Malarial parasite:- Part 4 – Plasmodium Malariae, Benign Quartan Malaria
Plasmodium Malariae
What sample is needed for Plasmodium Malariae?
- Malarial parasites ( MP ) may be diagnosed with a fever from a patient’s blood smear.
- The best time to make a smear is during shivering.
- Make thick and thin blood smears.
- A serum is needed for a serological method and PCR.
How will you define Plasmodium malaria?
- Plasmodium malariae causes fever every 72 hours.
- Primarily, it infects older small RBCs.
What are the important facts about Plasmodium Malariae?
- The Greeks recognized this because of its fever presentation.
- This is a cosmopolitan parasite but not seen everywhere.
- 2% to 3% in Africa.
- Sporadic cases are seen in Asia and S. America.
- It is common in regions of tropical Africa.
- Also seen in India, Sri Lanka, Malaya, Java, New Guinea, and Europe.
- Plasmodium malariae represents only a small percentage of infections.
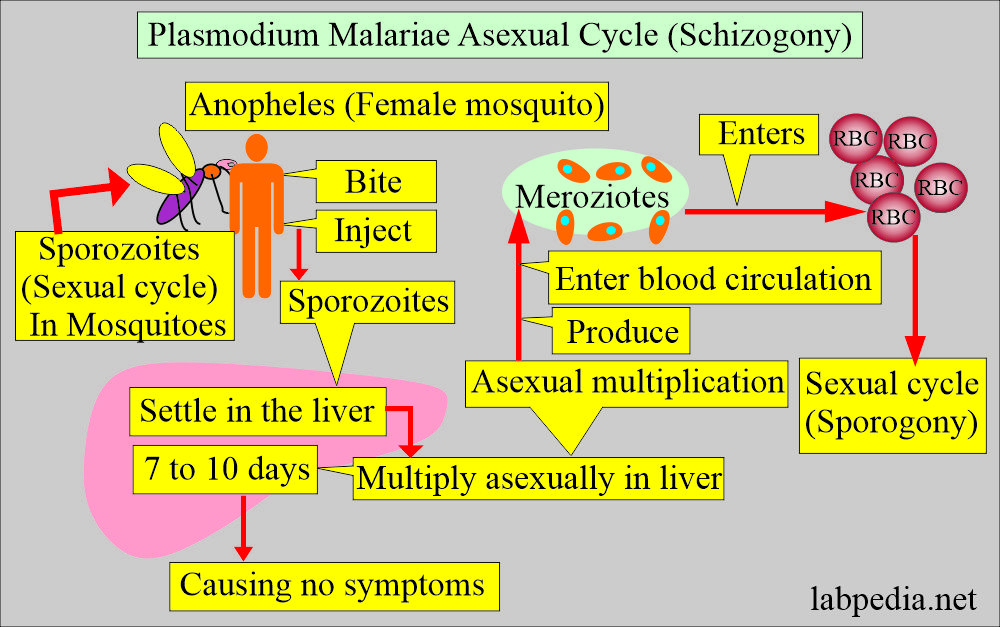
What is the vector of Plasmodium malaria?
- These are seen in wild animals. Chimpanzees are also infected.
- It spreads through female mosquito bites.
- Various groups of Anopheles exist, and around 30 to 40 serve as a vector for Plasmodium malariae.
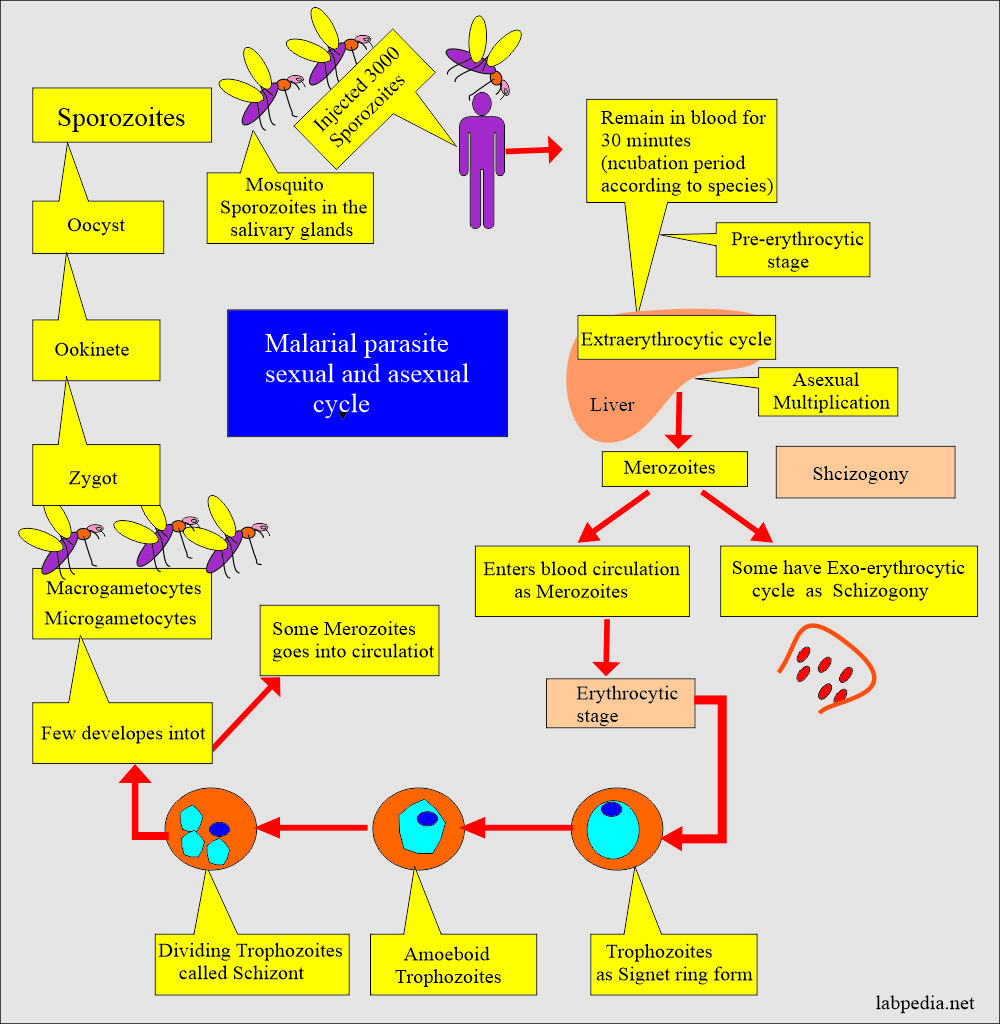
What is the exoerythrocytic cycle of Plasmodium Malariae?
- It is completed in the liver in 13 to 16 days.
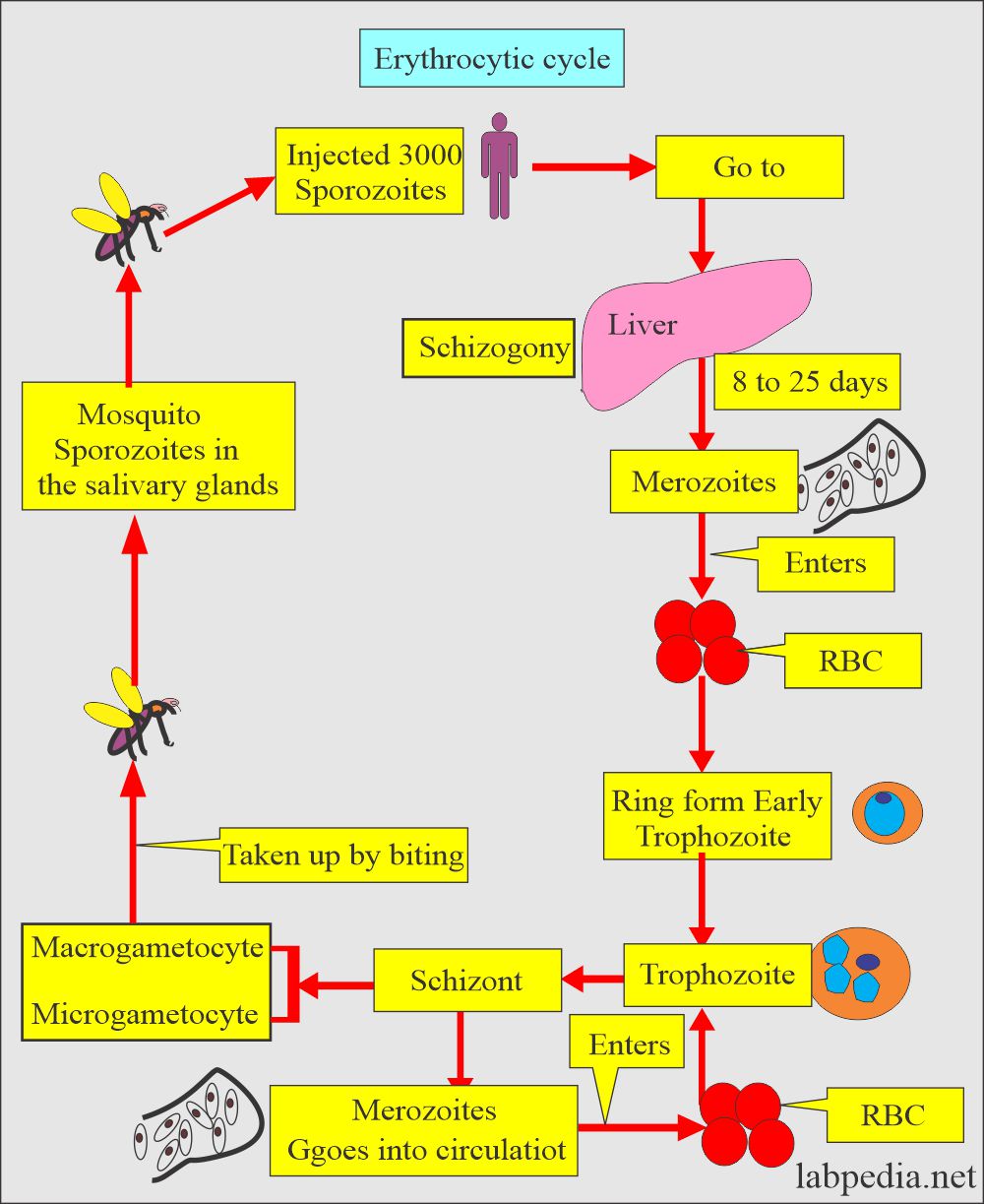
What is the erythrocytic cycle of Plasmodium Malariae?
- Ring form typically occupies 1/6 of the infected RBC.
- It is smaller than P. vivax.
- There is a heavy chromatin dot.
- Pigments form early.
- Trophozoites are typically non-ameboid, with solid cytoplasm.
- The cytoplasm shows dark brown pigments that may mask the chromatin.
- Schizonts typically contain 6 to 12 merozoites.
- These are arranged in rosettes or irregular clusters.
- Central brown-green pigment may often be visible.
- Parasite completely fills the RBC.
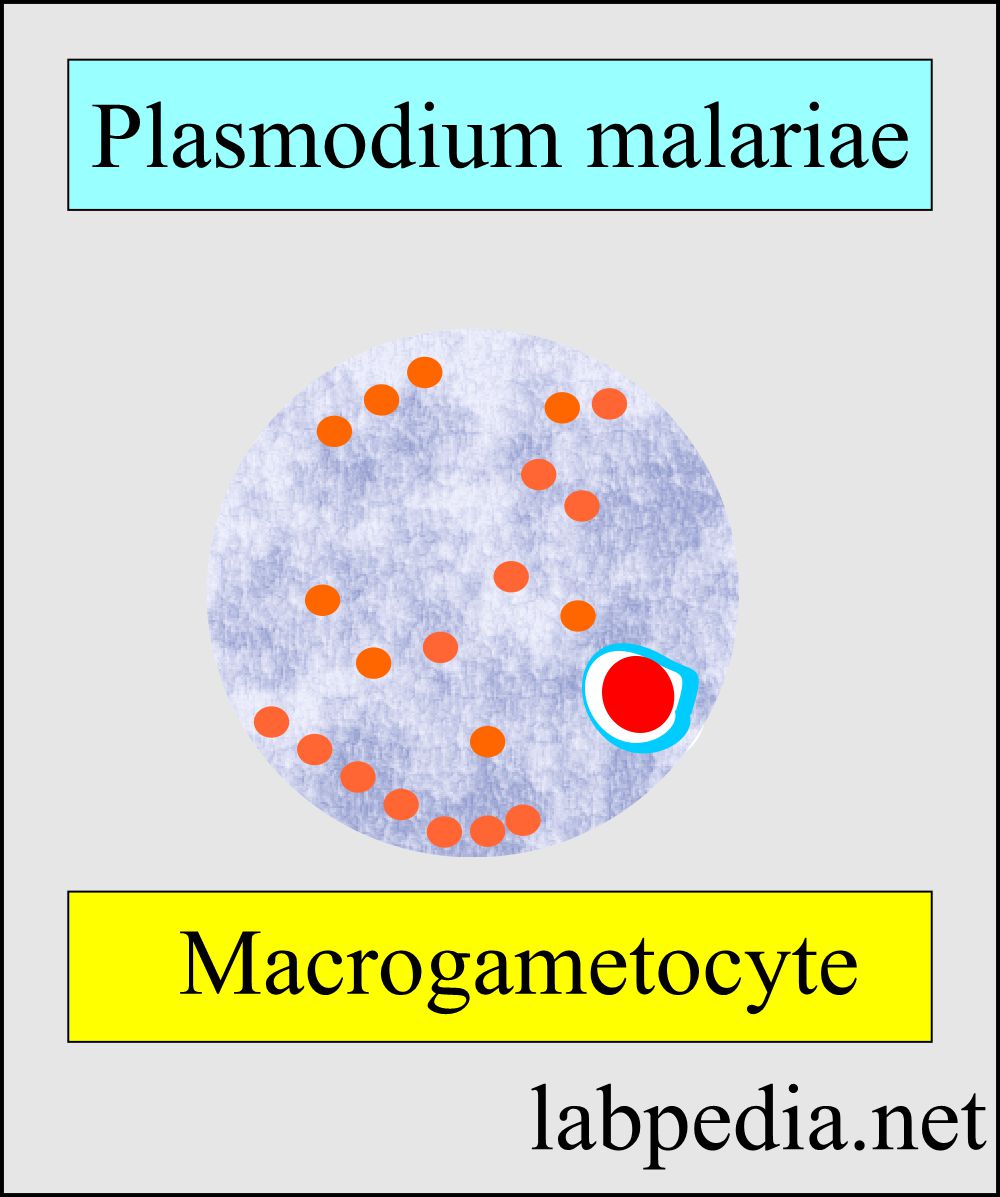
- Microgametes are similar to P. vivax except for one notable darker pigment, which is coarse.
- Macrogametocytes also have darker pigments and are more coarse.
- No Schuffner’s dots are seen.
What are the clinical presentations of Plasmodium Malariae?
- There is an incubation period of 18 to 40 days.
- There are flu-like symptoms.
- Cyclical paroxysms occur every 72 hours.
- There may be spontaneous recovery.
- No relapse is reported.
How will you diagnose Plasmodium Malariae?
- History of the patient in suspected areas.
- Blood smear:
- Make a blood smear when the patient has a fever. Thin and Thick smears are made.
- The thick smear is more helpful in finding M. Parasites.
- The thin smear is suitable for identifying the type of malarial parasite.
- Collect blood 6 to 8 hourly till 48 hours to declare negative for malaria.
- Giemsa stain is the best choice.
- Serologic methods are based on immunochromatic techniques. Tests often use a dipstick or cassette format and provide results in 2-15 minutes.
- Polymerase chain reaction (PCR): The PCR technique detects parasite nucleic acids. It is more sensitive than smear microscopy, but it is of limited value for diagnosing acutely ill patients because of the time needed for this procedure.
How will you control Mosquitoes?
- Try to eliminate breeding places:
- Fill the vacant land and pump out the water.
- Remove the junk and water-retaining debris.
- Destroy the larvae:
- Clean the drains.
- Try to remove algae from the ponds.
- Add larva-eating fish to the ponds.
- Use of the insecticide:
- The best example is DDT.
- Use of mosquito repellent:
- Pyrethroid repellent.
- N, N- diethyl meta tolbutamide.
- Use of mosquito nets.
- Use clothes to prevent mosquito bites.
- Train people for malaria prevalence.
- Train the people for the detection of malaria, treatment, and follow-up.
How will you treat plasmodium malariae?
- Antimalarial drugs used are quinidine, chloroquine, primaquine, pyrimethamine, sulfadoxine, mefloquine, tetracyclines, and proguanil.
- Chloroquine is the drug of choice and is best for P. falciparum.
- This is effective for the erythrocytic stage and not for the liver stage.
- Must use primaquine to eradicate P. ovale and P. vivax.
- there are chloroquine resistant cases of P. falciparum.
- Amodiaquin, piperaquin and pyronaridine are close to chloroquin.
- In some areas, Amodiaquine is less toxic, cheap, and effective against chloroquine-resistant P. falciparum.
- Mefloquine is effective against choloquin resistant P. falciparum.
- Quinine and quinidine are still the first lines of therapy against P. falciparum.
- Primaquine is a synthetic drug and is the drug of choice for eradicating liver-stage from P. vivax and P. ovale.
- Antibiotics and Inhibitors of folate synthesis are slow-acting antimalarial drugs.
- Halofantrine and lumefantrine are related to quinine and are effective against the erythrocytic stage.
- Malaria drug-resistant strains are emerging.
Duration of the various cycles in malarial parasites:
| Type of malarial parasite | Sexual cycle in the mosquito | Length of asexual cycle | Length of the sexual cycle |
| Plasmodium falciparumm | 9 to 10 days | 5 to 7 days | 36 to 48 hours |
| Plasmodium vivax | 8 to 9 days | 8 days | 48 hours |
| Plasmodium ovale | 14 days | 9 days | 48 hours |
| Plasmodium malariae | 15 to 20 days | 15 to 16 days | 72 hours |
Questions and answers:
Question 1: How many days are needed for the exoerythrocytic cycle?
Question 2: How many merozoites are seen in the schizonts of plasmodium malariae?