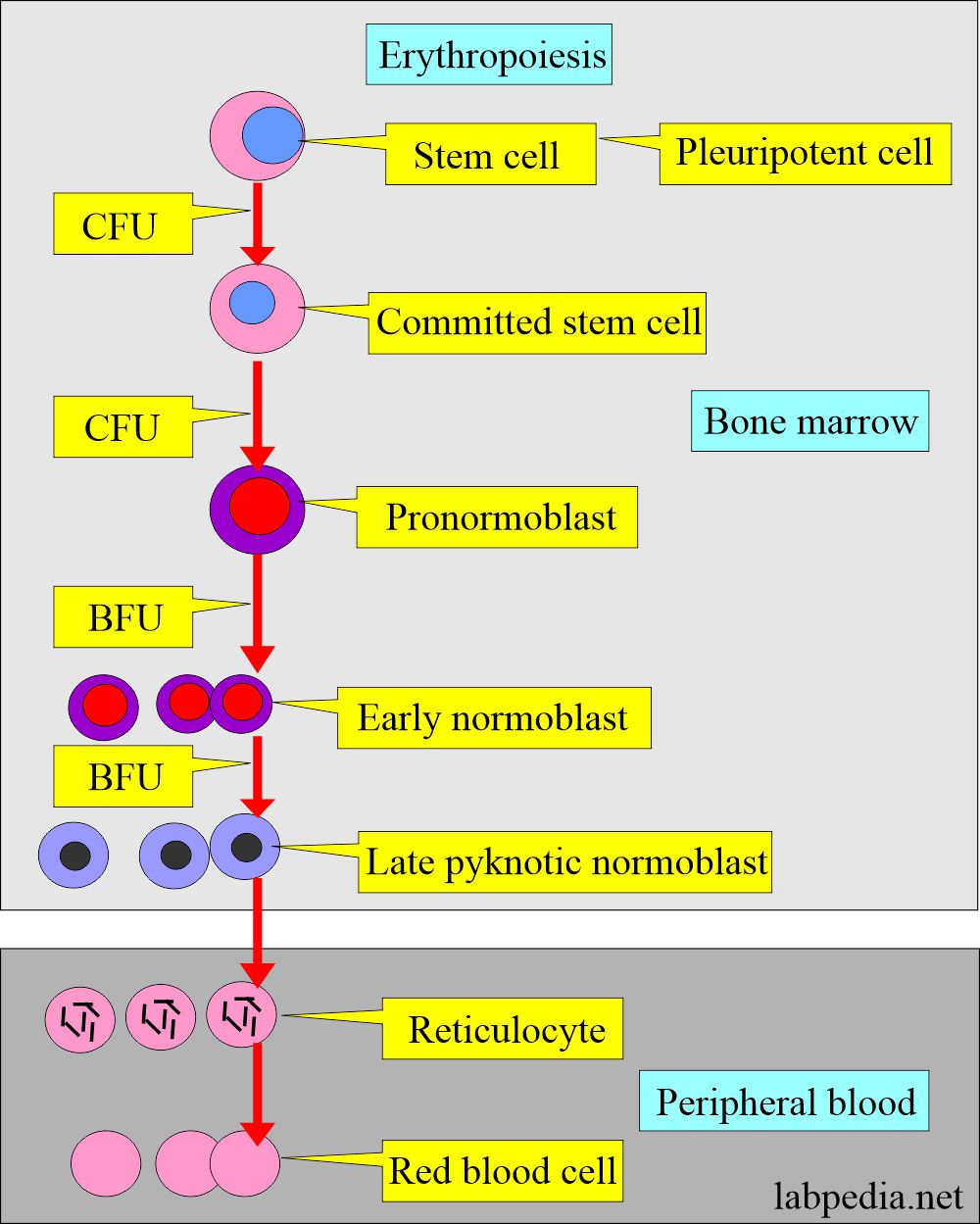
Maturation in the bone marrow:
- Bone marrow provides a suitable environment for stem cell survival, growth, and development. This consists of stromal cells and a microvascular network.
- Stromal cells consist of adipocytes, fibroblasts, endothelial cells, and macrophages.
- RBC develops from the erythroblasts in the bone marrow, which form from the stem cells.
- The stem cell becomes committed to stem cells under the colony-forming unit (CFU) influence.
- Committed stem cell becomes pronormoblast.
- Pronormoblast transforms into early normoblast under the influence of a burst-forming unit (BFU).
- Erythroblast transforms into normoblast, which will form matures RBC. This process takes place under the influence of erythropoietin.
- The committed stem cells develop under the influence of burst-forming units (BFU).
Differentiating points in the RBC stages morphology:
| Features | Pronormoblast | Normoblast | Reticulocyte | Mature RBC |
| Cell size µm | 14 to 19 | 12 to 17 | 7 to 10 | 7 to 8 |
| Nuclear shape | round | round | absent | absent |
| Nuclear chromatin | reddish-blue | blue purple | absent | absent |
| Nucleoli | 0 to 2 | absent | absent | absent |
| Cytoplasm | dark or royal blue | pink, moderate | clear, gray-blue | pink |
Maturation of Red blood cells in the peripheral blood (Erythropoiesis and RBC maturation):
- It occurs from the reticulocytes and transforms into mature red blood cells.
- RBCs take 1 to 2 days to mature as red blood cells.
- Bone marrow maturation is influenced by a colony-forming unit (CFU).
- The normal RBC life span is 120 days, and it can travel around 300 miles (480 km) in circulation.
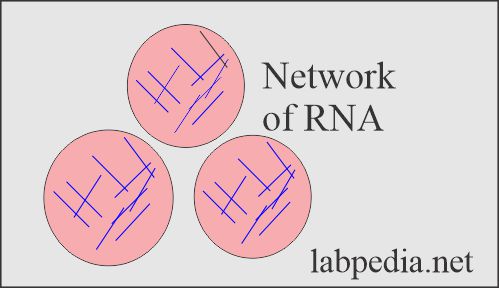
- Mature RBCs can be differentiated from the normoblast and reticulocytes.
- The normoblastic cells have a prominent nucleus, while reticulocytes have remnants of nuclear chromatin (RNA).
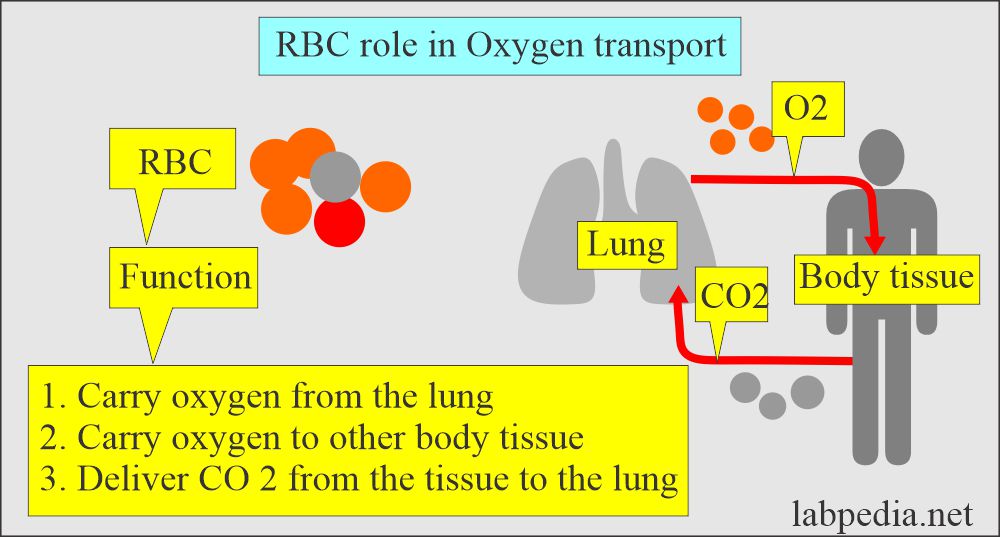
Red Blood Cell functions:
- The RBCs’ primary function is to carry oxygen from the lungs to other body tissue and deliver CO2 from the tissue to the lung.
- After oxygenation in the lung, RBC carries O2 back to body tissue.
- RBCs are biconcave, giving Hb more surface area to combine with O2.
- Hemoglobin of RBCs facilitates CO2 excretion.
- RBCs can change shape, so they can easily pass through the small capillaries.
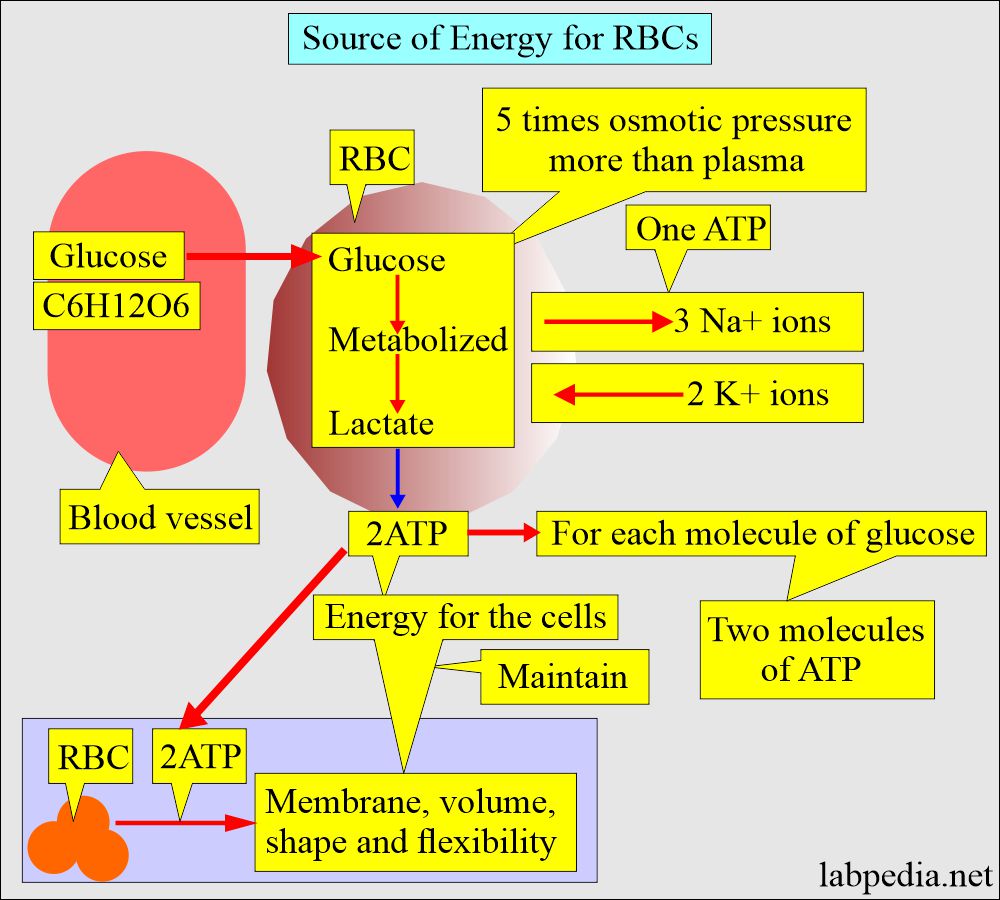
Source of energy for RBC:
- RBC utilizes glucose, which generates 2 ATP molecules that generate energy to maintain:
- Hb function.
- RBC membrane.
- RBC volume.
- RBC shape
- RBC flexibility.
- Adequate amounts of reduced pyridine nucleotide.
- Glucose is metabolized in the RBC, and it needs a Glucose-6-phosphate dehydrogenase enzyme to convert glucose to Fructose-6-phosphate.
- RBCs generate energy almost exclusively through the anaerobic breakdown of glucose.
- The adult RBCs possess little ability to metabolize fatty acids and amino acids.
- Mature RBCs do not possess mitochondria for oxidative metabolism.
RBC life span:
- RBC life in the peripheral blood is around 120 days.
- The aged RBCs are extracted from the blood by the spleen.
- Abnormal RBCs have a shorter lifespan.
- Hypersplenism may destroy the RBCs and remove them from circulation.
- There are approximately 500 RBCs for one WBC.
Normal Values of red blood cells
Source 1
- Cord blood = 3.9 to 5.5 million/cmm
- Adult = 18 to 44 years :
- Male = 4.7 to 6.1 million/cmm.
- Female = 3.8 to 5.4 million/cmm
- 45 to 64 years :
- Male = 4.2 to 5.6 million/cmm.
- Female = 3.8 to 5.0 million/cmm
- 65 to 74 years :
- Male = 3.8 to 5.8 million/cmm.
- Female = 3.8 to 5.2 million/cmm
Source 4
| Age | Normal value |
| Birth to 2 weeks | 4.1 to 6.1 x 106/cmm |
| 2 to 8 weeks | 4.0 to 6.0 x 106/cmm |
| 2 to 6 months | 3.8 to 5.6 x 106/cmm |
| 6 months to 0n3 year | 3.8 to 5.2 x 106/cmm |
| 1 to 6 years | 3.9 to 5.3 x 106/cmm |
| 6 to 16 years | 4.0 to 5.2 x 106/cmm |
| 16 to 18 years | 4.2 to 5.4 x 106/cmm |
| >18 years male | 4.5 to 5.5 x 106/cmm |
| >18 years female | 4.0 to 5.0 x 106/cmm |
| Men | 4.2 to 5.4 x 106/cmm |
| Women | 3.6 to 5.0 x 106/cmm |
Procedure to count RBCs:
Hayme’s solution consists of the following:
- Na Cl = 1 G (Isotonic solution).
- Na2SO4 = 5 grams. It will prevent rouleux formation.
- HgCl2 = 0.5 G acts as an antiseptic.
- D. H2O = 200 mL
Gower’s solution consists of the following:
- Na Cl for an isotonic solution.
- Na2SO4 = 12.5 G
- Glacial acetic acid = 33.3 G
- D.H2O = 200 mL
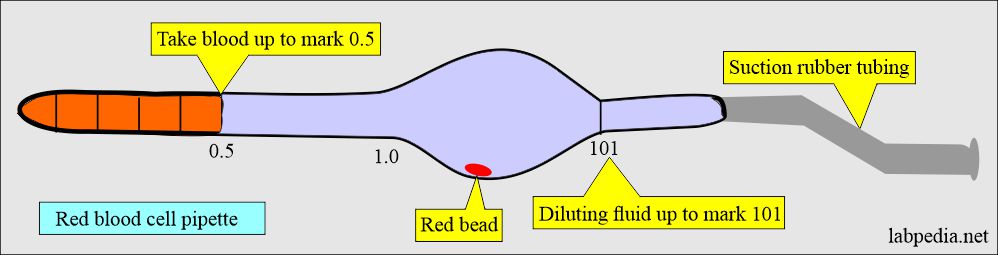
Procedure for RBC counting:
- RBCs counting solution is Hayem’s or Gowers isotonic saline.
- Make a dilution of 1:200 with a diluting solution. Fill the red bulb pipette up to 0.5 marks with the blood.
- Draw the solution to mark 101 of the RBC pipette.
- Mix the blood thoroughly in the pipette.
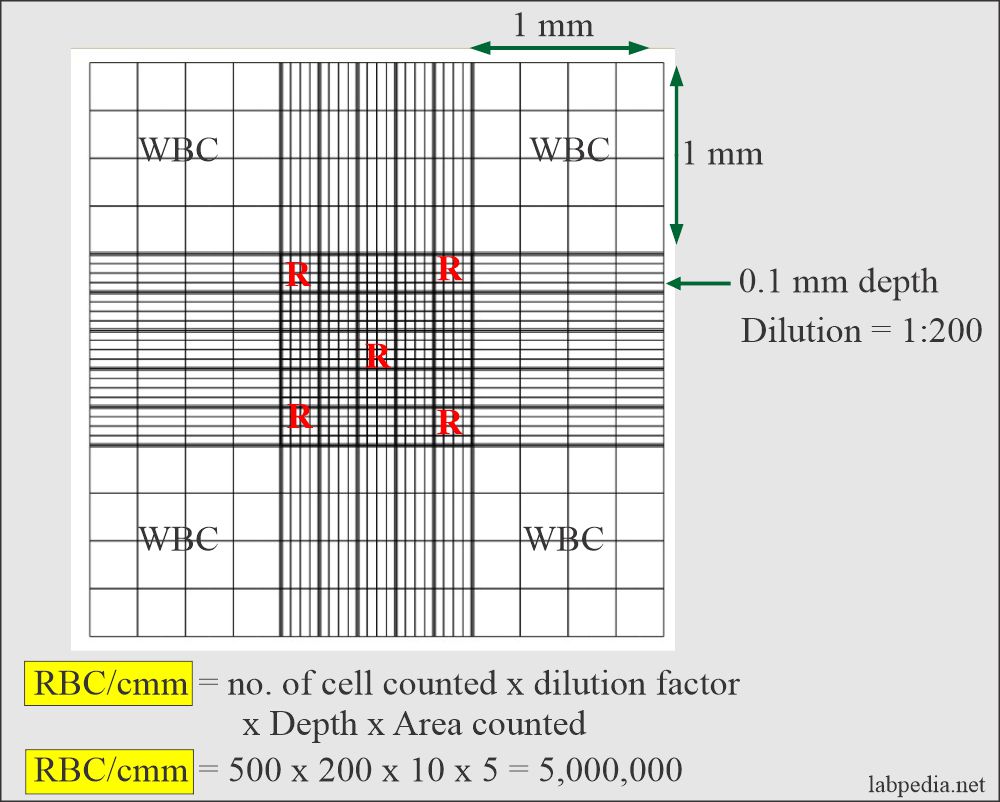
- Discard the first few drops (4 to 5 ) and fill the Neubauer chamber.
- Make sure that the chamber is free of air bubbles.
- The distribution of the cells should be uniform over the ruled area.
- Allow for 2 minutes to settle the cells.
- Now count RBCs in the Neubauer chamber.
- Use 40 X to count the RBCs.
- For RBCs, use the center square, which has 25 smaller squares.
- Count the corner 4 squares and one central square.
- Count only the RBCs that fall on these squares’ left and top borders.
- Repeat the count twice and divide by 2 to get the average.
The formula for RBCs count is as follows:
- Multiply factor = 10 x 200 / 0.2 = 10,000
- Multiply RBC count by 10,000 = RBCs million/cmm.
Increased RBC count is seen in the following:
- Primary Erythrocytosis.
- Polycythemia.
- Erythremia (Erythrocytosis).
- Secondary Erythrocytosis.
- Vigorous exercise.
- Hemoconcentration.
- High Altitude.
- Chronic obstructive pulmonary disease (COPD).
- Severe dehydration.
- Thalassemia trait.
- Hemoglobinopathies.
- Congenital heart disease.
- Extra-renal tumors.
- Tobacco use.
Decreased RBC count is seen in the following:
- Anaemias.
- Drugs that cause aplastic anemia.
- G-6 PD deficiency.
- Immune mechanism.
- Malignancy like Hodgkin’s disease and lymphomas.
- Acute and chronic hemorrhage.
- Autoimmune diseases like SLE and rheumatoid arthritis.
- A chronic infection like subacute endocarditis.
- Cirrhosis.
- Dietary deficiency of iron and vit B12.
- Pregnancy.
- Marrow failure, e.g., Bone Marrow fibrosis, leukemia infiltration, chemotherapy, and antiepileptic drugs.
- Drugs leading to bone marrow failures like quinidine, chloramphenicol, and hydantoin.
- Hemolysis is seen in spherocytosis, G6PD deficiency, and splenomegaly.
- Genetic abnormality is seen in thalassemia and sickle cell anemia.
- Hemorrhage, e.g., in GI tract or trauma.
- Chronic illness due to infections or malignancies.
- Organ failure is seen in renal diseases.
Differentiating points in the RBC stages morphology:
| Features | Pronormoblast | Normoblast | Reticulocyte | Mature RBC |
| Cell size µm | 14 to 19 | 12 to 17 | 7 to 10 | 7 to 8 |
| Nuclear shape | round | round | absent | absent |
| Nuclear chromatin | reddish-blue | blue purple | absent | absent |
| Nucleoli | 0 to 2 | absent | absent | absent |
| Cytoplasm | dark or royal blue | pink, moderate | clear, gray-blue | pink |
- Please see more details in CBC and peripheral blood smear.
Questions and answers:
Question 1: What is the difference between mature RBCs and reticulocytes?
Question 2: Is it possible that RBC can pass through the capillaries and what is the reason for this function?