Neisseria Gonorrhoea, Urethral / Cervical smear For Gonorrhoea
Neisseria Gonorrhoea
What sample is needed for the diagnosis of Neisseria Gonorrhoea?
- The sample for the diagnosis of Gonorrhea is taken from:
- The urethra in the male.
- The endocervical area in the female.
- Oropharynx.
- Rectal swab.
How do I get the sample for Neisseria Gonorrhoea?
Urethral smears:
- It is a preferred site for men.
- Ask the patient to squeeze the penis and rub it on the slide to get a good smear.
- Delay is needed for obtaining specimens until 2 hrs after the patient has last voided.
- Obtain specimens on the slide for gram stain. (can take gonorrhea culture). Ask the Patient to squeeze the penis to get secretions. OR.
- Gently insert the urogenital swab into the urethra.
- Rotate the swab in one direction for at least one revolution for a minimum of 10 seconds.
- Withdraw the swab and smear it on the slide.
- Gently insert the urogenital swab into the urethra.
The endocervical specimen:
- The endocervical specimen is the preferred site in females.
- Specimen collection should be done with a sterile swab or culturette.
- Rotate the swab against the wall of the endocervical canal several times for 20 – 30 seconds and withdraw without touching the vaginal surface.
- Inoculate for culture.
- Cytobrush is not recommended as it may cause trauma and bleeding that can render the specimen unsatisfactory.
What is the Microbiology of Neisseria Gonorrhoea?
- Neisseria gonorrhea, also called gonococcus.
- It causes the second most common sexually transmitted disease.
- This is an obligatory parasite of the human urogenital system.
- The incubation period is 2 to 8 days.
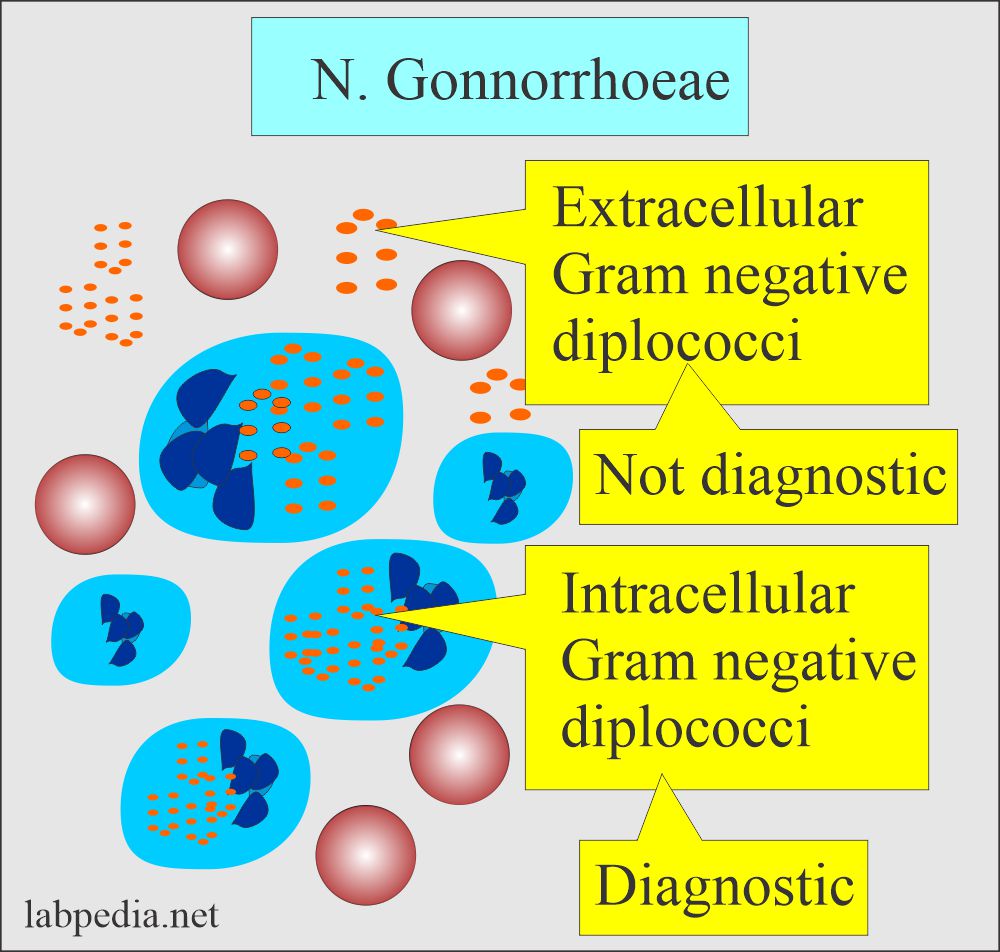
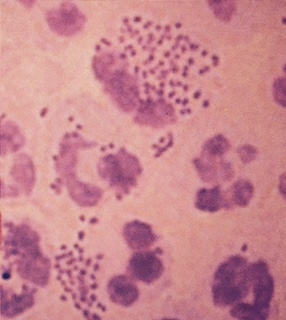
- These are gram-negative diplococci.
- These are oval cocci measuring 0.6 to 1.0 µm.
What are the culture characteristics of Neisseria Gonorrhoea?
- These occur in pairs with flattened adjacent sides or concave, bean-shaped.
- Culture media is an enriched medium like chocolate agar in the presence of CO² (5% to 10%).
- The best temperature for growth is 35 to 37 °C.
- Selective media can also be used by adding antibiotics that inhibit the growth of other bacteria but not the Neisseria, e.g., Thayer-Martin medium, which contains vancomycin, colistin, trimethoprim, and nystatin.
- There are small grey glistening colonies after 24 hours of incubation.
- These become larger, opaque, and somewhat irregular at 48 hours.
- These bacteria produce acid from glucose and no other sugars.
- These bacteria survive in the pus but can’t outside the body and die soon.
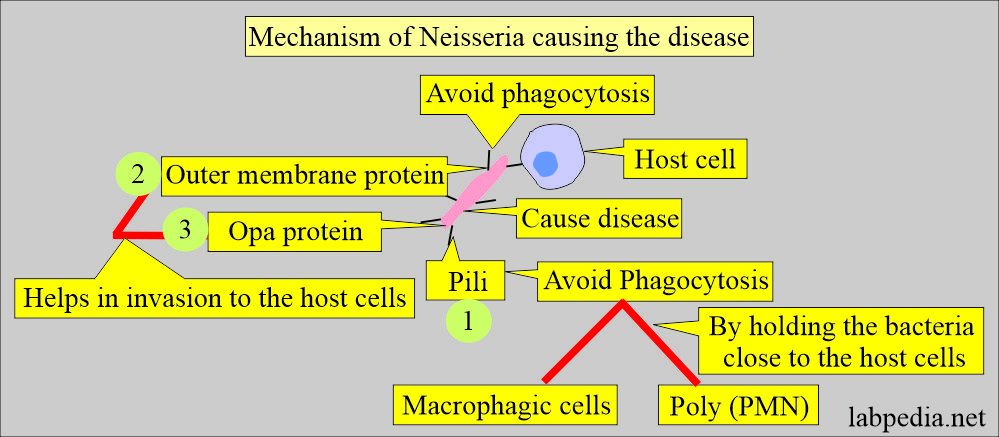
What are the virulence factors of gonorrhea?
- Pili over the surface of the bacteria. It will attach to the host cells and give rise to disease.
- It holds close to host cells and avoids phagocytosis by the macrophagic cells and poly (PMN).
- Membrane proteins cause penetration into the host cells.
- Opa protein is also another outer membrane protein. It causes adherence and penetration into the host cells.
Is Neisseria Gonorrhoea a sexually transmitted disease (STD)?
- In the USA, there are an estimated 820,000 new patients with gonorrhea occur every year.
- This is the second most common sexually transmitted disease. (CDC).
- N. gonorrhea infects the mucous membranes of the reproductive tract, including the cervix, uterus, and fallopian tubes in women and the urethra in women and men.
- These bacteria have fast growth in these mucous membranes.
- N. gonorrhea can also infect the mouth, throat, eyes, and anus mucous membranes.
What is the Mode of the spread of Neisseria Gonorrhoea?
- Gonorrhea bacteria can survive in the infected warm and moist areas like the urethra, cervix, and rectum.
- The spread is by:
- Sex when done without any protection, oral or anal.
- People with multiple sexual partners.
- Using contaminated sex vibrators or devices.
- Some of the sex partners have more risk of getting this infection.
- The patient may develop anal pain and discharge.
- Most common in the age group of 15 to 29 years.
What are the Signs and Symptoms of Neisseria Gonorrhoea?
In the female:
- There are mild symptoms of vaginal infection.
- Symptoms appear after 2 to 5 days in males, while in females, these bacteria may be present for over 30 days.
- There are painful urination and blood in the urine.
- There is a yellow vaginal discharge.
- If females are not treated, then it may lead to pelvic inflammatory disease.
- There may be conjunctivitis.
- Infected ladies may feel pain and bleeding after the coitus.
- On examination, there may be a swollen vulva.
In the Males:
- It may have painful and swollen testicles due to epididymitis.
- There is a yellowish or greenish discharge from the penis.
- There may be conjunctivitis.
- There are swollen and painful tests.
- The patient may develop anal pain and discharge.
What are the complications of Neisseria Gonorrhoea?
- Untreated gonorrhea can cause serious and permanent health problems in both women and men.
- There may be the possibility of septic arthritis.
- There may be gonococcal bacteremia.
In women, complications are:
- Gonorrhea can spread into the uterus or fallopian tubes and cause pelvic inflammatory disease (PID).
- PID can lead to internal abscesses and chronic pelvic pain.
- PID can also damage the fallopian tubes enough to cause infertility or increase the risk of ectopic pregnancy.
- Complications in females are:
- Urethritis.
- Cervicitis.
- Dyspareunia.
- Purulent vaginal discharge.
- Pelvic inflammatory disease (PID).
- Infertility.
- Ectopic pregnancy.
- Abscess.
- Peritonitis.
- Peri-hepatitis.
- Endometritis.
- Salpingitis.
- Oophoritis.
In men, complications are:
- Gonorrhea may be complicated by epididymitis.
- In rare cases, this may lead to infertility.
- Complications in males are:
- Urethritis.
- Epididymitis.
- Prostatitis.
- Urethral stricture.
- Rectal gonococcal infection.
- Untreated, gonorrhea can also spread to the blood and cause:
- Disseminated gonococcal infection (DGI).
- DGI is usually characterized by the following:
- Arthritis, tenosynovitis, and/or dermatitis.
- This condition can be life-threatening.
In pregnancy, complications are:
- A woman with gonorrhea can give the infection to her baby while passing through the birth canal during delivery.
- The baby may develop:
- Blindness.
- Joint infection.
- Or a life-threatening blood infection in the baby.
Complications of Pelvic inflammatory disease (PID):
- Infertility. The risk of infertility increases with each attack of gonorrhea.
- Ectopic pregnancy. It increases due to previous inflammation of the fallopian tubes.
- Abscess formation in fallopian tubes, ovaries, and peritoneum.
- Peritonitis, where bacteria spread from the ovaries and fallopian tubes.
- Peri-hepatitis may be seen in gonorrhea infection.
Complications in infants:
- Gonococcal infection can spread from the mother to the newborn and gives rise to ophthalmia neonatorum.
How will you diagnose Neisseria Gonorrhoea?
- A swab or urethral smear is quick and accurate if the sample is adequate.
- Culture the material obtained by swab or brush from the endocervical area in females and urethral swabs in males.
- CDC recommends that NAAT (nucleic acid amplification test) is a rapid test.
- For NAAT, the specimen can be taken from endocervical, vaginal, and urethral swabs.
- Also, NAAT can use urine from both men and women.
What will be the result of Gram stain for Neisseria Gonorrhoea?
- Stain the smears with gram stain.
- There are intracytoplasmic gram-negative cocci.
- These are seen as diplococci.
How will you Prevent Neisseria Gonorrhoea?
- This needs the education of young couples.
- Mechanical means like condoms can be used.
- Chemical prophylaxis is also effective.
- If there is exposure to gonorrhea patients, antibiotics within 24 hours are effective.
How will you treat Neisseria Gonorrhoea?
- This is a treatable disease.
- These are sensitive to penicillin, tetracycline, macrolides, ciprofloxacin, and cefuroxime.
- Most people (CDC) recommend dual antibiotic therapy.
- A single dose of Ceftriaxone 250 mg I/M.
- Azithromycin 1 gram oral dose.
- There are reports of resistant N. gonorrhea.
Questions and answers:
Question 1: What is the criteria of the diagnosis of N. Gonorrhea?
Question 2: What are the complications of Gonorrhea?