Prothrombin Time (PT)
Prothrombin Time (PT)
What sample is needed for Prothrombin Time (PT)?
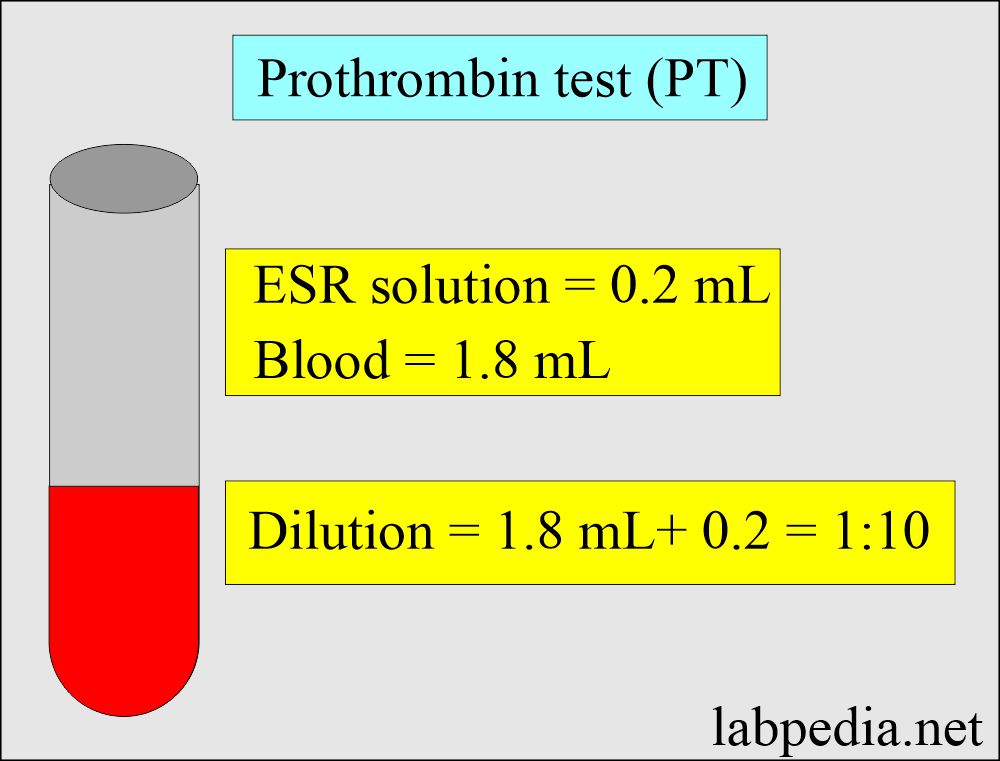
- The blood sample is taken with an ESR (sodium citrate) solution.
- The blood sample is 1.8 ml, and the ESR solution is 0.2 ml.
What precautions are needed for Prothrombin Time (PT)?
- Alcohol intake can increase PT time.
- A high-fat diet may decrease PT time.
- Some drugs decrease PT, like anabolic steroids, digitalis, Benadryl, griseofulvin, oral contraceptives, vitamin K, and chloral hydrate.
- Some drugs, such as aminosalicylic acid, barbiturates, beta-lactam antibiotics, chloramphenicol, clofibrate, heparin, methyldopa, neomycin, quinidine, quinine, sulphonamides, and salicylates, can increase PT.
What are the Indications for Prothrombin Time (PT)?
- This is one of the screening tests for coagulation.
- This test evaluates the extrinsic pathway defect.
- This test also finds a common pathway defect.
- This test is done to screen for prothrombin deficiency.
- PT is also used to evaluate dysfibrinogenemia.
- PT is done to monitor the effects of heparin and coumarin.
- In the case of bruises and abnormal bleeding.
- In the case of Vit. K deficiency.
- This is advised as a liver function test.
- This is used to assess synthetic liver function.
- To monitor the Warfarin therapy.
- This test can also be used in three different ways:
- To monitor anticoagulant therapy with Coumadin.
- As a part of general screen coagulation system disorder.
- It is used as a liver function test.
How will you discuss the Pathophysiology of Prothrombin Time (PT)?
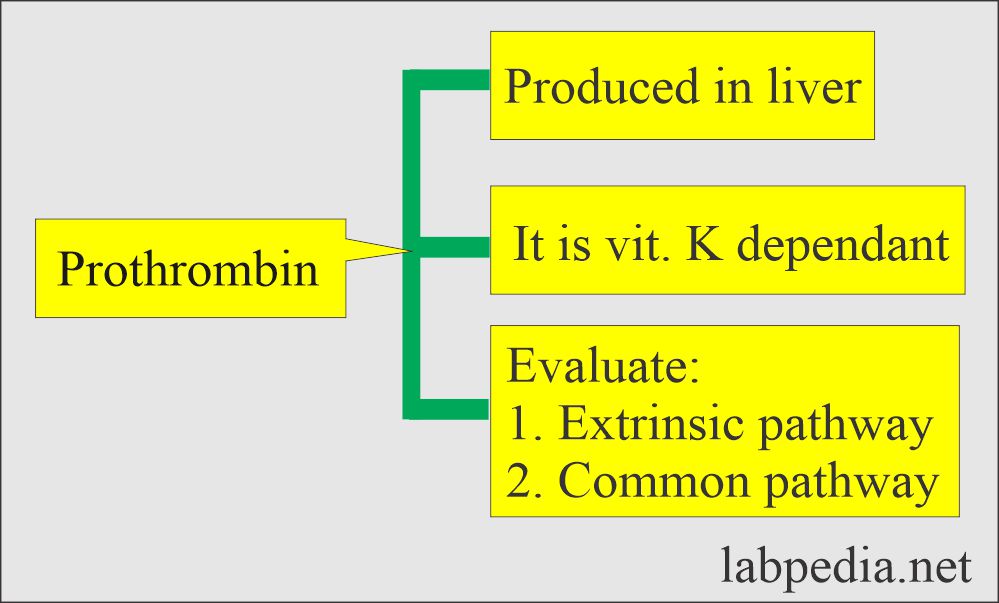
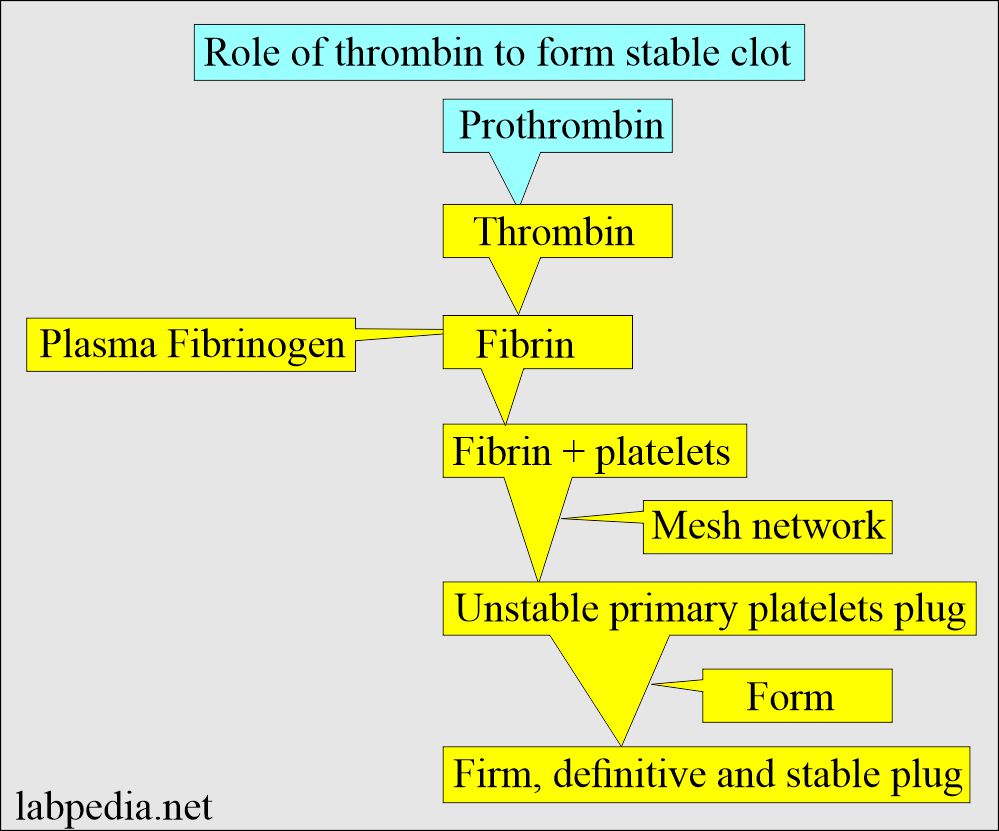
- Prothrombin is a protein produced by the liver. Its molecular weight is 71,600 Daltons.
- Prothrombin helps in the clotting mechanism.
- Prothrombin production depends upon the adequate intake amount of Vit. K and its absorption.
- It is the most abundant and has a long half-life of the vit. K-dependent clotting proteins circulate as a zymogen to serine protease.
- On clotting, prothrombin is converted into thrombin.
- Prothrombin
 Thrombin.
Thrombin.
- Prothrombin
- Factor II, VII, IX, and X depend upon the Vit. K for biosynthesis.
What are the facts about Prothrombin?
- The abnormality in prolonged Prothrombin test (PT):
- Factors I, II, VII, and X deficiency.
- Warfarin, liver diseases, and vit. K deficiency.
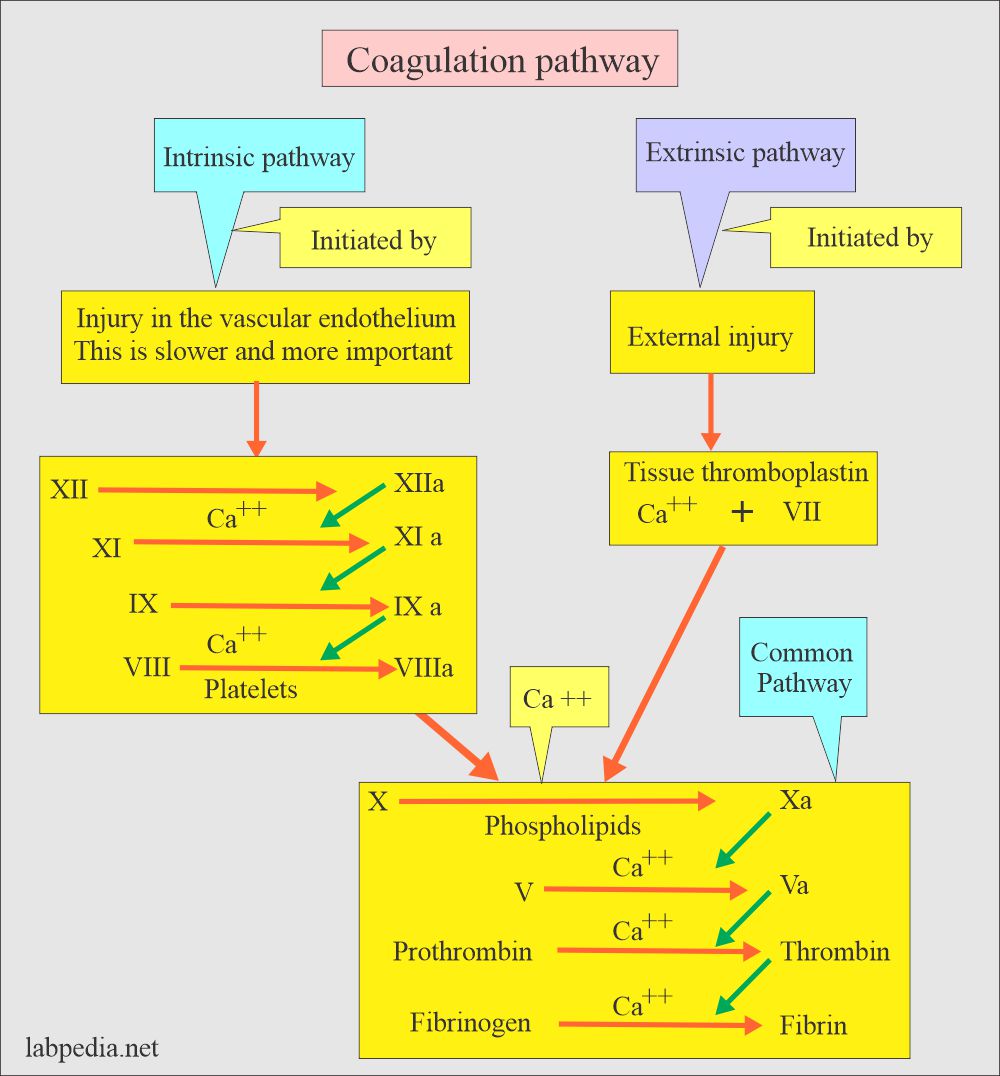
- Prothrombin Time (PT) measures :
- Extrinsic pathway (Activated VIIa)
- Tissue factor.
- Common pathways (factor X, V, II, and fibrinogen ).
What is the Principle of prothrombin time (PT)?
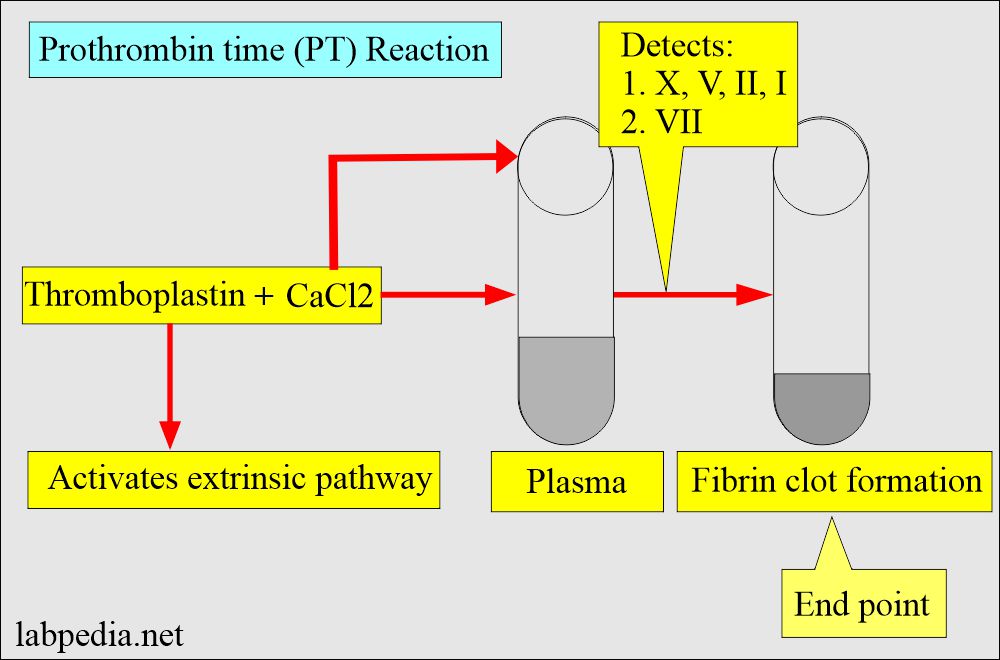
- A complete tissue thromboplastin and calcium were added to the patient’s plasma.
- Complete thromboplastin contains tissue-derived material that will activate the extrinsic pathway.
- Phospholipids act as platelet subtitiues.
- The endpoint is the fibrin clot formation.
- PT will indicate extrinsic pathway defect (prothrombin and factors V, VII, and X).
- In case of severe fibrinogen deficiency, PT may be abnormal.
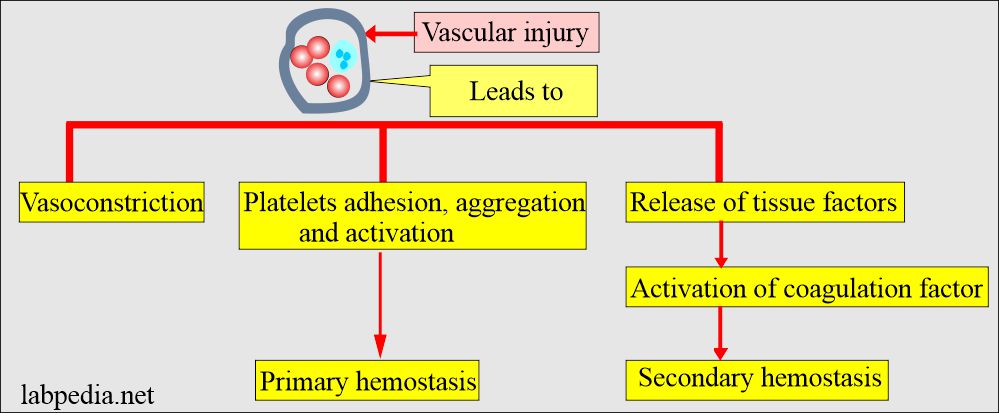
How will you discuss the Clotting Mechanism?
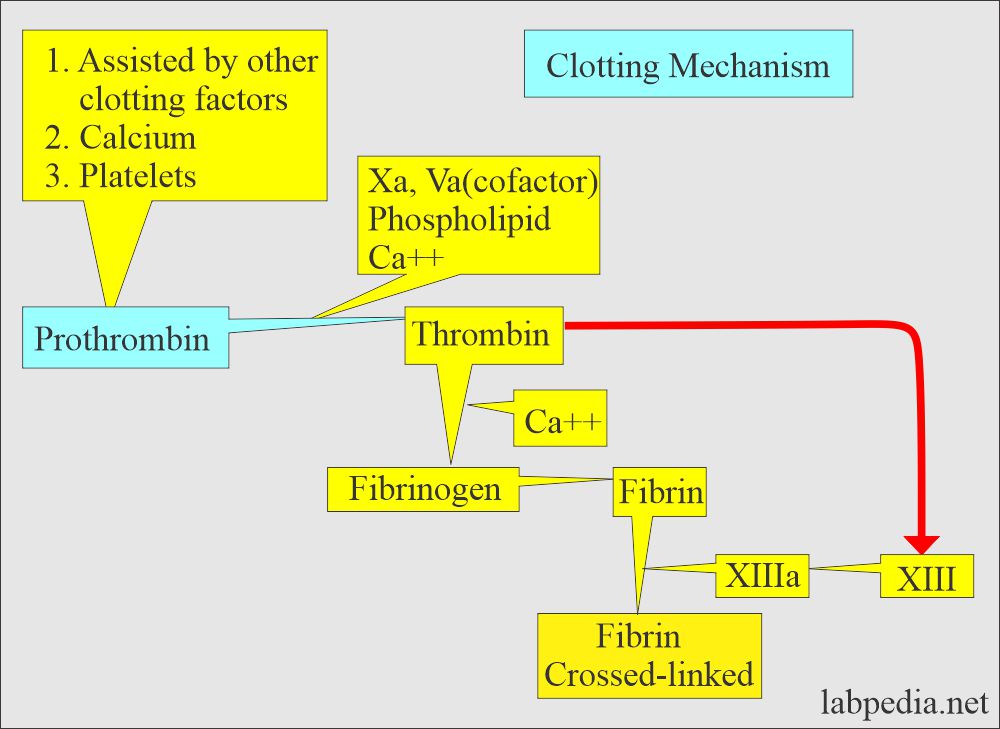
- The first stage is an aggregation of platelets to plug the damaged blood vessels.
- The second stage is the activation of clotting factors.
- The first phase is the activation of the intrinsic pathway.
- At the same time, the extrinsic pathway is activated.
- By common pathway, factor X is activated by the proteases formed by the intrinsic and extrinsic pathways.
- The fourth phase is the conversion of prothrombin to thrombin in the presence of Factor X, Factor V, phospholipids, and calcium.
- Thrombin converts fibrinogen to fibrin.
- Fibrin is converted into a stable gel.
- XIII cross-links the fibrin and forms the clot.
What is the normal value of Prothrombin Time (PT)?
- PT = 11 to 13 seconds (normally PT is 85% to 100%)
- (This may vary from lab to lab).
- This should be compared with the control, which will be around 11 to 14 seconds.
- Anticoagulant therapy response = 1.5 to 2 times the control value.
- Critical value = >20 seconds
- INR is an international normalized ratio. = 0.8 to 1.1
What are the causes of Increased Prothrombin Time (PT)?
- Deficiency of factor II (prothrombin), V, VII, and X.
- Liver diseases, like cirrhosis and hepatic failure.
- Factor I, II, V, VII, IX, and X are produced in the liver.
- This is abnormal when there is a severe disease of the liver.
- Biliary obstruction. There is a lack of bile, which is needed for the absorption of fat-soluble vitamins like Vitamins A, D, E, and K.
- Synthesis of factors II, VII, and X depends upon the vitamin K.
- Suppose the patients respond to Vit. K therapy in 1 to 3 days means no liver cell damage; instead, there is a biliary obstruction.
- If there is no response to Vit. k therapy, the patient has severe liver cell injury.
- Sprue, celiac disease, and chronic diarrhea.
- Vit. K deficiency, even in the newborn of the mother with Vit. K deficiency.
- Hemorrhagic disease of the newborn.
- Anticoagulant therapy (Warfarin and Coumadin).
- D I C.
- Factor 1 deficiency (Hypofibrinogenemia).
- Dysfibrinogenemia.
- Circulating anticoagulants are seen in lupus disease.
- Premature newborn.
- Salicylates intoxication.
- Massive blood transfusion.
Describe the summary of Prothrombin Time (PT) and Partial thromboplastin Time (PTT)?
- Abnormal PTT alone:
- Bleeding due to deficiency of factors V11, IX, and XI.
- Abnormal PT only:
- Factor VII deficiency.
- Abnormal PT and PTT both:
- Anticoagulant therapy.
- D I C.
- Vit. K deficiency.
- Liver diseases.
- Massive blood transfusion.
- Rarely due to Dysfibrinogenemia and deficiency of factors X, V, and II.
How will you Summarize the coagulation profile tests?
| Clinical condition | Prothrombin time | Thrombin time | APTT | Platelets count |
| Heparin therapy | prolonged mild | prolonged | prolonged | normal (the count is low) |
| Oral anticoagulants | Prolonged | normal | prolonged | normal |
| Circulating anticoagulant | normal/prolonged | normal | prolonged | normal |
| DIC | prolonged | prolonged | prolonged | low |
| Liver disease | prolonged | normal (rarely prolonged) | prolonged | low |
| Blood transfusion, massive | prolonged | normal | prolonged | low |
| Vit. K deficiency | prolonged | normal | prolonged | normal |
- For more information, please see PTT and APTT.
Questions and answers:
Question 1: What factor deficiency will be diagnosed by prothrombin time?
Question 2: What is the critical value of prothrombin time?