Pregnancy test:- Part 1 – Normal Pregnancy, Beta-HCG, Human Chorionic Gonadotropin (HCG),
Normal Pregnancy
Sample for Beta-HCG
- This is done in the urine of the patient.
- Collect the morning sample, which has the maximum concentration of HCG.
- Try to do the test on a fresh urine sample.
- You can collect the urine at any time of the day.
- Urine specimens should be clear in the case of turbidity or urine sediments requiring filtration or centrifuge.
- Instruct the patient not to drink after 2000 hours (8 PM) until the morning collection of the urine sample.
- This test can be done in the serum.
- Perform the test within 48 hours of collection.
- Important: Centrifuge the urine at 900 x g for 10 minutes.
- Can store the sample at 2 to 8 °C for 48 hours.
- Serum for β – HCG is stable for up to 7 days at 2 to 8 °C.
- For longer periods, freeze at -20 °C.
- Avoid hemolyzed, turbid, or sample which contains particulate material.
Precautions for Beta-HCG
- If the test is delayed more than 48 hours, then freeze the samples at -20 °C.
- Don’t repeat thawing and freezing again and again.
- Hemolysis and lipemic serum give a false result.
- Hematuria and proteinuria give a false positive test. I will recommend at least centrifuging the urine.
- This test may be negative in the diluted urine.
- Drugs like diuretics lead to dilution of the urine and may give a false-negative result.
- Some drugs that give false positive tests are anticonvulsants, hypnotics, tranquilizers, and antiparkinson drugs.
Indications for Beta-HCG
- For the diagnosis of pregnancy.
- It can be used during a high-risk pregnancy.
- It can be used for ectopic pregnancy.
- For screening of Down’s syndrome.
- This may be used as a tumor marker in some malignancies.
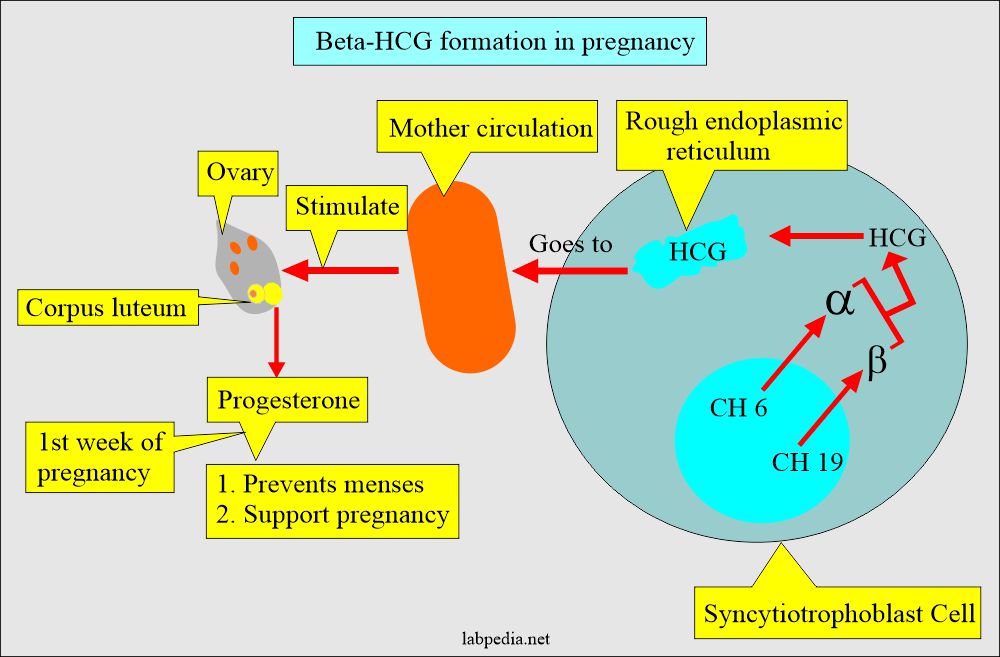
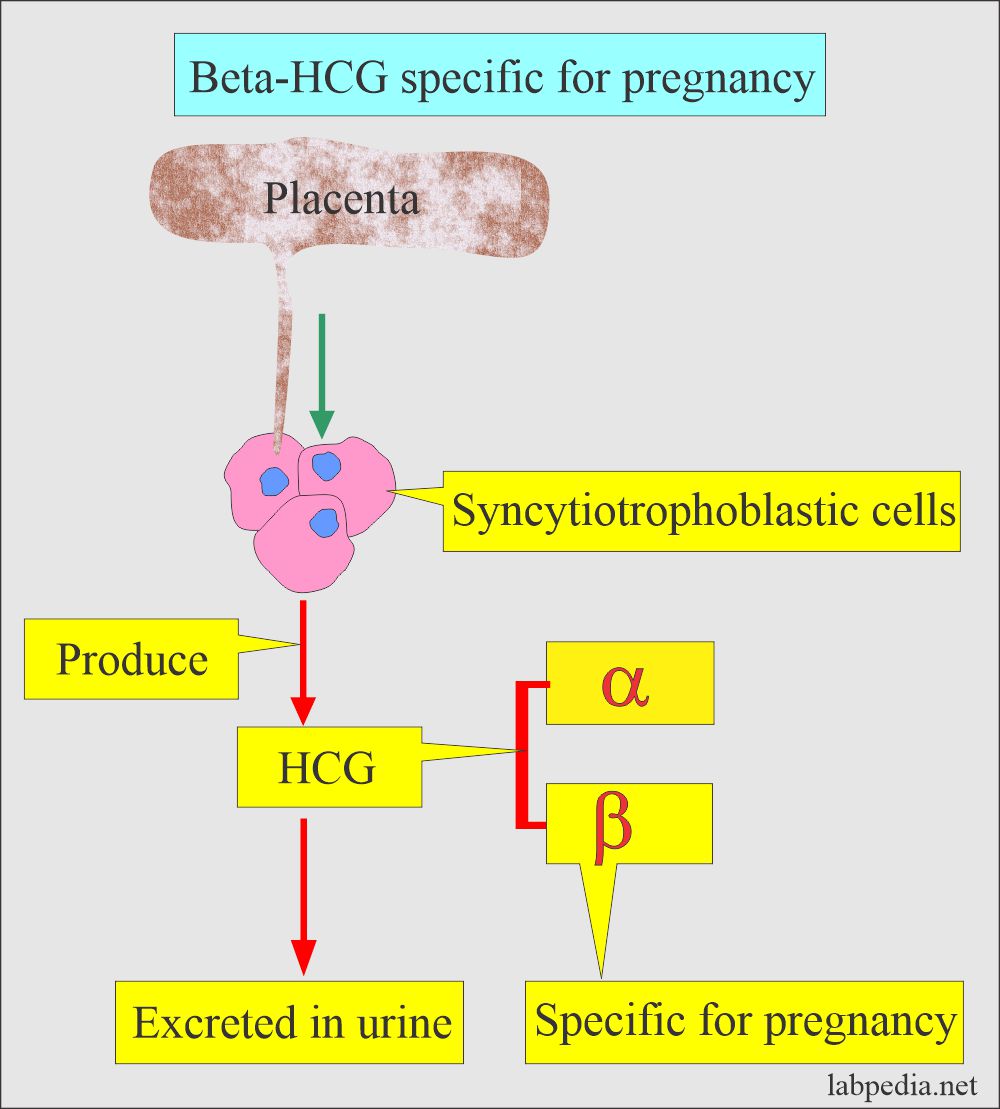
Pathophysiology of Human chorionic gonadotropin (HCG)
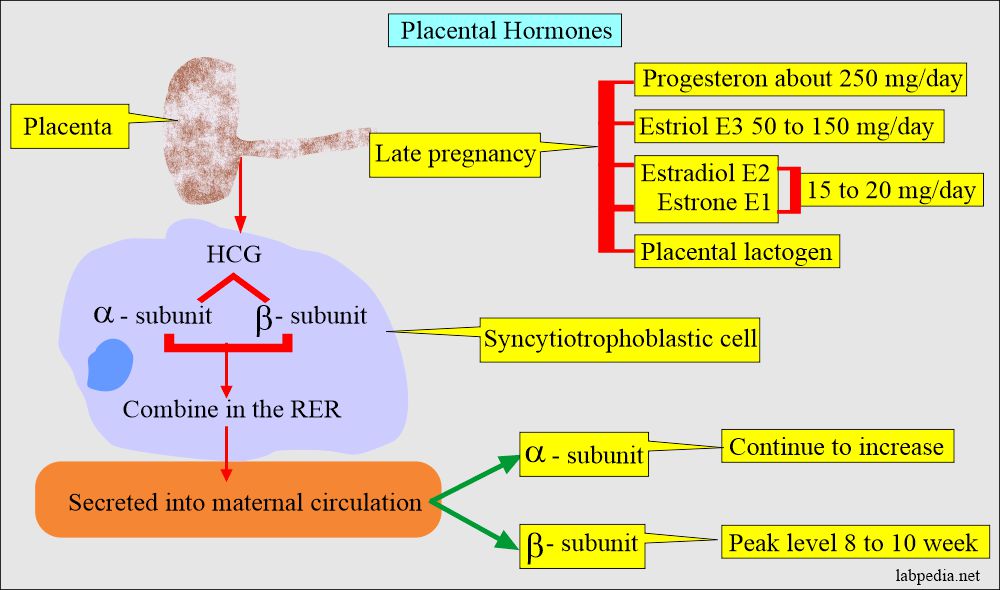
- The placental trophoblastic cells produce an appreciable amount of hormone, human chorionic gonadotropin (HCG).
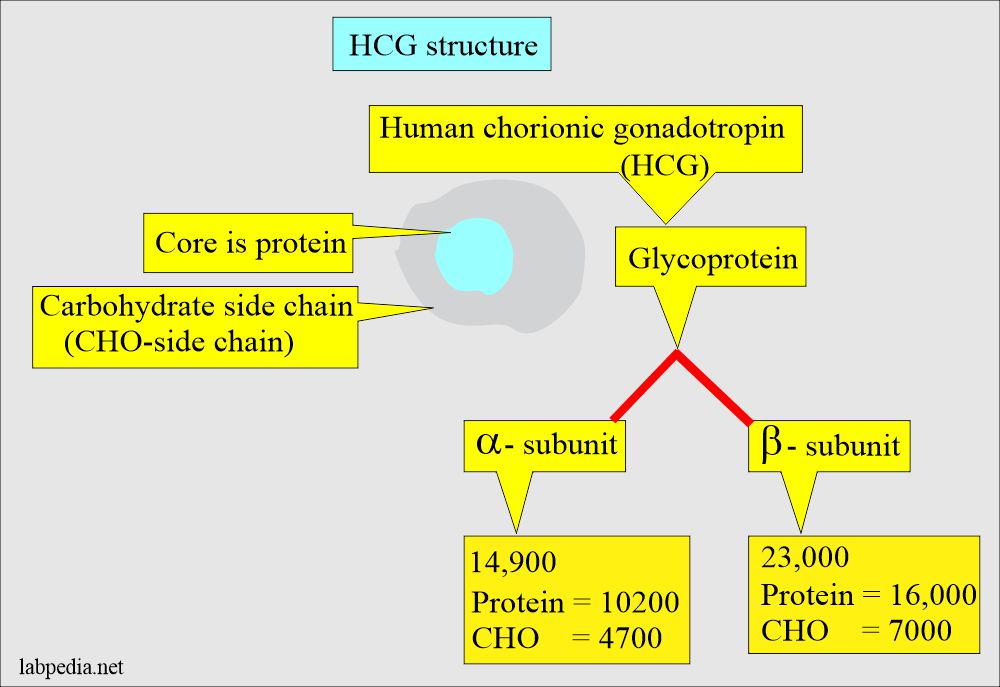
- HCG is a glycoprotein with alpha (α) and beta (β) subunits.
- Molecular weight is 37,900 D and has a high carbohydrate proportion than any other hormone.
- This is synthesized in the syncytiotrophoblast of the placenta.
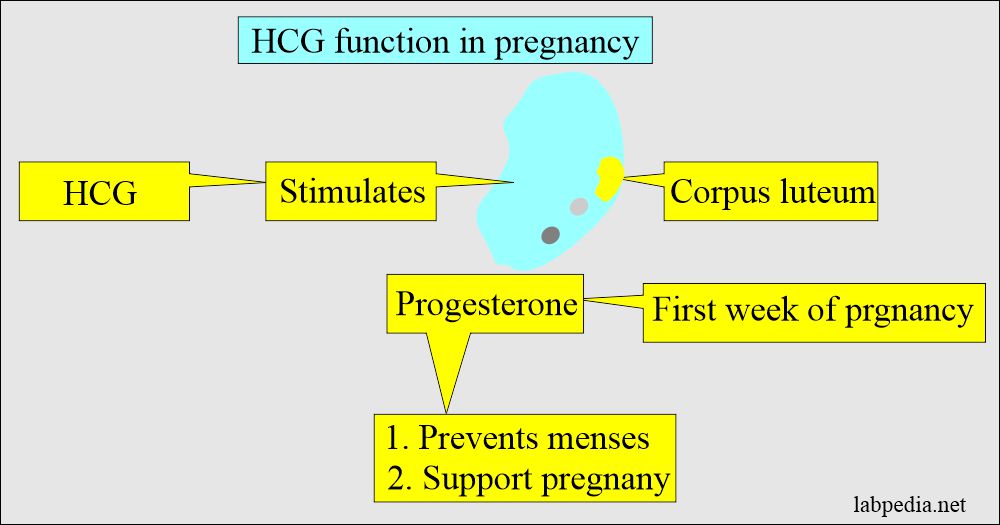
- HCG stimulates the corpus luteum to produce progesterone which maintains the pregnancy.
- This hormone is excreted in the urine.
- HCG is present in the blood and urine.
- HCG appears as early as the 10th day of fertilization or conception.
- In the first few weeks of the pregnancy, HCG rises markedly, and the serum levels are higher than the urine.
- After about one month, the HCG levels are the same in the serum and urine.
- This hormone is negative in the urine of men and nonpregnant women.
- <5% of the female may show a minute amount of HCG.
HCG consists of the following:
- Alpha subunit (α-HCG). This is the same for all the glycoprotein hormones. This is also part of pituitary hormones.
- α-HCG has a molecular weight of 14,900, where protein is 10200 and carbohydrates are 47,000.
- Beta subunit (β-HCG). This is specific to the HCG. This gives immunologic and biologic specificity. The β-HCG has antigenic individuality.
- β-HCG has a molecular weight of 23,000, where the protein portion is 16,000 and carbohydrates are 7000.
- Free β-subunit and intact β-subunit HCG are measured in most of the current methodologies.
- The β-HCG unit is specific for a pregnancy test.
- This test becomes negative after delivery in 3 to 5 days.
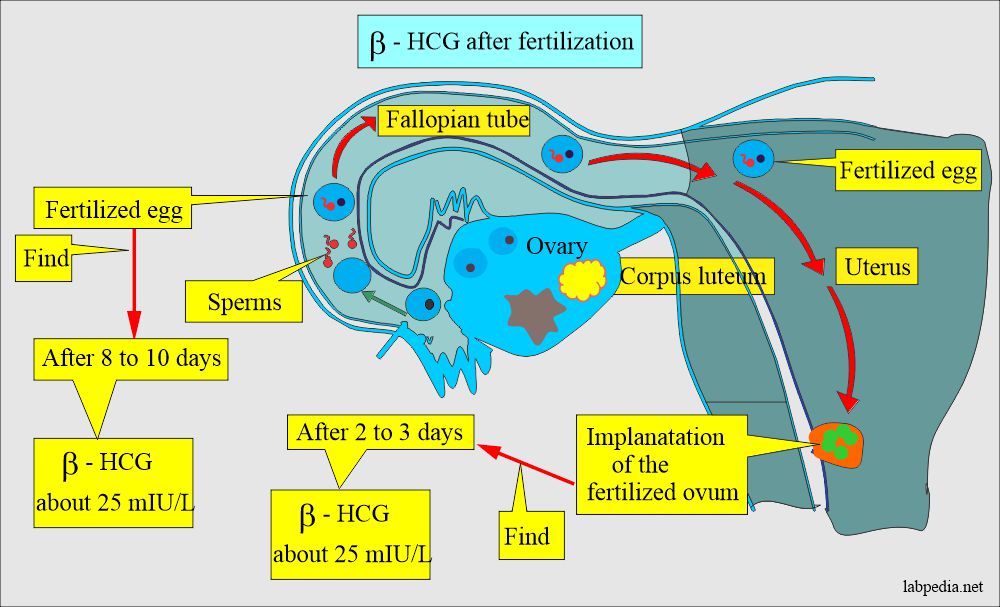
- β-HCG in blood detects pregnancy as early as 6 to 10 days after the implantation of the oocyte.
- This will be positive after 14 days of the last cycle in the urine.
- In a normal pregnancy, one can find 25 mIU/mL after 2 to 3 days of implantation and after 8 to 10 days of fertilization.
- The qualitative test detects pregnancy.
- This has less sensitivity (20 to 50 IU/L) than the quantitative test.
- This will be negative in the first week of the menstrual cycle.
Normal pregnancy
- A normal pregnancy lasts approximately 40 weeks, measured from the first day of the last normal menstrual cycle.
- Normal pregnancy is divided into three trimesters. Each trimester is slightly longer than 13 weeks.
- The first trimester, o to 13 weeks, begins on the first day of the last menses.
- Ovulation occurs on approximately the 14th day of the regular menstrual cycle.
- The fertilization occurs in the fallopian tubes and becomes a zygote carried down the tube into the uterus.
- The zygote divides and becomes morula.
- The morula develops a cavity, the primitive yolk sac, and becomes a blastocyst, which implants in the uterine wall about 5 days after fertilization.
- The cells on the exterior wall of the blastocyst become trophoblasts, which invade the uterine endometrium and develop into chorionic villi, creating the placenta.
- Now, these products of conception are referred to as an embryo.
- A cavity called the amnion forms within the embryo and enlarges with the accumulation of liquor amnii, usually called as amniotic fluid.
- From the combination of three primary cells named:
- Endoderm.
- Mesoderm.
- Ectoderm.
- Now the organs will start to develop; this process is called organogenesis.
- In the 10th week, the embryo is formed, where most major organs are developed, and now it is called a fetus.
- In the 13th week, the fetus weighs approximately 13 grams and is 8 cm long.
- During the second trimester, 13 to 26 weeks, the growth of the fetus is rapid. The fetus weighs around 700 grams, is 30 cm long, and many organs begin to mature.
- During the third trimester, 26 to 40 weeks, maturation of the organs is complete, weight is 3200 grams, and is about 50 coms long.
- Now the term is 37 to 40 weeks; normal labor starts with the rhythmic contraction of the uterus.
Stages of normal pregnancy and development of fetus:Clinical features First trimester Second trimester Third trimester Time period 0 to 13 weeks 13 to 26 weeks 26 to 40 weeks Weight 13 grams 700 grams 3200 grams Length 8 cms 30 cms 50 cms Organs development Embryo (Fetus), three epithelial layers Organs start maturing Maturation of organs is complete
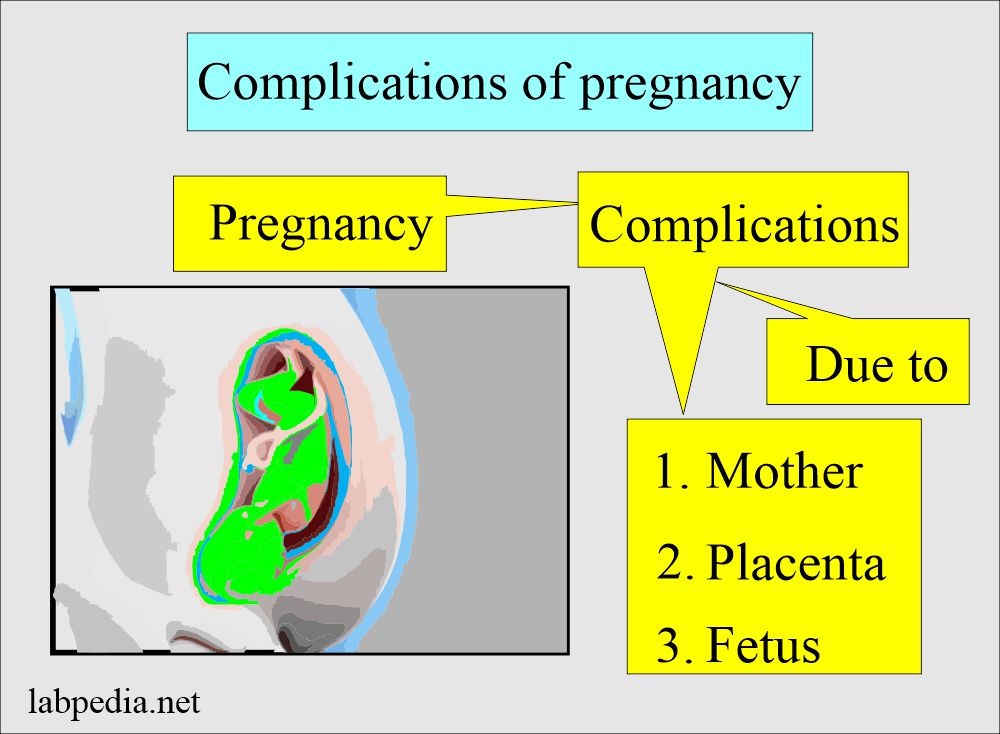
Complications of the pregnancy:
- Most of the pregnancy progress without any complications. The most common causes can arise from the mother, placenta, or fetus.
Complications arising from the mother are:
- Ectopic pregnancy.
- Hyperemesis graviderum.
- Preeclampsia.
- Liver diseases.
- Isoimmunization by the blood groups is a hemolytic disorder.
- Grave’s disease.
- HELLP syndrome (H =hemolysis, EL = elevated liver enzymes, LP = low platelets count).
Abnormalities of the placenta are:
- Molar pregnancy (Hydatidiform mole).
- 5% of the partial mole transforms into choriocarcinoma.
- 20% of the complete mole transforms into choriocarcinoma.
- Rarely choriocarcinoma.
Complications due to the fetus are:
- Neural tube defect.
- Down’s syndrome.
- Trisomy 18.Preterm delivery.
- Preterm delivery.
- Presence of fetal fibronectin.
- Fetal respiratory distress syndrome.
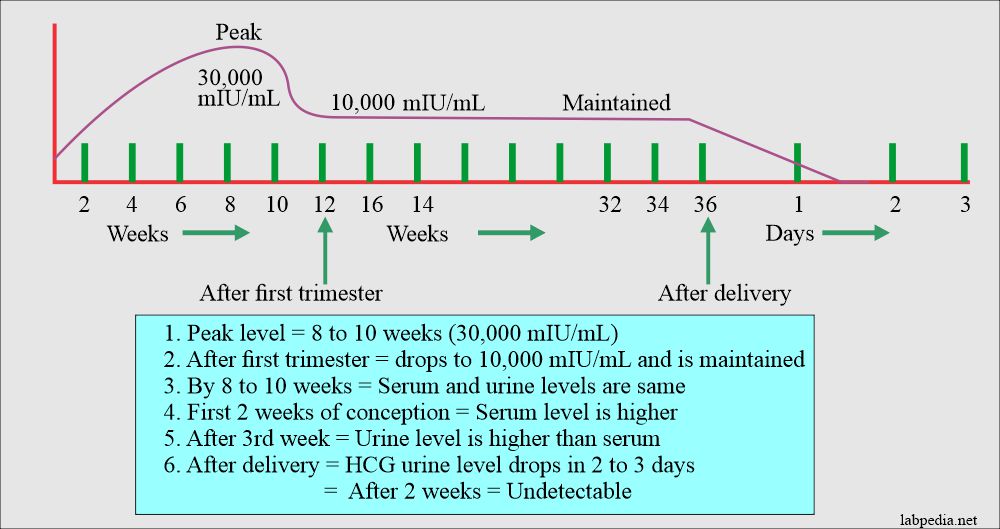
Normal HCG level During Pregnancy
- Negative in nonpregnant women.
- Positive in pregnant women.
- The blood test is positive after 11 days of conception.
- This test may become positive as early as 4 days after the expected date of menstruation.
- Or pregnancy is detected 8 to 14 days after the first missed menstrual cycle, and the positivity is 95%.
- The blood test is positive after 11 days of conception.
- The urine test is positive after 12 to 14 days of conception (fertilization).
- The peak level by 8 to 11 weeks of pregnancy, in another reference peak level, is at the 60th to 70th day of pregnancy, then starts to drop progressively.
- The peak level in serum and urine at the 8th to 10th week of gestation is around 30,000m IU/mL.
Normal values of HCG in the pregnancy:
| Detectable level | HCG mIU/mL |
| 6 to 8 days of conception | level around 10 to 15 |
| Double every 3 days | 1200 to 6000 |
| Double every 4 days | 6000 to peak level |
| 10 to 12 weeks | 150,000 to 200,000 |
| At the end first trimester | around 100,000 |
| By the early second trimester | the peak level is 10,000 (800ng/mL) |
| 2n trimester | 10,000 to 50,000 |
| 3rd trimester | 10,000 to 50,000 |
| After delivery until 2 weeks | detectable |
| Ectopic pregnancy | no normal dynamics of HCG (Abnormal) |
- To convert into SI units x 1.0 = IU/L
Source 2
HCG
- Qualitative = Negative
- Pregnancy = Positive
- Male and nonpregnant females = <5 mIU/mL
Quantitation of HCG
| Gestation week | Whole HCG mIU/mL |
| <1 | 5 to 50 |
| 2 | 50 to 500 |
| 3 | 100 to 10,000 |
| 4 | 1000 to 30,000 |
| 5 | 3500 to 115,000 |
| 6 to 8 | 12,000 to 270,000 |
| 12 | 15,000 to 220,000 |
β-HCG Normal
- <2 ng/mL
- Or <5 mIU/mL
Types of pregnancy diagnostic tests:
Biologic test on urine.
- These tests are not used now. These are of historical importance.
- In this test, the urine of the suspected lady is injected into an animal like a rabbit, mouse, or frog. These animals develop the corpus luteum.
- Then these animals were sacrificed, and a search was done for the corpus luteum.
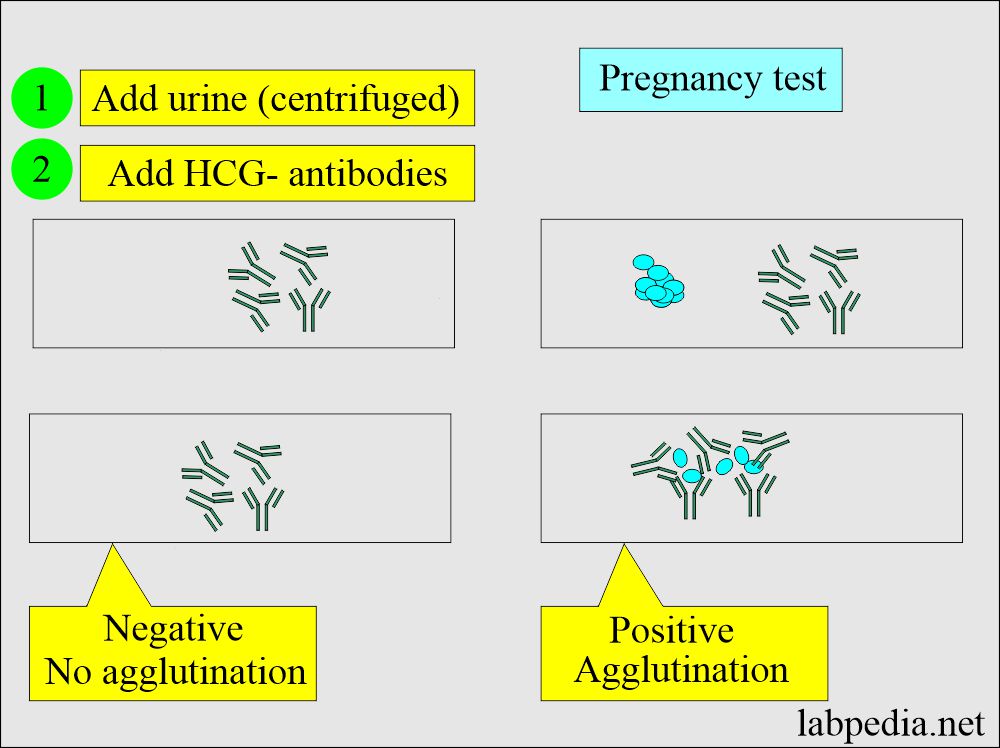
Immunologic tests.
- These are agglutination inhibition tests done on urine and blood.
- In this test, antibodies against HCG are produced, and the test can be done in 2 min or, in some kits, 2 hours.
- These have a high false-positive rate, so the test should be done after 28 days of the last menstrual cycle.
- The false-negative test may be seen when the HCG level is less than 25 to 50 IU/L.
- The false-negative test may be seen if the urine contains the following:
- Protein.
- Drugs.
- Bacteria contamination.
- White blood cells or RBCs.
- The false-negative result may be seen if the reagents:
- Kept at the extreme of the temperature.
- Extreme urine pH.
- Expired reagents.
- Now some of the improved kits can detect after 18 days.
Monoclonal antibody-based test:
- The monoclonal antibody against HCG can detect a small amount of the HCG even after 3 to 7 days after conception.
- Limitations of monoclonal antibody-based tests:
- These are not quantitative tests and may miss, not find early pregnancy or any other abnormality.
- Always run a positive control. The standard usually contains a small amount of HCG.
- Routine tests needed in a normal pregnancy for the evaluation of the fetus’s survival and abnormality:
Tests needed during the pregnancy:
| Test needed in pregnancy | Value in pregnancy | Interpretations/Complications |
| HCG level | >10 IU/L |
|
| Screening in the first trimester (free β-HCG, Pregnancy-associated plasma protein) | Depending upon various factors |
|
|
Quad screening in 2nd trimester (HCG, AFP, Estriol, and Inhibin) |
Depending upon various factors | To assess for:
|
| Hematocrit (Hct) | 36% to 48% |
|
| Blood grouping | Type A, B, AB, and O |
|
| Rh typing |
|
|
| Antibody detection | It should be negative |
|
| Toxoplasmosis IgG | Negative |
|
| Rubella IgG | If positive indicates immunity |
|
| Treponema pallidum testing | Should be negative |
|
| Cervical smear and culture for gonorrhea | Should be negative |
|
| Cervical smear and culture for Chlamydia | Should be negative |
|
| HB surface antigen (HBS-Ag) | Should be negative |
|
| HB surface antibody (HBS-Ab) | Positive (Immune) status |
|
| HIV | Should be negative |
|
| Group B Streptococcus | Should be negative |
|
Effects of Pregnancy on different biochemical parameters:
| Lab tests | Effect of pregnancy | Explanation |
| Hematocrit | It is decreased | It is due to an increase in the plasma volume |
| Coagulation factors |
|
|
| BUN | It has a mild decrease | There is an increase in the glomerular filtration rate |
| Creatinine | There is a mild decrease | There is an increase in the glomerular filtration rate |
| Alkaline phosphatase (ALK) | It is increased | It is due to an increase in the production of placental heat-stable ALK |
| Triglycerides | It is increased | |
| Cholesterol | It is increased | |
| 1,25 dihydroxy vitamin D | It is increased | It is due to increased calcium and transfer of Ca++ to the fetus |
| Parathyroid hormone | It is increased | In this case, ionized Ca++ remains normal |
| T3 and T4 | These are increased | But the patient is euthyroid |
| Thyroxin binding globulin | it is increased | Patient is euthyroid |
Interpretations, Differential Diagnosis, of Positive pregnancy test:
- HCG is present in the pregnancy.
- HCG may also be seen in 65% of the Ectopic pregnancy.
- A level of 20 IU/L or less subunit within the first week of pregnancy indicates ectopic pregnancy because there are insufficient trophoblastic cells.
- Hydatidiform mole.
- Choriocarcinoma.
- Germ cell tumors of the ovary and testes.
- HCG may be produced in primary liver cell carcinoma.
False-positive pregnancy test:
- This can happen in 2% to 5% of the cases.
- This may be seen due to interfering substances like:
- Proteins (proteinuria).
- Drugs like chlorpromazine, phenothiazine, and methadone.
- Bacteria infection.
- RBCs or WBCs (hematuria and pyuria).
- Cross-reactivity with pituitary gonadotropins, e.g., a high level of LH in postmenopausal women.
Negative pregnancy test:
- Dead fetus.
- Threatened Abortion.
- There is a sudden drop in the level of the plateau.
- Incomplete abortion.
False-negative tests:
- These are common because usually, the kits detect HCG levels at the concentration of 1000 to 2000 mIU/L.
- Therefore, these qualitative tests will not be positive until 8 to 14 days after the first missed menstrual cycle.
- These qualitative tests may not detect normal pregnancy even after the second trimester (when HCG levels are low).
- These tests may be negative in an ectopic pregnancy (when HCG levels are low).
- Use of the old reagents.
- In case the antiserum-HCG is denatured by the temperature or change in the pH.
- It may be negative in the diluted urine with low specific gravity.
- The sample was taken too early in the pregnancy.
Low HCG levels indicate:
- There may be a miscarriage.
- Maybe blighted ovum.
Positive HCG tests can be seen in the following:
- Pregnancy.
- Ectopic pregnancy (it is positive in 65% of the cases).
- Hydatidiform mole.
- In males with testicular germ cell tumors (choriocarcinoma and embryonal cell carcinoma).
- In a female with ovarian germ cell tumors (choriocarcinoma and embryonal cell carcinoma).
- Liver cell carcinoma (hepatoma) can also make HCG.
Pregnancy test interpretation for the layman:
- Remember if there are missed menstruation cycles and delayed more than one week. Then ask for the morning sample for a pregnancy test.
- If it is negative and there is no menstruation, repeat the pregnancy test after 6 to 7 days.
- If still negative, then advise for the ultrasound of the abdomen, including the uterus.
NOTE: Please see more details on the beta-HCG level.