Malarial parasite:- Part 2: – Plasmodium Falciparum, MP Falciparum, Black Water Fever
Plasmodium Falciparum
What sample is needed for the diagnosis of Plasmodium Falciparum?
- Malarial parasites (MP) may be diagnosed with a fever from a patient’s blood smear.
- The best time to make a smear is during shivering.
- Make thick and thin blood smears.
- A serum is needed for a serological method and PCR.
How will you define Plasmodium falciparum?
- This is the most common type in the tropics.
- It causes a fever after every 48 hours. This is the most fatal type of malaria and leads to blackwater fever.
- It can infect all stages of maturation of RBCs.
What are the important facts about Plasmodium Falciparum?
- Plasmodium falciparum is most common (≈45%) in the tropics and the United States.
- Epidemiology of the Plasmodium falciparum:
- 90% of cases occur in Africa,
- 40% to 50% of cases in western Pacific and SE Asia,
- 4% to 30% in S. Asia, S. America, and the rest of the topics.
- P. Falciparum is responsible for the majority of malaria deaths globally.
- This is the most prevalent species in sub-Saharan Africa.
- This can infect RBCs of any age.
- Young RBCs are more vulnerable.
- RBCs are not usually enlarged or distorted, as seen in P. vivax and P. ovale.
- As all ages of RBCs are involved, there is a large amount of toxic cellular material and plugging of the capillaries.
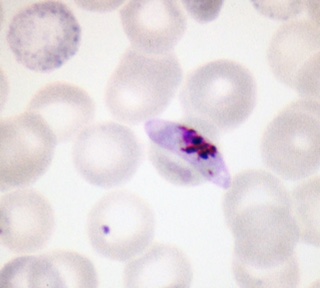
- Only ring form and gametes are seen in the smears.
- Only the ring form and the gametocytes are seen in the peripheral blood.
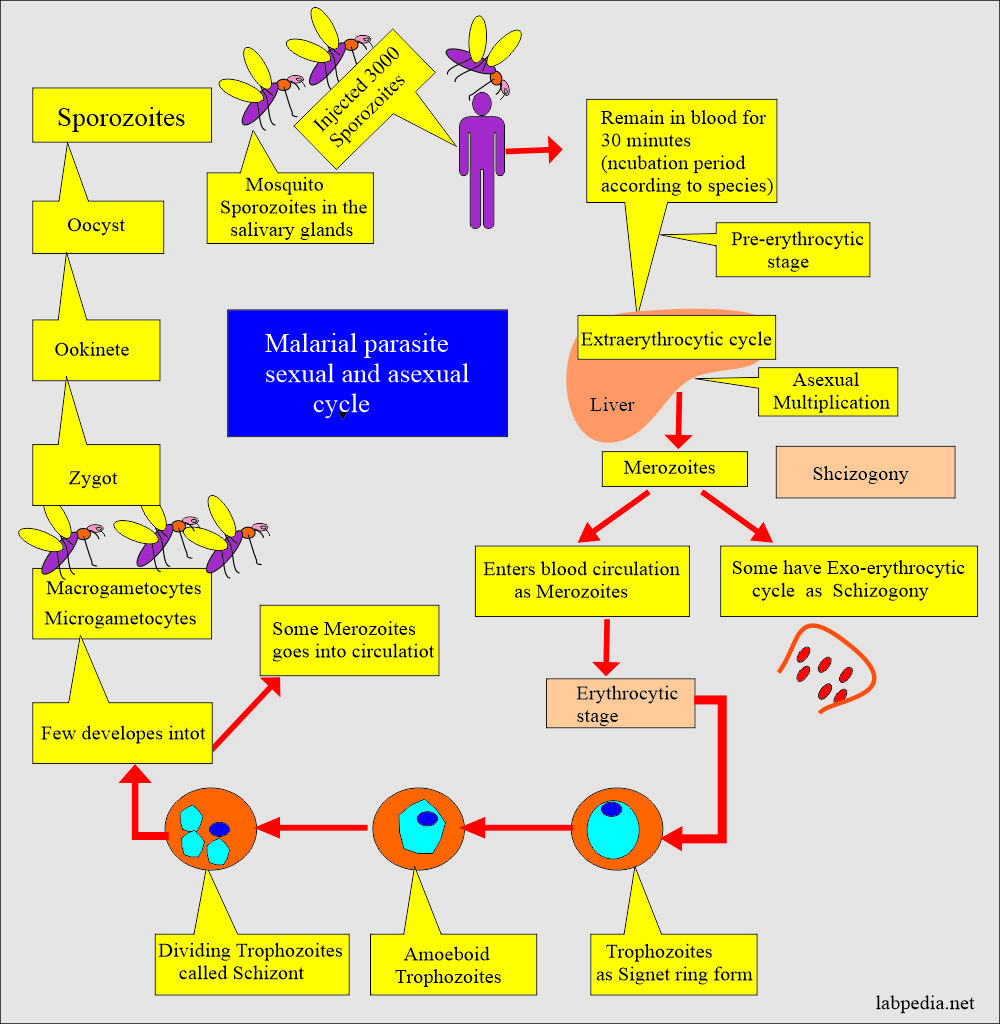
What is the exoerythrocytic cycle of Plasmodium Falciparum?
- P. falciparum schizont grows in the liver cells.
- It is more irregular in shape than the P. vivax, with projections extending in all directions by the fifth day.
- After rupture, it releases about 30,000 merozoites.
- There may be remission of up to one year.
- These merozoites can infect RBCs of any age, even reticulocytes, causing a very high level of parasitemia.
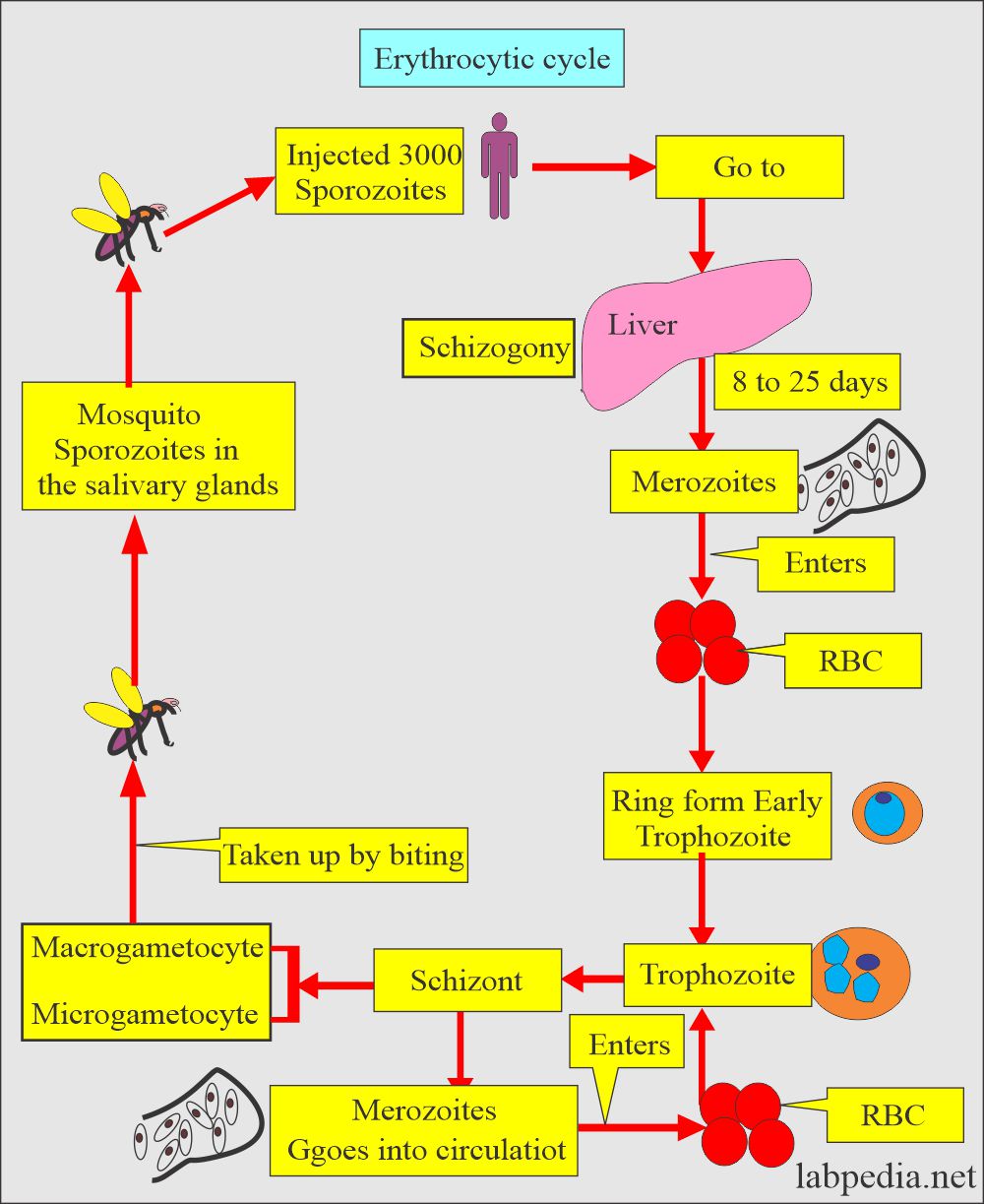
What is the erythrocytic cycle of Plasmodium Falciparum?
- Merozoites enter all aged RBCs and reticulocytes.
- There is the sequestration of the RBCs in the capillaries of the brain, spleen, and bone marrow.
- The early ring form trophozoite is the smallest of any Plasmodium type.
- Schizonts are less symmetrical than any of the other forms.
- It forms 8 to 32 merozoites and is usually 16 in number.
- The erythrocytic cycle takes 48 hours.
- There is a high level of parasitemia, with more than 65% of the RBCs containing parasites.
- The 25% involvement of RBCs is fatal.
- Only young trophozoites, such as ring form and gametocytes, are seen in the peripheral blood.
How will you discuss the clinical presentation of Plasmodium Falciparum?
- There may be early flu-like symptoms.
- This is the most fatal and threatening type of other types.
- The incubation period is short, 7 to 10 days.
- There are episodes of chills and fever.
- There will be nausea and vomiting.
- There will be diarrhea.
- There are muscle aches and pain.
- These symptoms are cyclical for 36 to 48 hours.
What is Blackwater fever or malignant tertian malaria?
What is the mechanism of injury to the RBCs?
- Acute intravascular hemolysis causes hemoglobinuria (Blackwater fever).
- When this parasite enters the kidney, brain, and liver.
- Infected RBCs develop a sticky-knobby appearance leading to the sludging of the RBCs and causing infarction of the brain, kidneys, and other organs.
What are the signs and symptoms of Blackwater fever?
- Cerebral malaria is only caused by Plasmodium falciparum. These patients will have cerebral signs and symptoms and may go into a coma.
- There is marked hemoglobinuria.
- Plasmodium Falciparum, when severe, gives rise to:
- Coma.
- Breathing difficulties.
- Low blood sugar.
- Low hemoglobin leads to anemia.
- Children are more prone to develop cerebral malaria.
- Untreated, severe malaria can lead to death.
How will you diagnose Blackwater fever?:
- For the diagnosis, a smear will show banana-shaped parasites.
How will you protect from Plasmodium falciparum (Blackwater fever)?
- Sickle cell anemia and Thalassemia give protection from the plasmodium falciparum.
- These RBCs rupture before the merozoites mature inside these RBCs.
What are the complications of Plasmodium Falciparum?
- There may be acute renal failure.
- Other possibilities are tubular necrosis and nephrotic syndrome.
- The brain is involved with plug formation in the capillaries and causes cerebral malaria.
- The patient goes into a coma, followed by death.
- There may be pulmonary edema.
- There is severe anemia.
How will you diagnose Plasmodium Falciparum?
- Make thick and thin blood smears.
- Gametocytes are readily identified.
- Take a smear every 6 to 12 hours for another 48 hours.
- Advise serological tests.
- PCR.
How will you control mosquitoes?
- Try to eliminate breeding places:
- Fill the vacant land and pump out the water.
- Remove the junk and water-retaining debris.
- Destroy the larvae:
- Clean the drains.
- Try to remove algae from the ponds.
- Add larva-eating fish to the ponds.
- Use of the insecticide:
- The best example is DDT.
- Use of mosquito repellent:
- Pyrethroid repellent.
- N, N- diethyl meta tolbutamide.
- Use of mosquito nets.
- Use of clothes to prevent mosquito bites.
- Train people for malaria prevalence.
- Train the people for the detection of malaria, treatment, and follow-up.
How will you treat Plasmodium Falciparum?
- Antimalarial drugs are quinidine, chloroquine, primaquine, pyrimethamine, sulfadoxine, mefloquine, tetracyclines, and proguanil.
- Chloroquine is the drug of choice and is best for P. falciparum.
- This is effective for the erythrocytic stage and not for the liver stage.
- Must use primaquine to eradicate P. ovale and P. vivax.
- There are chloroquine resistant cases of P. falciparum.
- Amodiaquin, piperaquin and pyronaridine are close to chloroquin.
- In some areas, Amodiaquine is less toxic, cheap, and effective against chloroquine-resistant P. falciparum.
- Mefloquine is effective against choloquin resistant P. falciparum.
- Quinine and quinidine are still the first lines of therapy against P. falciparum.
- Primaquine is a synthetic drug and is the drug of choice for eradicating liver-stage from P. vivax and P. ovale.
- Antibiotics and Inhibitors of folate synthesis are slow-acting antimalarial drugs.
- Halofantrine and lumefantrine are related to quinine and are effective against the erythrocytic stage.
- Malaria drug-resistant strains are emerging.
Questions and answers:
Question 1: What is blackwater fever?
Question 2: What is the typical shape of gametocyte of plasmodium falciparum?