Fluid Analysis:- part 6 – Pleural Fluid Aspiration procedure (Thoracentesis)
Pleural Fluid Aspiration procedure (Thoracentesis)
What sample is needed for Pleural Fluid Analysis?
- The sample is aspirated from the pleural cavity.
What are the indications for Pleural fluid aspiration (Thoracentesis)?
- This may be diagnostic.
- Or maybe therapeutic to relieve the pain and dyspnoea.
- Gram and AFB stain may be done.
- It is used for culture.
- It can be used for the PCR for the diagnosis of tuberculosis.
- It may be done in case of malignancy.
- Autoimmune diseases like systemic lupus erythematosus (SLE).
- Inflammation of the pancreas, like pancreatitis.
- In the case of pneumonia.
- Empyema (pus in the pleural space).
What are the contraindications for Pleural fluid aspiration?
- Avoid in case of thrombocytopenia.
- Avoid in patients with bleeding tendency.
- In case the volume is too small.
- If the patient has a bleeding tendency.
- If there is a skin disease in the area of the puncture.
- If the patient is on anticoagulant therapy.
- There are chances for infection.
- Chances of liver or spleen injury.
How will you define pleural fluid?
- The pleural fluid is obtained from the pleural cavity, between the parietal pleural membrane lining the chest wall and the visceral pleural membrane covering the lungs.
- Pleural fluid may be:
- Exudate is mostly due to infections or neoplastic processes.
- Other conditions like collagen diseases, trauma, pulmonary infarction, and drug hypersensitivity may cause exudate.
- Transudate is due to congestive heart failure, nephrotic syndrome, hypoproteinemia, and cirrhosis.
- The most common cause is congestive heart failure.
How will you define thoracentesis?
- It is the removal of the fluid or air from the pleural cavity.
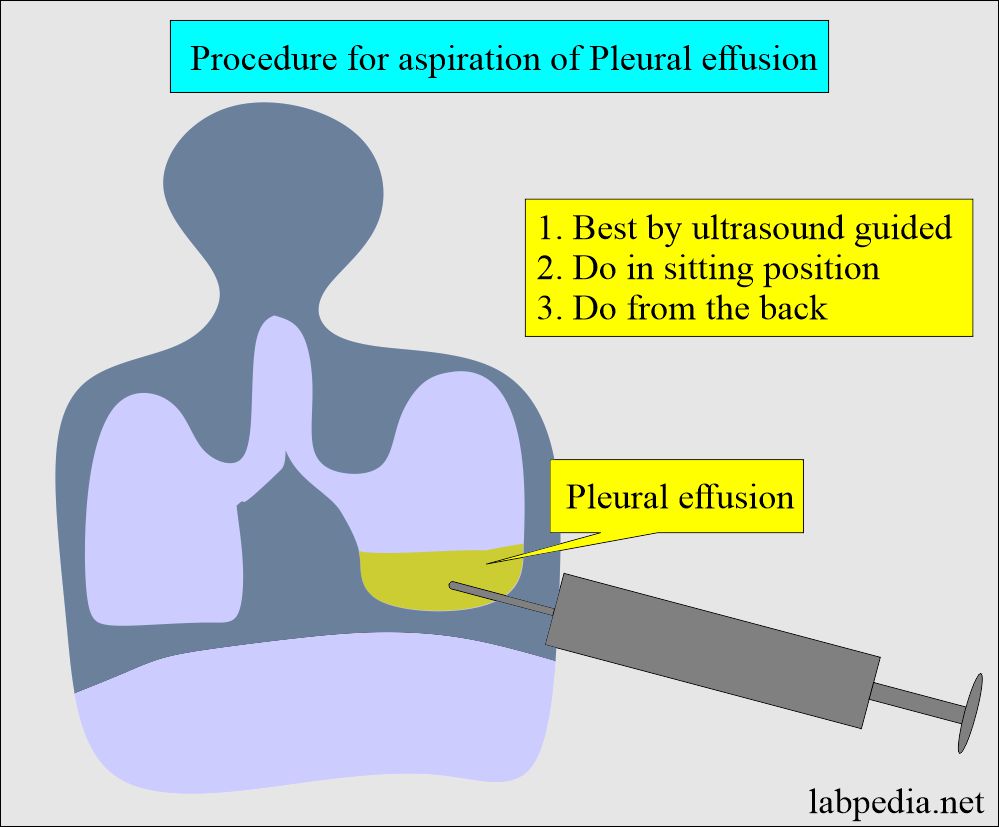
How will you perform the Procedure for thoracentesis?
- Make the chest X-ray available near the patient’s bedside to see the location of the fluid.
- Give the sedative to the patient if necessary.
- Expose the chest.
- This is better to do ultrasonography-guided aspiration.
- The patient will be in a sitting position.
- Give local analgesia.
- Do the percussion and mark the upper level of fluid.
- Ideally, it is done on the posterior side, roughly 10 cm from the spine.
- Enter the syringe below 1 to 2 intercostal spaces from the upper border.
- Withdraw at least 40 mL of the fluid. It is preferable to take 300 mL to 1000 mL.
- Collect the sample in a clean container (maybe sterile).
- You can add heparin if necessary, particularly when the fluid is bloody. Heparin 5 to 10 U per mL of the fluid.
- Send the sample immediately to the lab; if it is delayed, then refrigerate the sample.
Pleural Fluid Analysis: Pleural fluid aspiration procedure (Thoracentesis)
What is the gross appearance of Pleural Fluid in various diseases?
- In the case of empyema, it has a foul odor and a thick and pus-like appearance.
- Chylothorax fluid is opalescent and pearly fluid.
- The chylous fluid contains a high concentration of triglycerides and a positive Sudan III stain.
- Pseudochylous fluid contains a high concentration of cholesterol and cholesterol crystals.
What is the difference between chylous and pseudochylous pleural fluids?
| Characters featured | Pseudochylous fluid | Chylous fluid |
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
- How to differentiate hemothorax and hemorrhagic exudate:
- Advise hematocrit (Hct) on the pleural fluid:
- In the case of hemothorax = Hct is similar to the blood.
- In chronic membranous disease, fluid = Hct will be much lower.
- Advise hematocrit (Hct) on the pleural fluid:
| Appearance | Clinical significance |
|
|
|
|
|
|
|
|
What are the microscopic examination findings of pleural fluid?
- Total cell count:
- The cell count >1000 /mL suggests exudate.
- Polys indicate an acute inflammatory condition like pneumonia, early tuberculous effusion, and pulmonary infarction.
- If >50% of white cells are lymphocytes, it indicates tuberculosis or neoplasm.
- The presence of RBCs indicates neoplasm, intrathoracic bleeding, or malignancy.
What is the significance of the various cell types in the pleural fluids?
| Type of the cells | Significance of the various types of cells |
|
|
|
|
|
|
|
|
|
|
|
|
What are the biochemical findings of pleural fluid?
- Protein:
- >3 g/dL indicates exudates.
- <3 g/dL indicates transudates.
- Albumin gradient is a better factor than total protein.
- Albumin gradient = Pleural albumin – serum albumin.
- A value 1.1 g/dL or more indicates transudate.
- Value <1.1 g/dL indicates exudate.
- Total protein ratio = Fluid total protein – serum total protein
- If the ratio is >0.5, it indicates exudate.
- pH:
- Normal pH = 7.4
- <6.0 indicates an esophageal rupture and allows the influx of acid or gastric fluid from the stomach.
- >7.4 indicates malignancies.
- Pleural fluid pH <7.3 may indicate the need for chest tube drainage and antibiotics in case of pneumonia.
- Glucose:
- The glucose level is like a serum glucose level.
- Glucose <60 mg/dL may be seen in:
- Tuberculosis.
- Malignancy.
- Rheumatoid arthritis.
- Empyema.
- Amylase:
- This may be elevated in malignant tumors.
- It will be raised in case of pancreatitis, and this amylase may be the first to be raised in the pleural fluid.
- Rupture of the esophagus with leakage of salivary amylase.
- Lactate dehydrogenase (LDH):
- Pleural fluid LDH / serum LDH if >0.6 is seen in the exudate.
- Triglycerides:
- This is done to diagnose chylous pleural effusion.
- In the chylous fluid, triglycerides are >110 mg/dL.
What is the significance of the chemicals in the pleural fluids?
| Chemical parameter | Significance in various diseases |
|
|
|
|
|
|
|
|
|
|
|
|
- Carcinoembryonic antigen (CEA):
- CEA is raised in case of pleural effusion due to GIT malignancy.
- This may be raised in the case of breast carcinoma.
- Exudate:
- Pleural fluid cholesterol >60 mg/dL.
- Pleural fluid cholesterol: serum cholesterol = >0.3
- Pleural fluid bilirubin: serum bilirubin = 0.6 or more.
- Transudate:
- Proteins are <3 g/dL.
What is the microscopic examination of pleural fluid?
- Cytology:
- This will be positive in 50 to 60% of the malignant pleural effusion.
- The most common site is the lungs and breast.
- The third common cause is lymphoma.
- In the case of pleural fluid, you may see staphylococcus aureus, Enterobacteriaceae, anaerobes, and mycobacterium tuberculosis.
- Advice:
- Gram stain.
- Culture.
- AFB stain.
- Gram stain and culture:
- Advise gram stain before starting the antibiotics.
- Advise culture for tuberculosis, and this may take 4 to 6 weeks.
- Advice for fungal culture because this may cause pleural effusion.
- Immunologic tests: It differentiates pleural effusion from the immunologic and non-inflammatory processes.
- The most common tests advised are an anti-nuclear antibody (ANA) and Rheumatoid factor.
What are the normal Pleural fluid findings?
Source 2
| Characteristics | Values |
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
Questions and answers:
Question 1: What is the significance of CEA in pleural fluid?
Question 2: What is the normal pH of the pleural fluid?
