Parathyroid hormone (PTH)
Parathyroid hormone (PTH)
What sample is needed for the Parathyroid hormone (PTH)?
- The serum of the patient is required.
- A fasting sample is preferred.
- Place on ice.
- The serum should be separated immediately because the PTH is unstable at room temperature and even on refrigeration.
- Refrigerate during centrifugation.
- Immediately freeze the sample.
- It can be stored at -20 °C to -70 ° C.
- A lower level is seen if the sample is left at room temperature for 4 hours.
- Also, a lower level is seen if the sample is kept at 4 °C for one day.
- The EDTA plasma is the best choice if the chemical method allows it.
- Simultaneous estimation of total calcium, ionized calcium, and phosphorus is recommended.
What are the Indications for Parathyroid hormone (PTH)?
- This is done to evaluate hypercalcemia or hypocalcemia.
- This is also done to establish the diagnosis of hyperparathyroidism.
- PTH differentiates hyperparathyroidism from Nonparathyroid causes leading to hypercalcemia.
What are the precautions for Parathyroid hormone (PTH)?
- Lipemic serum and hemolysis interfere with the method.
- Some drugs may affect the result and increase PTH value like:
- Anticonvulsants.
- Isoniazid.
- Lithium.
- Rifampicin.
- Steroids.
- Drugs that decrease PTH value are:
- Cimetidine.
- Propranolol.
How would you discuss the Pathophysiology of Parathyroid hormone (PTH)?
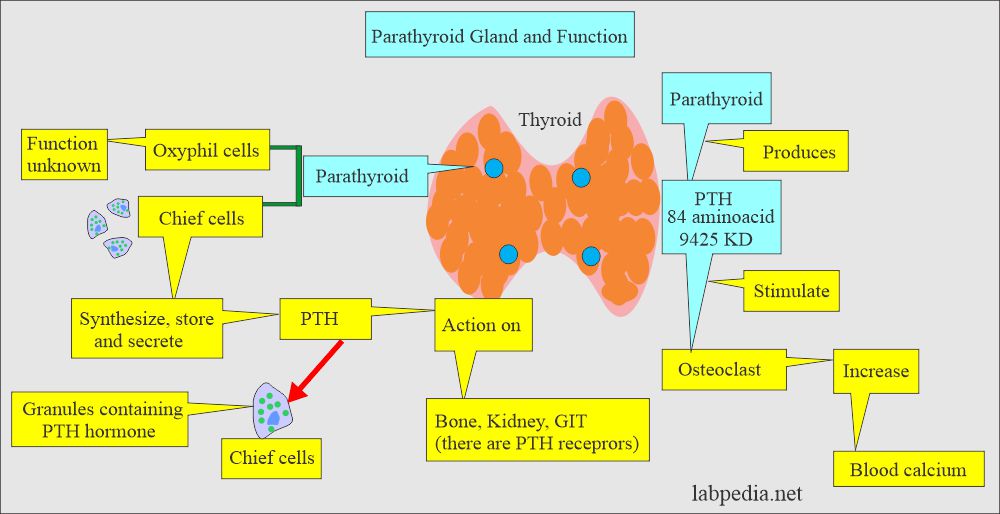
- This is a polypeptide hormone produced in the parathyroid gland.
- The parathyroid glands are 4 in number and present close to or on the posterior surface of the thyroid gland.
- Additional parathyroid glands may be found in the mediastinum (in the thymus gland) or neck.
Where is the formation of the Parathyroid hormone (PTH)?
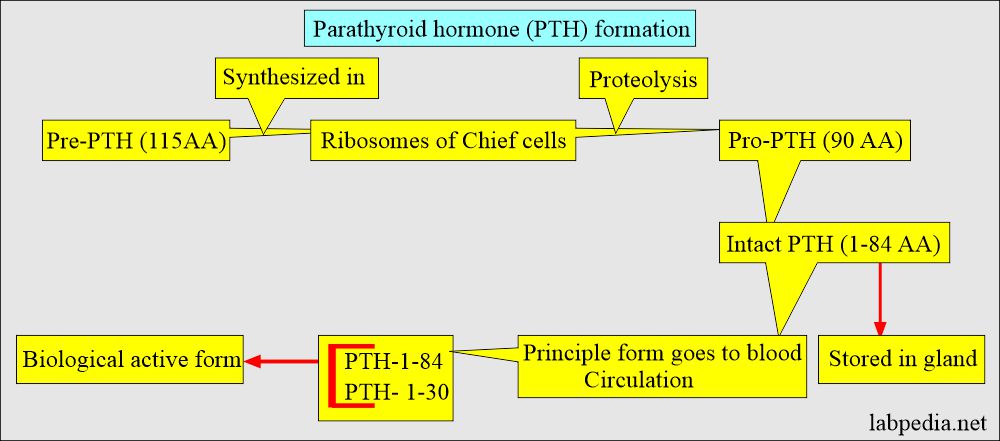
- Preparathyroid (115 AA) is synthesized in the ribosomes of Cheif cells.
- Proteolysis converts the Parathyroid hormone (PTH) into Pro-PTH (90 AA).
- By the second, proteolysis converted into Intact-PTH (1- 84 AA).
- PTH-1-84 is metabolized in the peripheral tissue, mainly the liver and kidney.
- This is stored in the gland, and some go into blood circulation.
- The biological activity of the PTH resides in the first 30 AAs of the N-terminal.
- The concentration of the biologically active form of PTH in blood circulation is very low (10 pmol/L or 0.1 ng/mL).
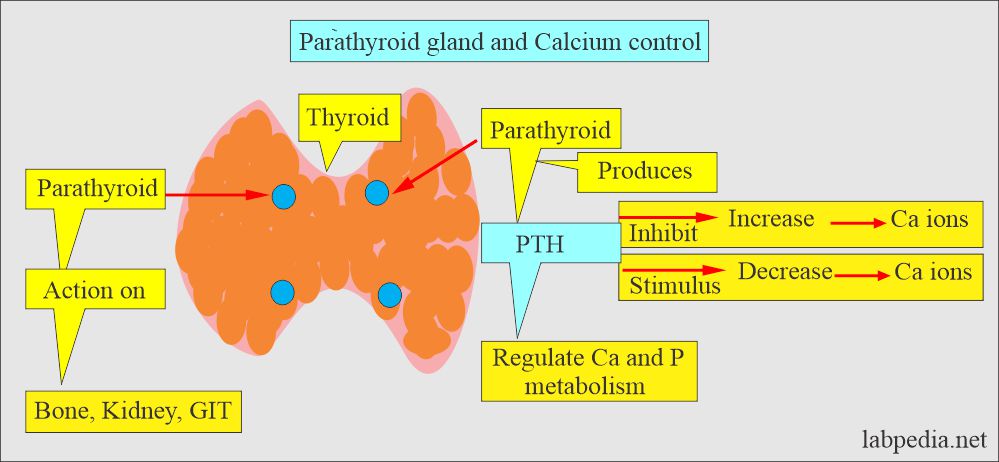
- PTH secretion is directly controlled by plasma calcium.
- This is the main hormone regulating calcium concentration in the extracellular fluid.
- A decrease in the ionized calcium is the stimulus for the PTH secretion.
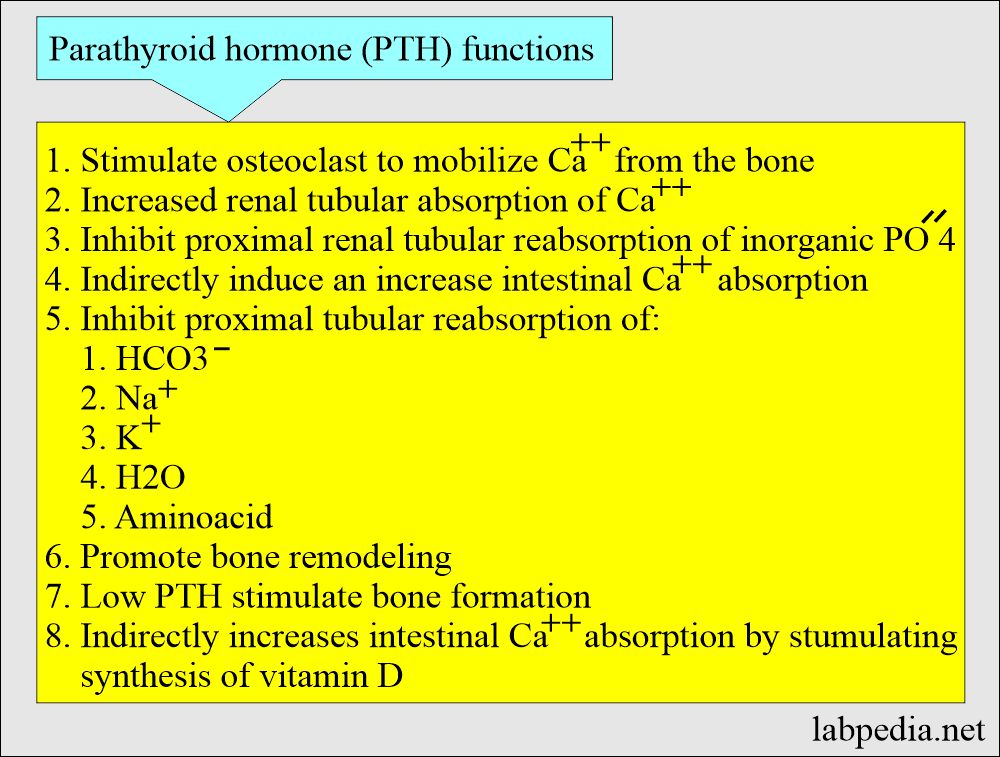
- PTH + 1,25- hydroxy D3 rais the calcium level by the following mechanisms:
- It promotes the dissolving of the bone.
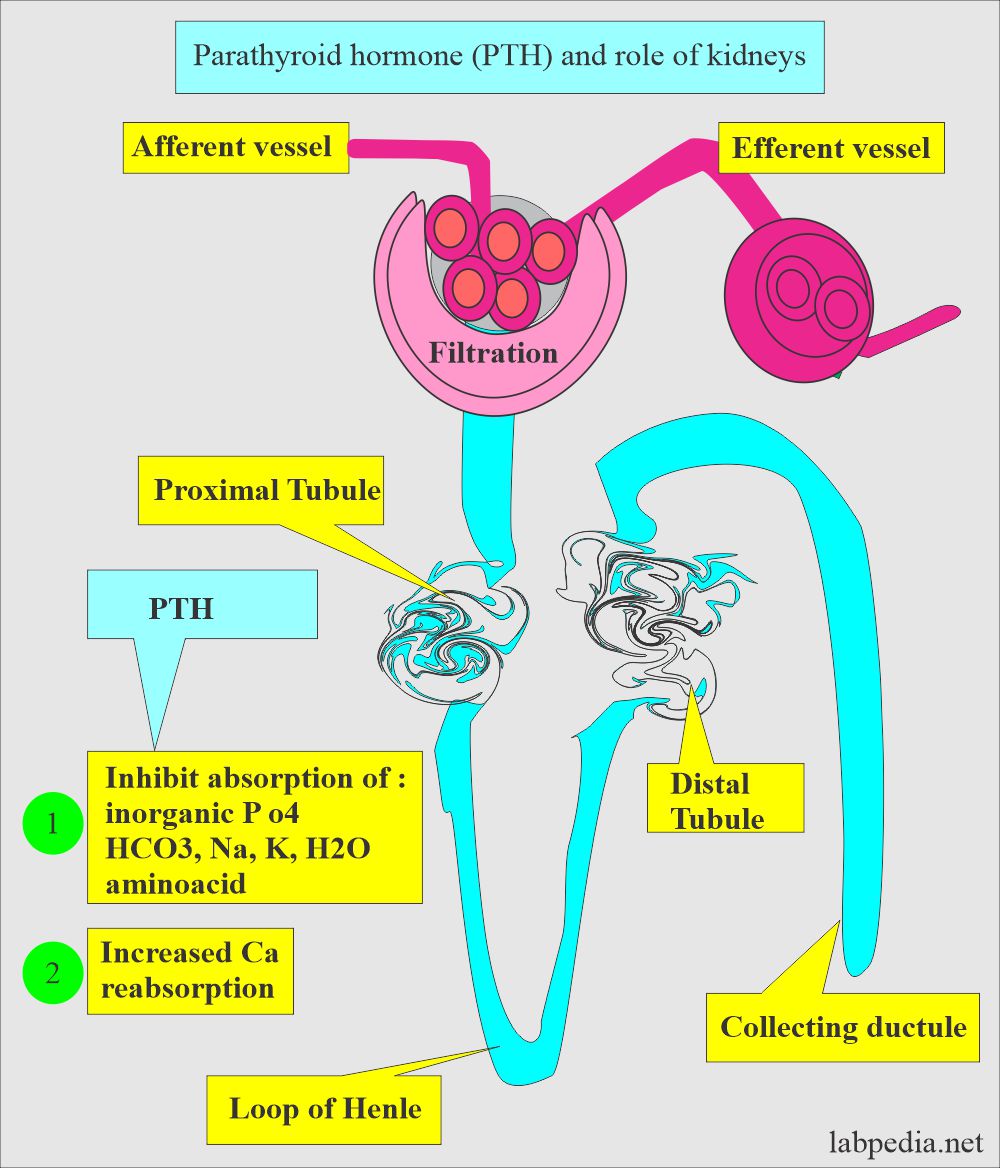
- Increases renal tubular reabsorption of calcium in the kidney.
- Increase intestinal absorption of calcium.
- A rise in Calcium inhibits PTH secretion.
- Magnesium also influences the PTH level.
- Hypermagnesemia suppresses the PTH secretion, although not like Calcium.
| Clinical condition | PTH | PTH |
| Ionized hypocalcemia | Stimulate | |
| Ionized hypercalcemia | Suppress | |
| Hyperphosphatemia | stimulate | |
| Hypermagnesemia | Suppress |
How will you classify hyperparathyroidism?
- Hyperparathyroidism is classified into:
- Primary hyperparathyroidism.
- Secondary hyperparathyroidism.
- Tertiary hyperparathyroidism.
How will you define Primary hyperparathyroidism?
- It is caused by parathyroid adenoma or rarely by cancer.
- The patient will have high PTH.
- And high Calcium levels.
- It may occur due to solitary adenoma.
How will you define Secondary hyperparathyroidism?
- It is due to chronic renal failure, where the patient has low calcium and high phosphate.
- Now, parathyroid glands persistently produce PTH to maintain Calcium levels.
- These patients have high PTH and low calcium.
How will you define Tertiary hyperparathyroidism?
- In this case, patients bypass the compensatory mechanism.
- Develops a high PTH level.
- This PTH leads to hypercalcemia.
- These patients have high PTH and High calcium levels.
- Intact PTH molecules metabolized into three different molecules:
- N-terminal.
- Mid-Region.
- C- terminal.
- Variation of the blood PTH level:
- The PTH level has diurnal variation. It is highest around 2 AM and lowest around 2 PM.
What are the normal levels of Parathyroid hormone (PTH)?
Source 1
- C- terminal and midmolecule
- Serm (by RIA)
- 1 to 16 years = 51 to 217 pg/mL
- Adult = 50 to 300 pg/mL
- N- Terminal
- Serum (by RIA)
- 2 to 13 years = 14 to 21 pg/mL
- Adult = 8 to 24 pg/mL
- Intact molecule
- Serum (by ICMA))
- Cord blood = ≤ 3 pg/mL
- 2 to 20 years = 9 to 52 pg/mL
- Adult = 10 to 65 pg/mL
Source 2
- Intact PTH molecule = 10 to 65 pg/mL (10 to 65 ng/mL)
- N-terminal intact PTH = 8 to 24 pg/L (8 to 24 ng/L)
- C-terminal intact PTH = 50 to 330 pg/L (50 to 330 ng/L)
- Mostly, the intact PTH molecule is recommended.
What are the causes of Increased Parathyroid hormone (PTH) levels?
- Primary hyperparathyroidism.
- Pseudohypoparathyroidism ( Secondary hyperparathyroidism ).
- Vit. D deficiency ( hereditary ) and rickets.
- Zollinger Ellison syndrome.
- Non-PTH-producing tumors give rise to paraneoplastic syndrome; They produce PTH-like protein that acts like PTH.
- Chronic renal failure.
- Hypocalcemia.
- Malabsorption.
What are the causes of decreased PTH levels?
- Grave’s disease ( Hypoparathyroidism ).
- Non-Parathyroid hypercalcemia.
- Surgical, secondary hypoparathyroidism.
- Sarcoidosis.
- Metastatic bone tumors.
- Vit.D intoxication.
- Milk-alkali syndrome.
- DiGeorge syndrome.
Questions and answers:
Question 1: What is the calcium level in primary hyperparathyroidism?
Question 2: When is the serum PTH level highest in the blood?


good informations
Thanks for the encouraging remarks