Platelets – Part 2 – Platelets Count (Thrombocyte count)
Platelets Count
What sample is needed for Platelets Count?
- This can be done on EDTA blood.
- This is stable for 5 hours at 23 °C and 24 hours at 4 °C.
- Take capillary blood and dilute directly; this sample is stable for 3 hours.
- Fetal blood is collected from the umbilical area percutaneously.
- The platelets can be assessed on the DLC slide as well.
What are the indications for platelet count?
- To diagnose the cause of petechial bleeding in the skin.
- To find the cause of spontaneous bleeding.
- In women with heavy menses.
- This is advised in a patient on chemotherapy.
- This is advised in case of bone marrow failure.
- Platelets count is of value in thrombocytopenia seen in:
- Uremia.
- Liver diseases.
- Malignancies.
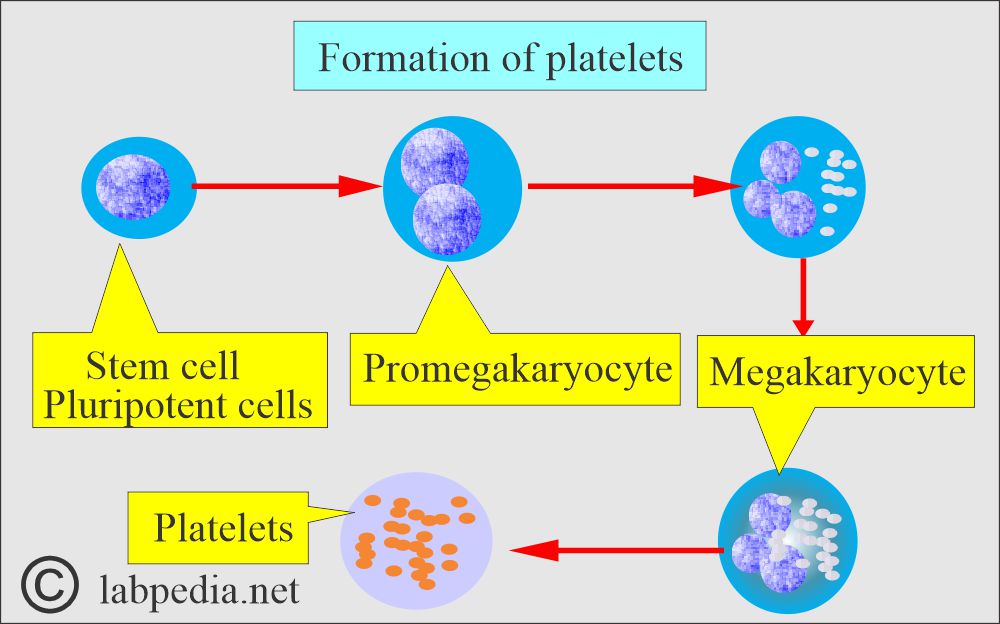
How is the Formation of Platelets?
- Platelets are the smallest form of formed elements of blood.
- The megakaryocytes in the bone marrow form platelets. These are the detached portions of the megakaryocytes.
- Platelets are the smallest of the formed elements of blood.
- Platelets measure 3.0 x 0.5 µm in diameter.
- These are non-nucleated, small, round, or oval, flattened disk-shaped structures.
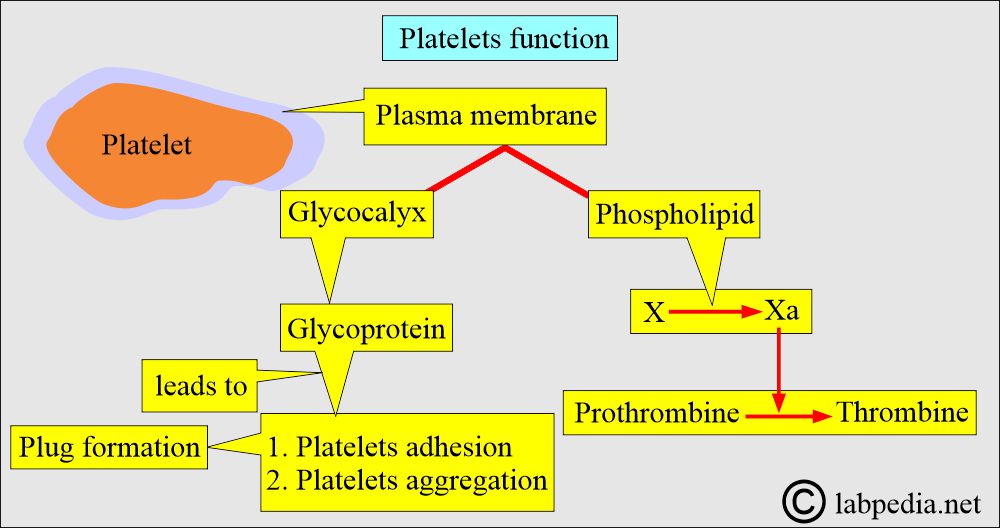
What are the functions of Platelets?
- The glycoprotein of the platelet surface is important in the platelet reactions of:
- Adhesion.
- Aggregation.
- Leading to plug formation during hemostasis.
- Glycoproteins are:
- Glycoprotein 1a.
- Glycoprotein 111a.
- Glycoprotein 1b.
- Glycoprotein 11b.
- The binding site for 11b/111a is a receptor for fibrinogen, which is important in platelet aggregation.
- The membrane phospholipids known as factor 3 are important in converting coagulation factor X to Xa and prothrombin (factor 11) to thrombin (factor 11a).
- Platelet activity is needed for:
- Blood clotting.
- Vascular integrity.
- Vasoconstriction.
- In hemostasis, the steps are:
- Platelet aggregation that occludes the breaks in the vessel wall.
- Initiates the clotting mechanism.
How are the platelets distributed in the body?
- The lifespan of platelets is roughly 7.5 days.
- Of platelets, two-thirds are in the blood, and one-third are in the spleen.
What are the contents of platelets?
- The glycocalyx is the outer membrane.
- α-Granules.
- Lysosomes contain neutral proteases, bactericidal enzymes, and acid hydrolases.
- Dense granules contain ADP, ATP, and Calcium.
- β-thromboglobulin functions are:
- Inhibits heparin.
- It is chemotactic.
- Promotes smooth muscle growth for the repair of vessels.
- Platelet factor 4, inhibits heparin.
- Platelet-derived growth factor (PDGF) functions are:
- It promotes smooth muscle growth.
- It takes part in atherosclerosis and lipid metabolism.
- Thrombospondin functions are:
- It mediates cell-to-cell interaction.
- It promotes platelet-to-platelet interaction.
- Fibrinogen leads to fibrin formation.
- Von Willebrand factor (VWF) promotes platelet adhesion.
- Factor V is a cofactor in fibrin formation.
- Factor VIII is also a cofactor for fibrin formation.
- Fibronectin functions are:
- It is a cellular adhesion molecule.
- It promotes platelet spreading.
- Plasminogen is the precursor to plasmin and has a function in fibrinolysis.
- High molecular weight Kinogen has a role in activating the intrinsic pathway via contact.
- α2-Antiplasmin inhibits plasmin.
How will the Platelets be activated?
- This may be transient, reversible, or irreversible.
- After activation, the changes are:
- Initially, there is a pseudopod formation.
- There is a contraction.
- Adhesion.
- Change in shape.
- There is a stickiness.
- There is aggregate formation.
- There is a platelet plug formation.
- There is the release of chemical secretions.
- The last step stabilizes the platelet plug by forming a fibrin mesh over the platelet aggregates.
What is the normal platelet count?
Source 1
| Age | x 103/µL |
| Fetal blood | |
| 18 to 20 weeks | 242.1 ± 34.5 |
| 21 to 22 weeks | 258.2 ± 53.6 |
| 23 to 25 weeks | 259.4 ± 42.4 |
| 26 to 30 weeks | 253.5 ± 36.6 |
| Adult | 150 to 400 |
- To convert into SI unit x, 106 = x 109/L
Source 2
| Age | cmm (mm3) | x 109/L (SI unit) |
| Adult/elderly | 150,000 to 400,000 | 150 to 400 |
| Premature infants | 100,000 to 300,000 | 100 to 300 |
| Newborn | 150,000 to 300,000 | 150 to 300 |
| Infants | 200,000 to 475,000 | 200 to 475 |
| Children | 150,000 to 400,000 | 150 to 400 |
- Thrombocytopenia occurs when the count is less than 100,000 /cmm.
- Thrombocytosis occurs when the count is more than 400,000 /cmm.
- Thrombocythemia occurs when the count is above one million /cmm.
What are the Methods for counting platelets?
- By automated hematology analyzers.
- Direct smear also gives information about platelets’ size, shape, and clumping.
- Direct count from the peripheral blood smears.
- Count platelets on an oil objective in 10 fields and multiply by 2000, which gives a rough idea of the count.
- Platelets in 10 field X 2000 = Total platelets.
What is the manual method of platelet count?
- Take 20 µL of blood.
- Add 1.8 mL of 1% ammonium oxalate.
- Ammonium oxalate will lyse the RBCs and WBCs, while Platelets will remain intact.
- Leave for 15 minutes to complete the lysis of RBCs.
- Mount the Neubauer chamber.
- Leave the chamber for 15 minutes in high humidity.
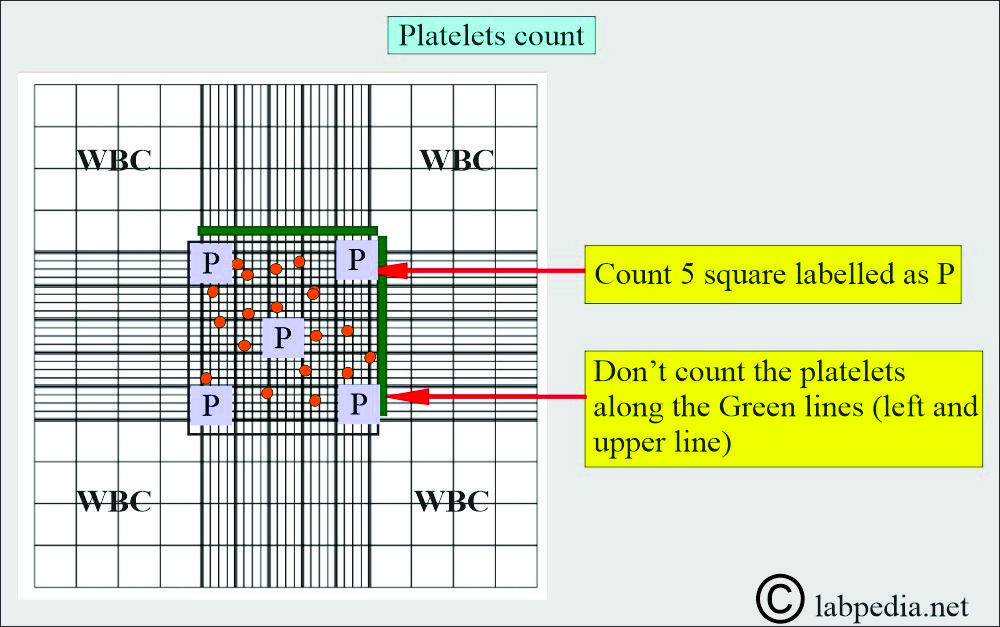
- Count the large central square labeled as P.
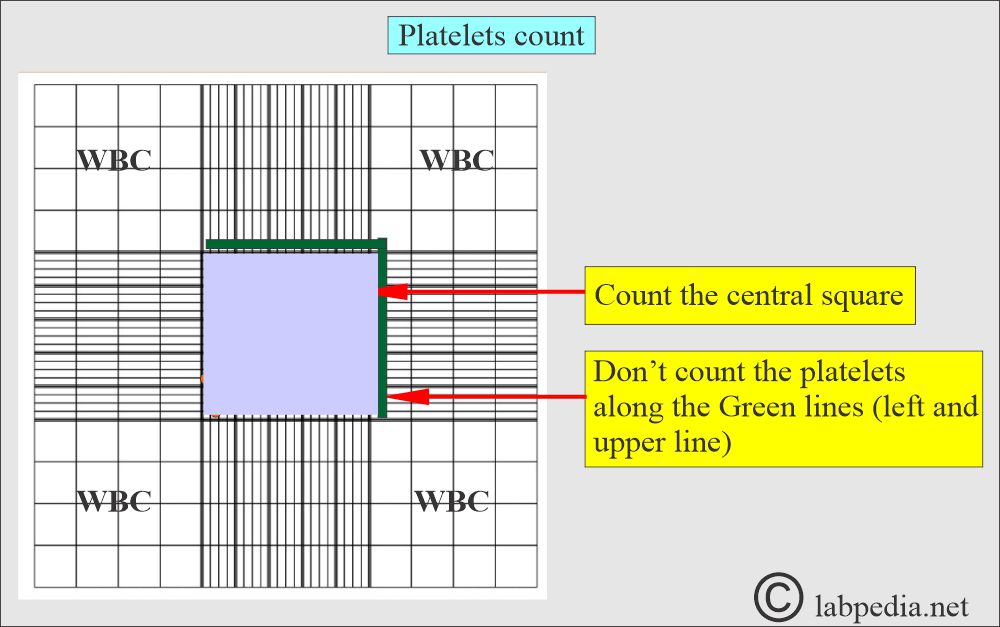
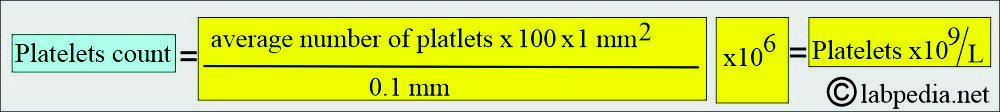
Platelet count in the chamber
- How will you calculate the platelets?
- Area of 5 squares in the central area = 0.2 sq. mm
- The depth of the chamber is 0.1 mm.
- The volume of 5 squares in the central area = 0.2 x 0.1 µL = 0.02 µL
- Dilution of the blood sample = 1:20
- If P number of platelets is counted in 0.02 µL
- The number of platelets /µL = P x 20 x 1/0.2
- = P x 20 x 50
- = P x 1000
- Note: You can use the constant factor of 1000.
What is another method of platelet counting?
- Under 400x magnification while adjusting the light.
- Count all 25 squares in the large central area.
- Duplicate the counting procedure.
- Multiply the counted platelets by 1000 = Total platelet count/cmm.
- Multiply the above number of platelets by 106 to get the count in SI units.
- Example:
- Suppose the platelet count in 25 squares (Central square) = 300 x 1000 = 300,000/cmm
- To convert into SI units = 300,000/cmm x 106
- = 300 x 109/L
What are the sources of errors in platelet counting?
- To minimize the error of counting platelets manually:
- Mix thoroughly, diluting fluid before filling the chamber.
- Avoid platelet clumping.
- Improper dilution.
- Not properly filling the chamber.
- Avoid microclot formation.
- Keep in mind the calculation errors.
- Contaminated counting fluid.
- In case of clumping of the platelets.
- Run the test in duplicate and then get the average of the two results.
- If taking blood from the finger, then don’t squeeze the finger.
- The count is lower on the skin puncture sample than on the venous blood sample.
What is the mechanism of thrombocytopenia?
- This may be due to decreased production of bone marrow. This may be due to the following:
- Bone marrow failure.
- Infiltration of the bone marrow by tumors or fibrosis.
- Destruction or sequestration of the platelets by hypersplenism.
- Antibodies destroy the platelets.
- Destruction of the platelets by infection or drugs.
- Increased utilization of disseminated intravascular coagulation.
- In severe hemorrhage, which leads to loss of platelets.
- A large blood transfusion leads to a dilutional effect.
What are the causes of thrombocytopenia?
- Idiopathic Thrombocytopenia ITP.
- Hypersplenism.
- Anemias are pernicious, aplastic, and hemolytic.
- After a massive blood transfusion
- An infection, such as viral or bacterial,
- Chemotherapy treatment.
- HIV infection.
- Leukemias, carcinoma, and myelofibrosis. This is due to the infiltration of the bone marrow.
- D I C.
- Toxemia of pregnancy, eclampsia.
- Antiplatelet antibody.
- Renal failure.
- Inherited diseases like Wiskott-Aldrich syndrome.
- An autoimmune disease like systemic lupus erythematosus
What are the causes of Thrombocytosis?
- Malignant tumors like leukemia and lymphoma,
- Polycythemia vera.
- Splenectomy.
- Iron deficiency anemia.
- Autoimmune diseases like Rheumatoid arthritis and SLE.
- Hodgkin’s lymphoma
- Chronic pancreatitis and inflammatory bowel disease.
- Tuberculosis.
What is the Critical value of platelets?
- The patient may develop spontaneous bleeding when the platelet count is < 20,000 /cmm.
- Platelet counts > 50,000 /cmm usually show no bleeding.
Questions and answers:
Question 1: What is the level of platelets when bleeding may take place?
Question 2: What is the source of platelets?

Very well written and lucid .
Thanks for the comments.
Very well written and lucid. Useful reference.
Well written explained in a meaningful mannar and very practical.Thank you
Thanks for the comments.