Maternal screening:- Part 2 – Prenatal Screening For Genetic Abnormalities (Chromosomal)
Maternal screening
What sample is needed for Maternal screening?
- The patient’s serum is taken during the second trimester.
- Ideally, around the 18th week is the best time.
What is the significance of Maternal screening?
- This is done for pregnant ladies to prepare them mentally for abnormal babies.
What are the indications for Maternal screening?
- Prenatal screening is done to diagnose:
- Neural tube defect
- Trisomy 18
- Down’s syndrome
- This test is advised for the ladies who:
- Has a family history of birth defects.
- Ladies 35 years or older age group.
- If there is a history of drugs used during pregnancy, which may be harmful to the fetus.
- Diabetic ladies using insulin.
- If there is a history of viral infection during pregnancy.
- If the lady is exposed to radiation, even on routine X-rays.
- This test may be advised in case of multiple pregnancies.
What are the possible Genetic abnormalities?
- Many chromosomal abnormalities are:
- Autosomal does not involve the sex chromosomes.
- Sex-linked abnormalities are called inherited through sex chromosomes.
- There may be total or partial deletion of the chromosome.
- Presence of the extra chromosome attached to the pair of chromosomes (trisomy).
- There may be translocation, where part of a chromosome is broken and attached to another chromosome.
- Other genetic abnormalities include a deficiency in enzymes or abnormalities.
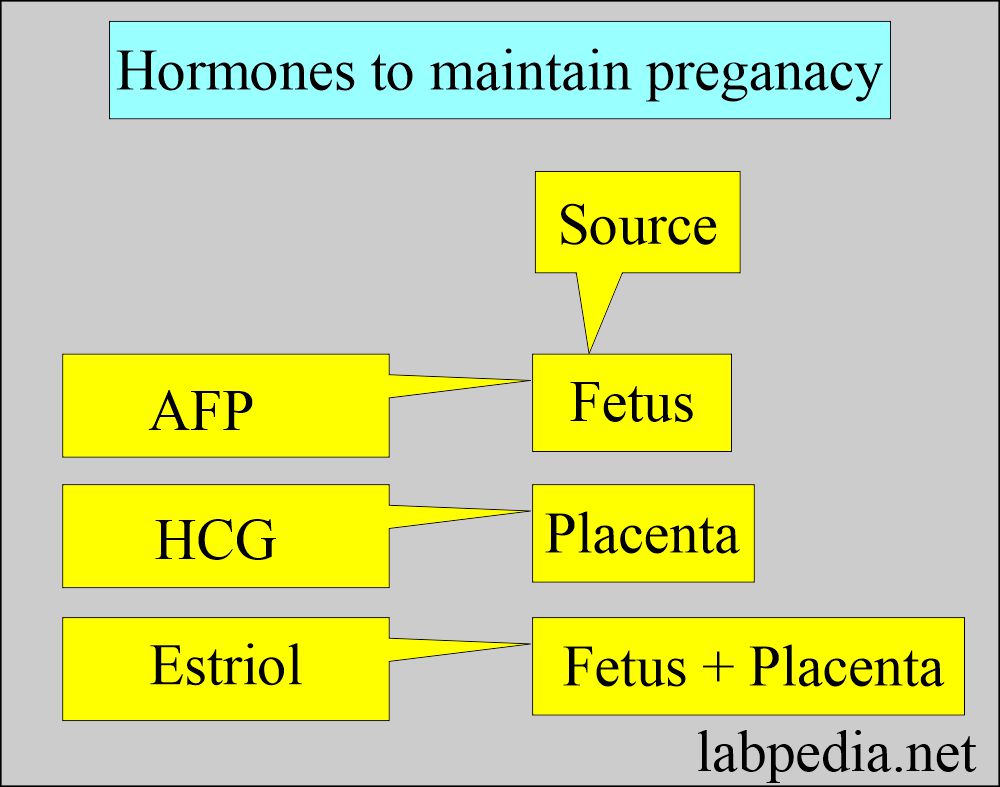
- Triple screening measures the level of AFP, HCG, and estriol.
- This is a screening test and not confirmatory for fetal abnormalities.
- There may be a false positive test.
- This can be supported by ultrasound.
- Amniocentesis was advised in positive cases for more accuracy.
Neural tube defect
How will you define Neural tube defect?
- Neural tube defect is due to failure of fusion of the neural tube.
- Neural tube defects may show as follows:
- Anencephaly
- Encephalocele
- Spina bifida (open)
- Meningomyelocele
- Anencephaly is a serious condition; most babies die within a few hours of birth.
- The incidence of neural tube defects is one per 1300 pregnancies.
- Another source says 1 in 500 live births.
How will you diagnose a Neural tube defect?
-
- Normal HCG.
- Increased AFP
- Decreased UE.
- Maternal AFP is raised.
- An ultrasound of the abdomen may help diagnose the neural tube defect. It will confirm the single pregnancy.
- Ultrasound establishes normal pregnancy, fetal viability, and identifiable congenital defects.
- Amniotic fluid level of AFP:
- AFP > 2.5 MoM (multiple of the median) will be found in 90% of cases of anencephaly.
- AFP >2.5 MoM diagnoses in 80% of the cases of spinal bifida.
- Electrophoresis of amniotic fluid shows two bands of nonspecific cholinesterase and acetylcholinesterase (ACHE).
Trisomy 18
How will you define Trisomy 18?
- There is a third copy of chromosome 18 in most of the cells.
- An extra chromosome is attached to a pair of chromosome 18 (trisomy).
- This is a chromosomal abnormality showing aneuploidy.
- Clinical presentation of trisomy 18:
- Congenital heart disease.
- Renal abnormality.
- Intellectual abnormality.
- The ears are low-set.
- Fists are clenched.
- The incidence is 1 per 4100 pregnancies.
- The incidence of trisomy 18 abnormality increases with the age of the mother.
- Baby with trisomy 18 abnormality, 60% die in the first month of life.
- While 90% die within the first year of life.
- Trisomy 18 usually shows a characteristic pattern that there is:
- Decreased HCG.
- Decreased AFP
- Decreased UE
- About 80 % of Trisomy 18 cases were detected by the above screening.
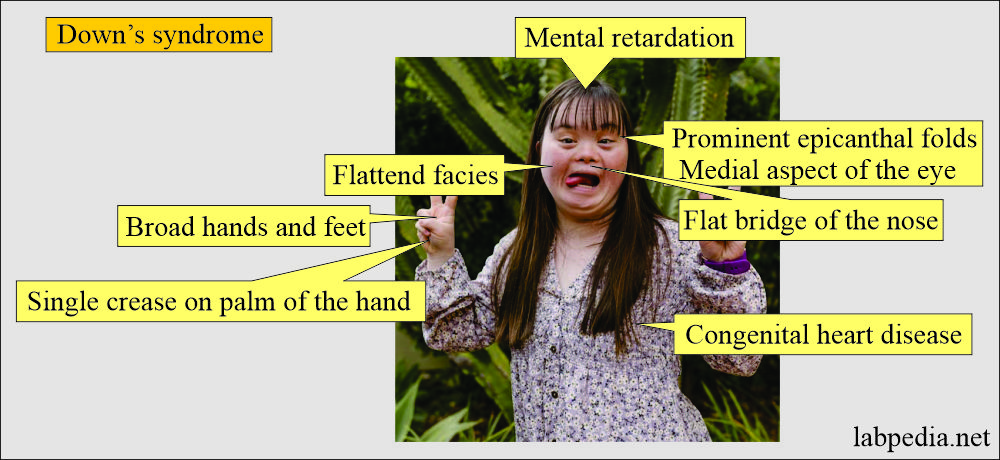
Down’s syndrome
How will you define Down’s syndrome?
- Women >35 years of age need genetic analysis Of amniotic fluid.
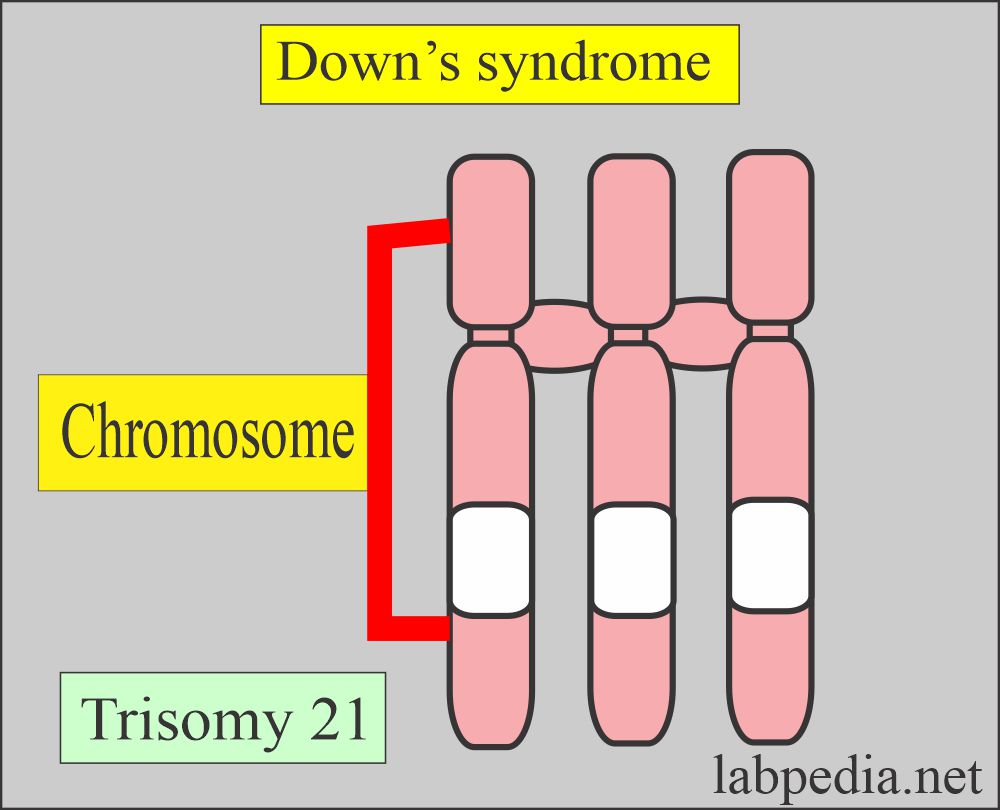
- Genetic picture:
- This syndrome is characterized by trisomy 21 and is common autosomal aneuploidy.
- Clinical presentation of Down’s syndrome:
- Down’s syndrome baby shows:
- Retarded growth.
- There is a lack of muscle tone.
- There is an intellectual abnormality.
- The incidence increases with the mother’s age.
- The incidence is 1 per 750 live births of the baby.
How will you diagnose Down’s syndrome?
- The triple screen:
- This test consists of the estimation of the following:
- Human chorionic gonadotropin (HCG).
- Alpha-fetoprotein (AFP)
- Unconjugated estriol (UE)
- The sensitivity of this panel to Down’s syndrome is 70 %.
- Quad screening:
- This test consists of the following:
- Human chorionic gonadotrophin (HCG).
- Alpha-fetoprotein (AFP).
- Unconjugated Estriol (UE).
- Dimeric inhibin A
- The accuracy of the quad test for Down’s syndrome is 80%.
- The combined serum test and ultrasonographic measurement of nuchal fold thickness led to a more than 90% sensitivity.
- Amniotic fluid analysis is the gold standard for ladies above the age of 35 years.
- Down’s syndrome shows the following pattern:
- Increased HCG
- Decreased AFP.
- Decreased UE.
- Ultrasound will be helpful in evaluating the gestational age, excluding the multiple gestations, and can find anatomical abnormalities.
- Amniotic fluid may be obtained by amniocentesis to estimate AFP and acetylcholinesterase.
Differential diagnosis of genetic abnormalities:
| Abnormality | HCG | AFP | UE | Dimeric Inhibin A |
| Down’s syndrome | increased | decreased | decreased | increased |
| Neural tube defect | normal | increased | decreased | |
| Trisomy 18 | decreased | decreased | decreased | |
| Diabetic mother | decreased | decreased | ||
| Smoker mother | decreased | increased | decreased |
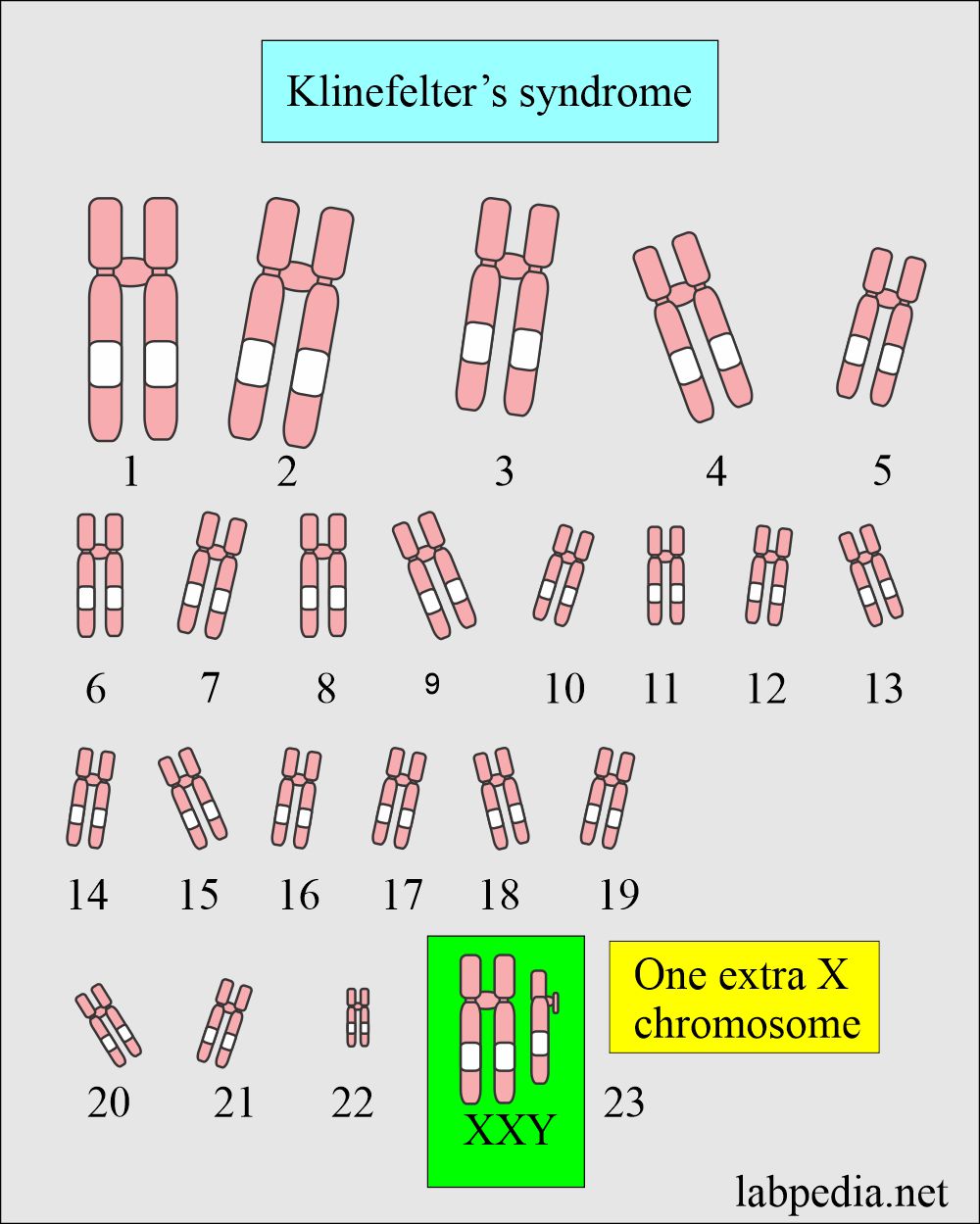
Klinefelter’s syndrome
What is the genetic picture of the Klinefelter’s syndrome?
Genetic picture of Klinefelter’s syndrome:
- The patient looks male, but the sex chromosome is XXY instead of XY.
What is the presentation of Klinefelter’s syndrome patient?
- The external genitalia is usually normal except for small testes.
- A tendency for androgen hormone deficiency will lead to gynecomastia and decreased body hair.
- In some patients, the above findings are mild or absent.
- There is a tendency for mental retardation, but patients with normal mental status may be seen.
- These patients are always sterile.
How will you diagnose Klinefelter syndrome?
- Testicular biopsy is diagnostic, showing marked atrophy of the seminiferous tubules.
- The buccal smear shows one barr body due to XX chromosome.
- 10% of the cases have mosaic cell patterns.
- Chromosome karyotyping is the procedure of choice.
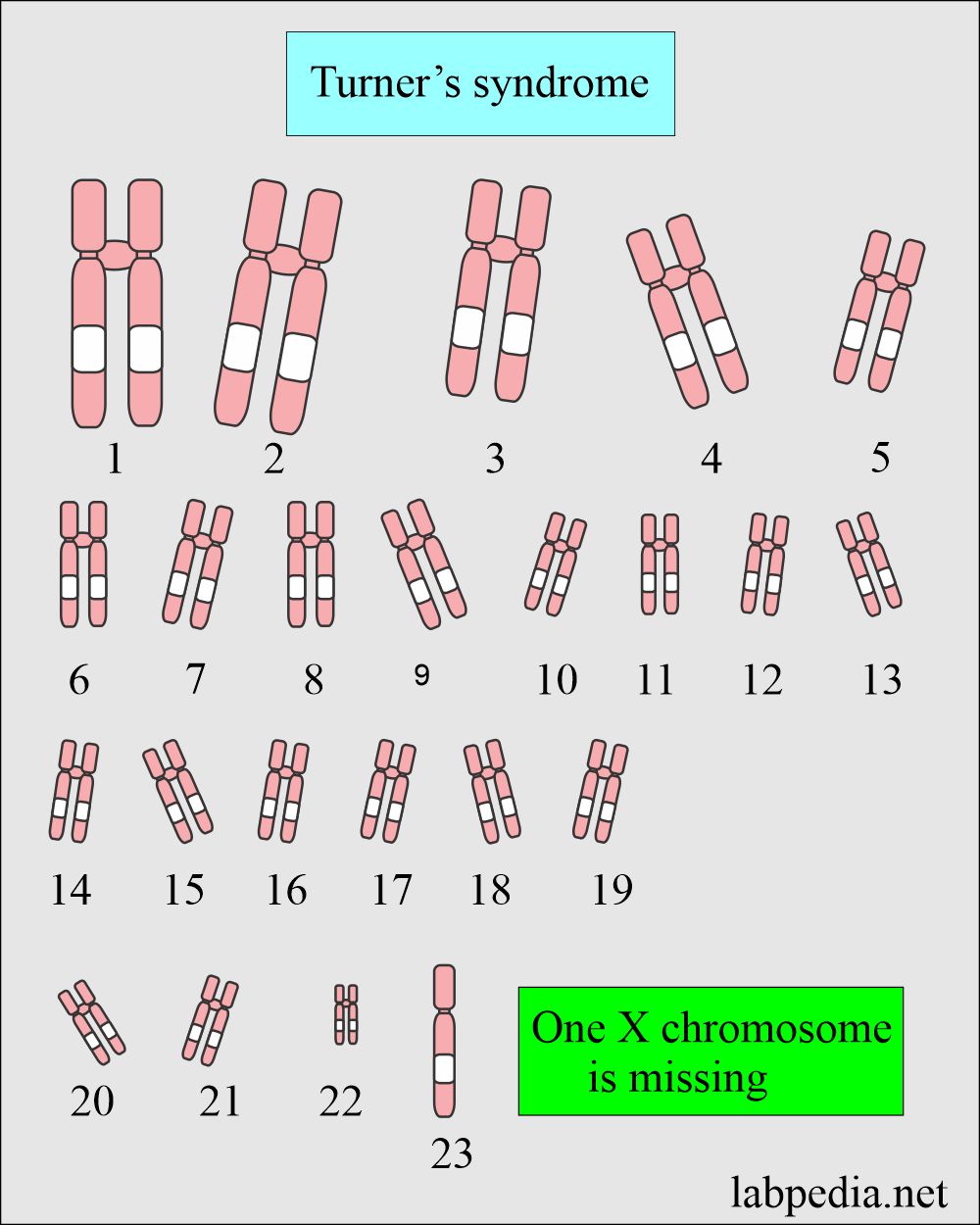
Turner’s syndrome
How will you define Turner’s syndrome?
- This is also called ovarian agenesis.
- This is the most common abnormality of genetics in females.
What is the Genetic picture of Turner’s syndrome?
- One X female chromosome is deleted, so the patient has only 45 chromosomes. There is only one X chromosome instead of two XX chromosomes.
How will Turner’s syndrome be presented?
- Typically affected females have short stature but normal body proportions.
- Secondary-sex characters are not developed, and there are small genitalia.
- Body hairs usually have a normal distribution.
- Some patients may have a webbed neck, coarctation of the aorta, and short fingers.
- These ladies usually do not menstruate because of the lack of ovaries.
How will you diagnose Turner’s syndrome?
- Buccal smears are negative.
- In the case of positive cases, do chromosomal karyotyping.
- The reason is that some cells are positive, and some cells are negative (mosaic pattern).
What are the conditions associated with increased maternal AFP?
- Neural tube defect.
- Twins.
- Fetal death.
- Feto-maternal hemorrhage.
- Omphalocele.
- Sacrococcygeal Teratoma.
- Cystic teratoma.
- Cystic hygroma.
- Intestinal obstruction.
- Renal anomalies.
- Turner syndrome.
Questions and answers:
Question 1: How many chromosomes in Klinefelter's syndrome?
Question 2: What is a picture of karyotyping in Turner's syndrome?