Malarial Parasite: – Part 1 – Plasmodium Life Cycle and Diagnosis
Plasmodium Life Cycle and Diagnosis
What sample is needed for a Malarial parasite?
- Malarial parasites (MP) may be diagnosed with a fever from a patient’s blood smear.
- The best time to make a smear is during shivering.
- Make thick and thin blood smears.
- A serum is needed for a serological method and PCR.
What are the indications for a Malarial parasites?
- The diagnosis of the malarial parasite infection.
How will you define Plasmodium?
- The Sporozoa of the genus Plasmodium are pigments-producing amoeboid parasites of vertebrates.
- These have one habitat in the RBCs and another in cells of other tissues.
- Spread in the human by the blood-sucking bite of female anopheles mosquitoes.
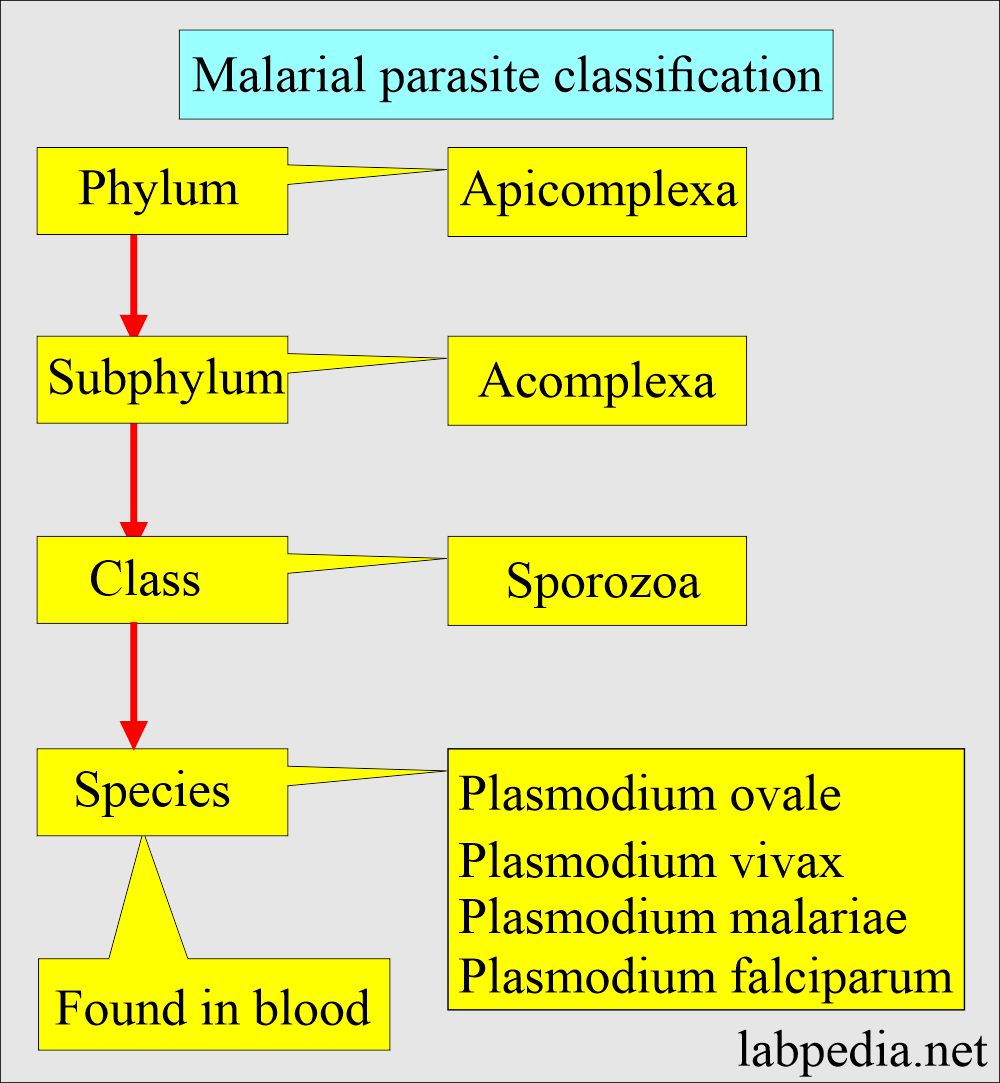
How will you discuss the parasitology of Malarial parasite?
- Malaria is the Italian word that means mala; aria means bad air.
- The plasmodium grows in the swamp-bred mosquito.
- Protozoan parasites cause malaria, are called Plasmodia, and belong to the Plasmodiidae family.
- Types of malaria parasites are :
- P. falciparum.
- P. vivax.
- P. ovale.
- P. malariae.
- A fifth one, P. knowlesi.
What is the vector of the malarial parasite?
- Mosquito species of the genus Anopheles transmit all the Plasmodium species, causing malaria in humans.
How will the malarial parasite spread?
- Sporozoites from the saliva of a biting female mosquito are transmitted to either the blood or the lymphatic system of the recipient.
- Malaria spreads through:
- Mosquito bite.
- Transfusion malaria from the contaminated transfused blood.
- By sharing contaminated needles and syringes, mostly the drug abusers.
- Congenital malaria is rare.
What are the different shapes of the Plasmodium?
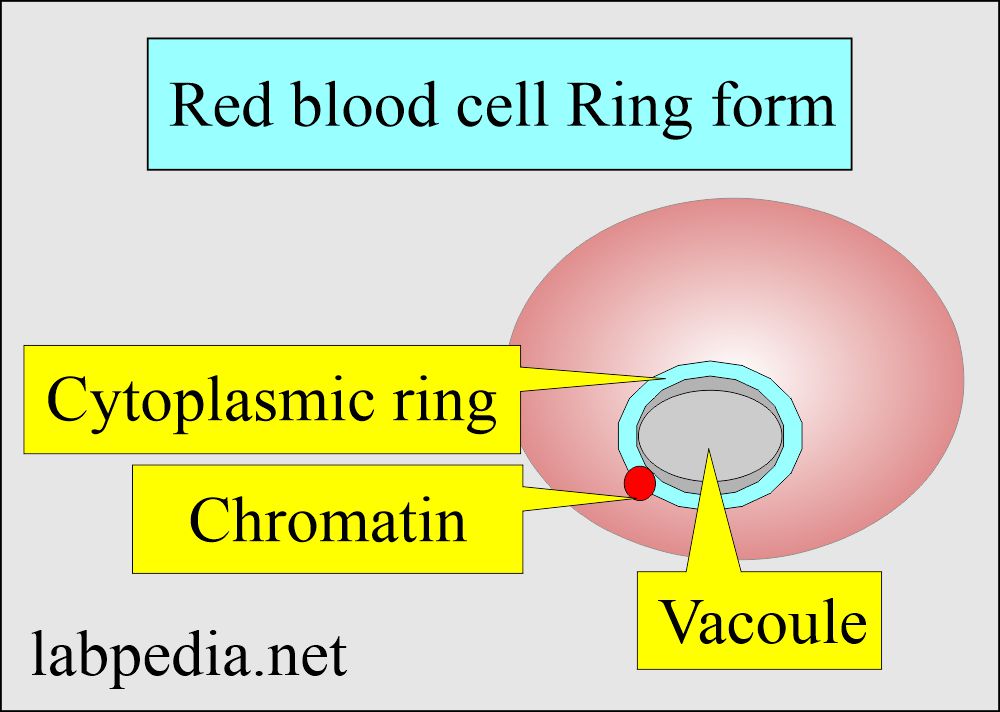
Ring form:
- It is an early trophozoite.
- This is a ring-like malarial parasite following the invasion of RBCs.
- Giemsa stain shows it as a blue stain cytoplasmic circle connected to a red chromatin dot.
- The space inside the ring is known as the vacuole.
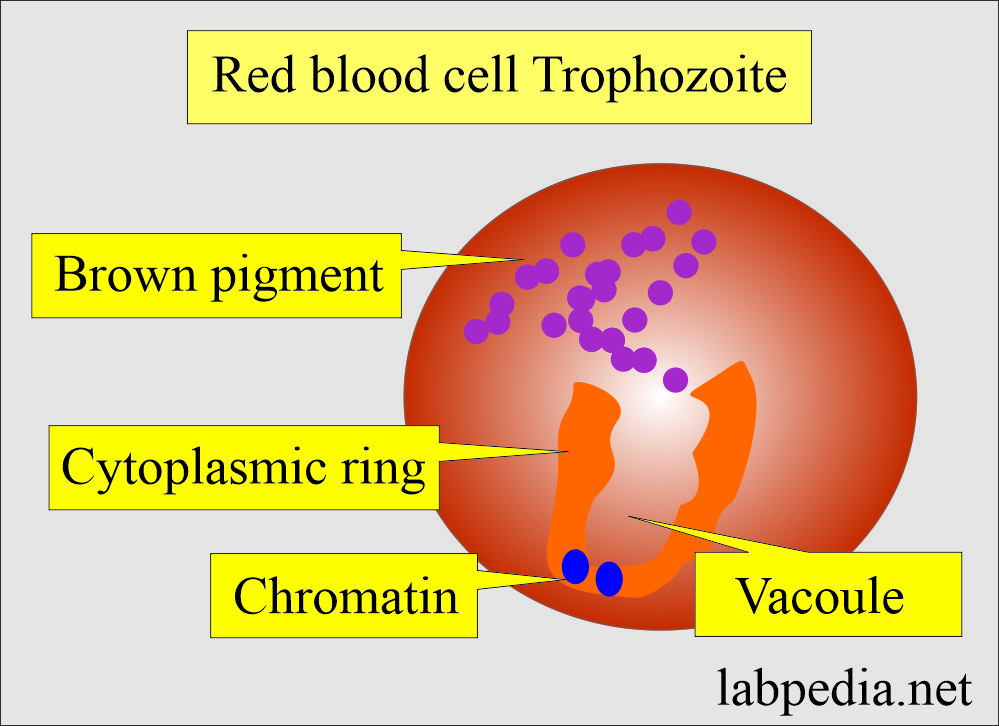
Trophozoites:
- The shape varies according to the type of malarial parasite.
- There are a cytoplasmic circle and a chromatin dot.
- More space is taken by the developing trophozoites.
- Pigments are brown in color.
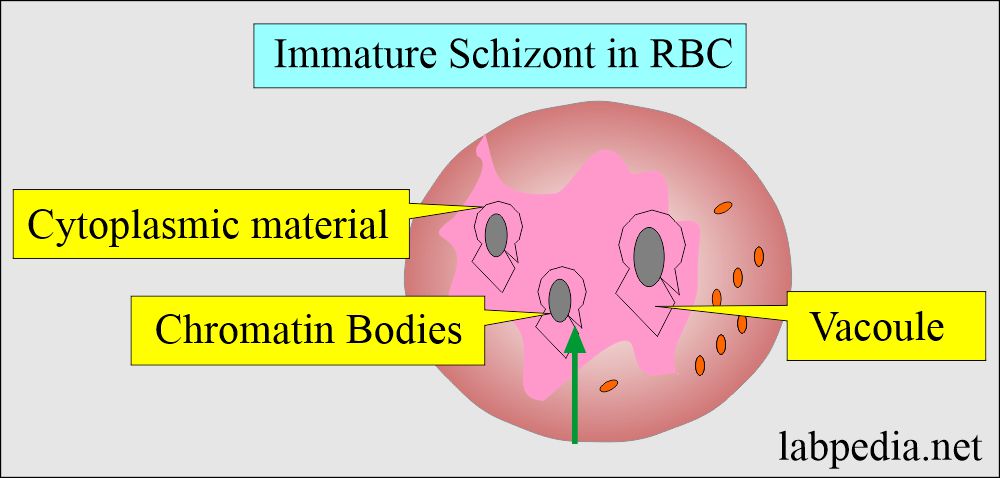
Immature schizonts:
- There is active chromatin replication.
- Visible cytoplasmic material surrounds the growing chromatin.
- Pigments are often brown.
- It occupies more space in the RBC.
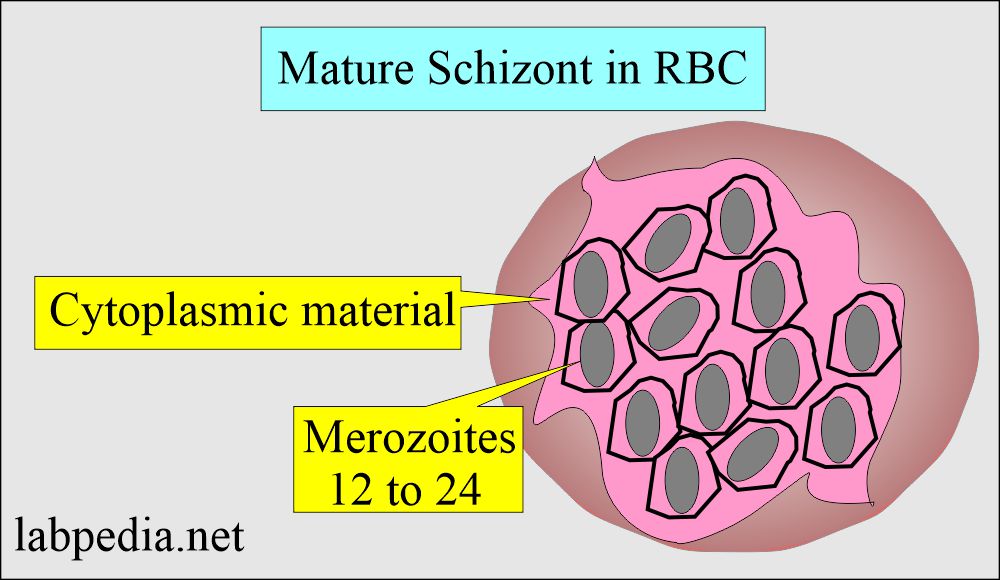
Mature Schizonts:
- These are characterized by the presence of merozoites.
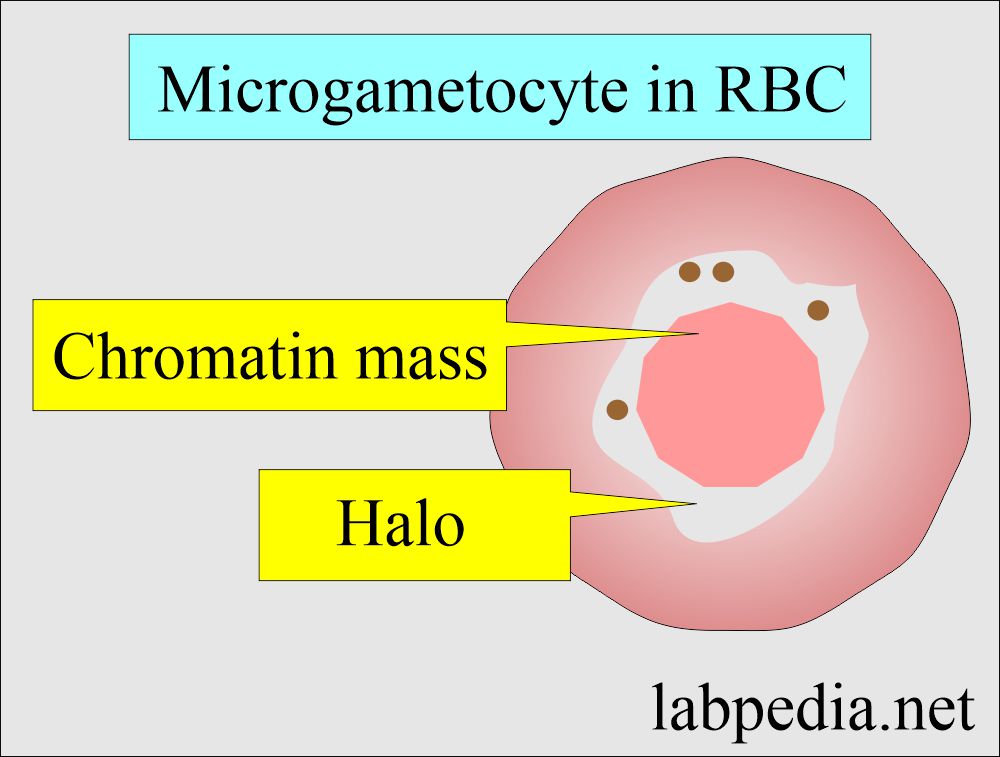
Microgametocytes:
- Plasmodium falciparum is crescent-shaped; in others, it is typically round.
- There is a large diffuse chromatin mass that stains pink to purple.
- A colorless pale halo surrounds the chromatin mass.
- Pigments are usually visible.
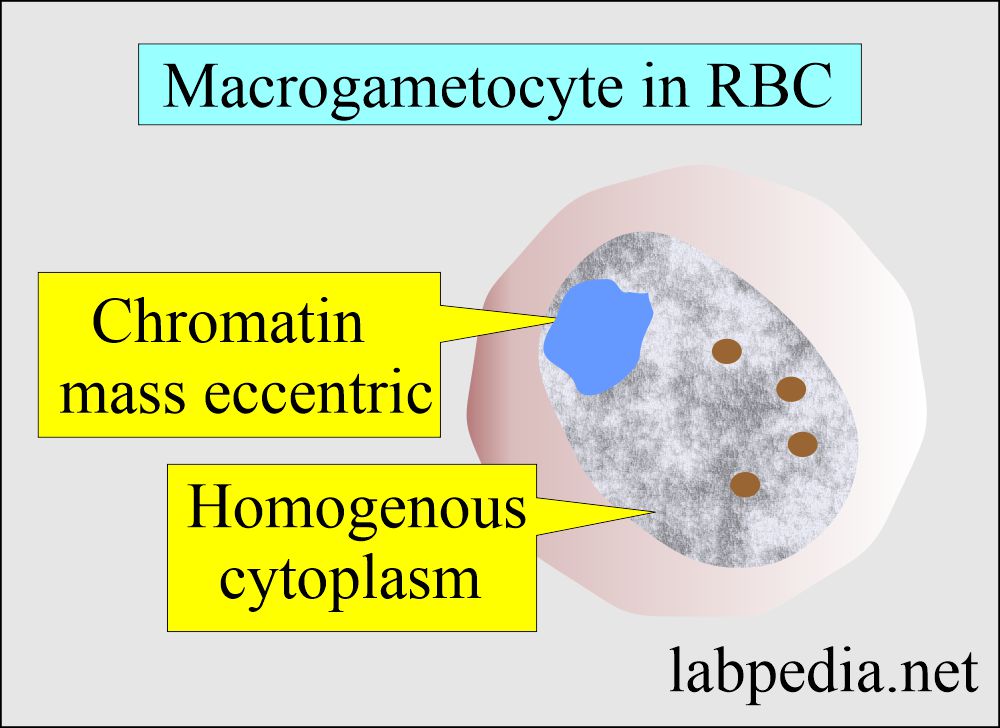
Macrogametes:
- These are round to oval in shape, with the exception of P. falciparum, which is crescent in shape.
- Chromatin is surrounded partially or completely by the cytoplasm.
- Pigments are also present.
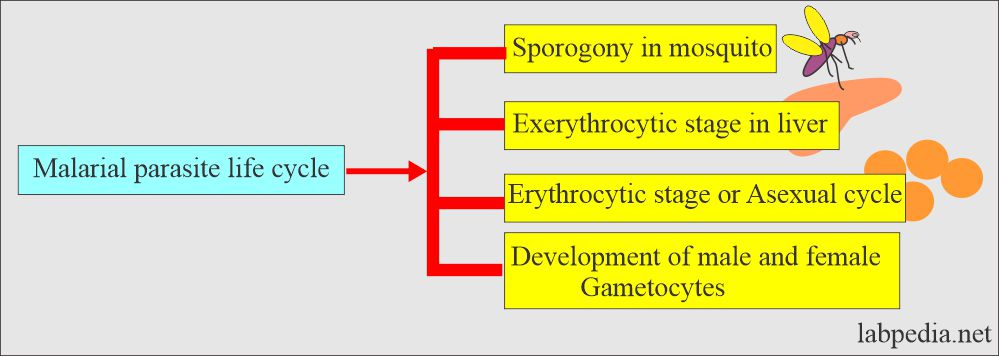
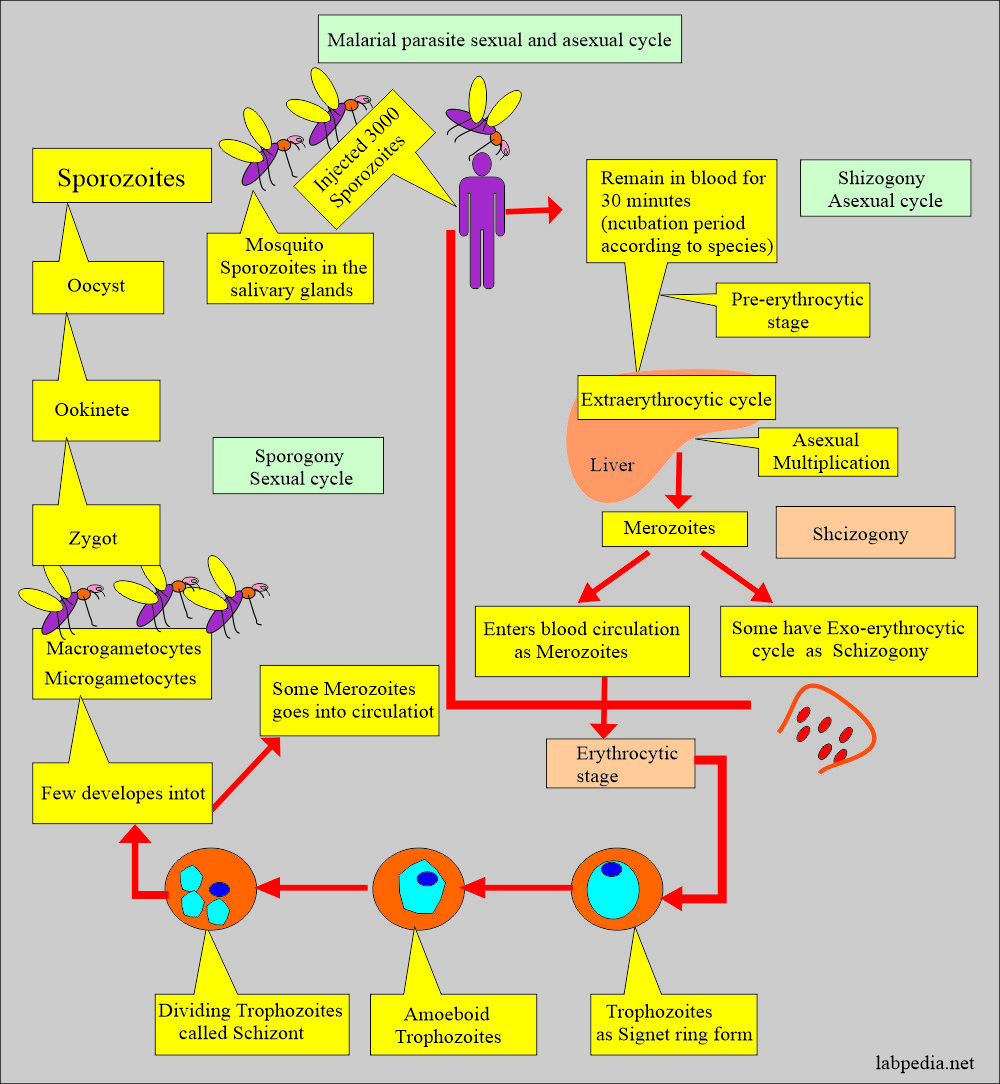
How will you discuss the lifecycle of a malarial parasite?
Asexual cycle:
- The majority of sporozoites migrate to the liver and invade hepatocytes.
- Initially, elongated sporozoite has transformed into a rounded form.
- This rounded form then matures within the hepatocyte to a schizont containing many merozoites.
- This cycle takes 5 to 16 days.
- Merozoites leave the liver and enter the blood; this is an asexual cycle.
The sexual cycle:
- It starts when the mosquito sucks the blood from the patients.
- Micro and macrogametocytes in the stomach of a mosquito combine and form a zygote.
- This forms oocyst and sporozoites.
- Sporozoites are injected into humans containing merozoites.
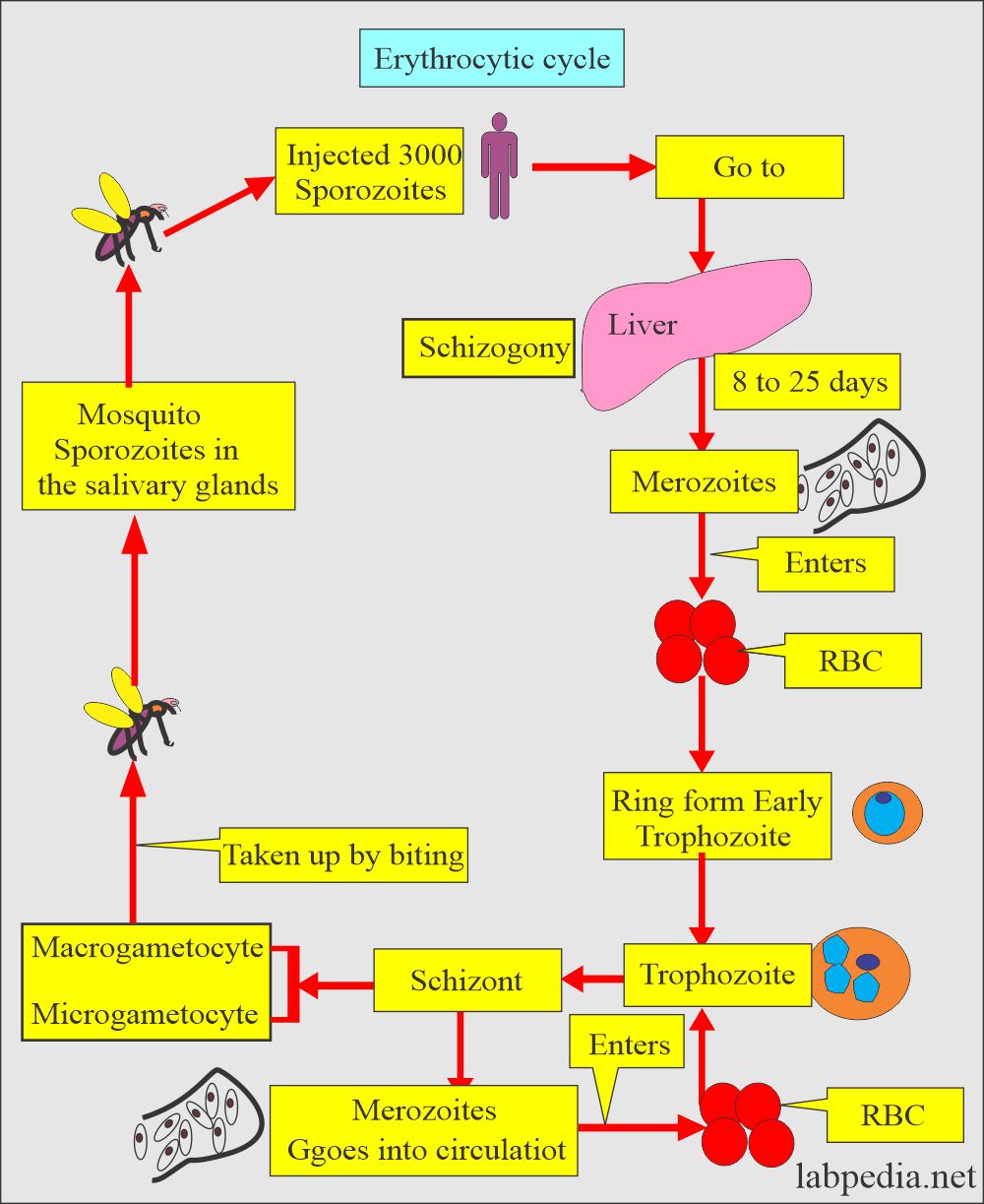
How will you describe the RBC cycle (Erythrocytic cycle) and the Asexual cycle?
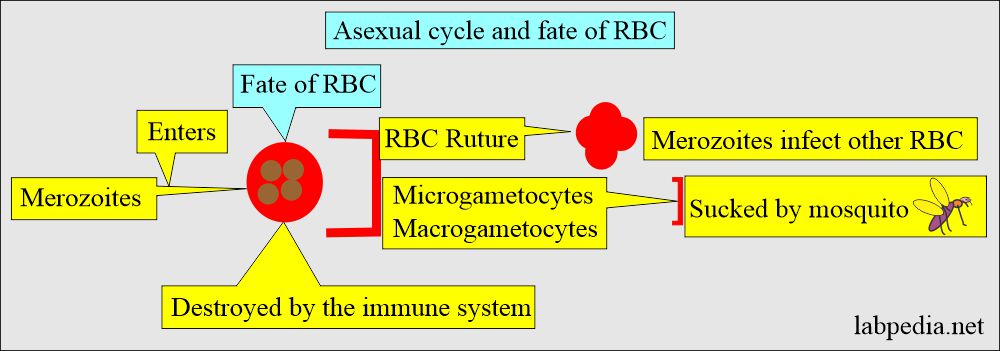
- Now, Merozoites enter the RBCs and start the Asexual cycle.
- Produce more merozoites. This cycle repeats for 1 to 3 days.
- This multiplication can result in thousands of parasite-infected cells in the host bloodstream.
- The patient may develop signs and symptoms of illness and complications of malaria.
- The complications of the malaria parasite, if not treated, may last for months.
- Some merozoites transform into a sexual form called male and female gametocytes.
- These gametocytes circulate in the blood and are taken up by the biting mosquito.
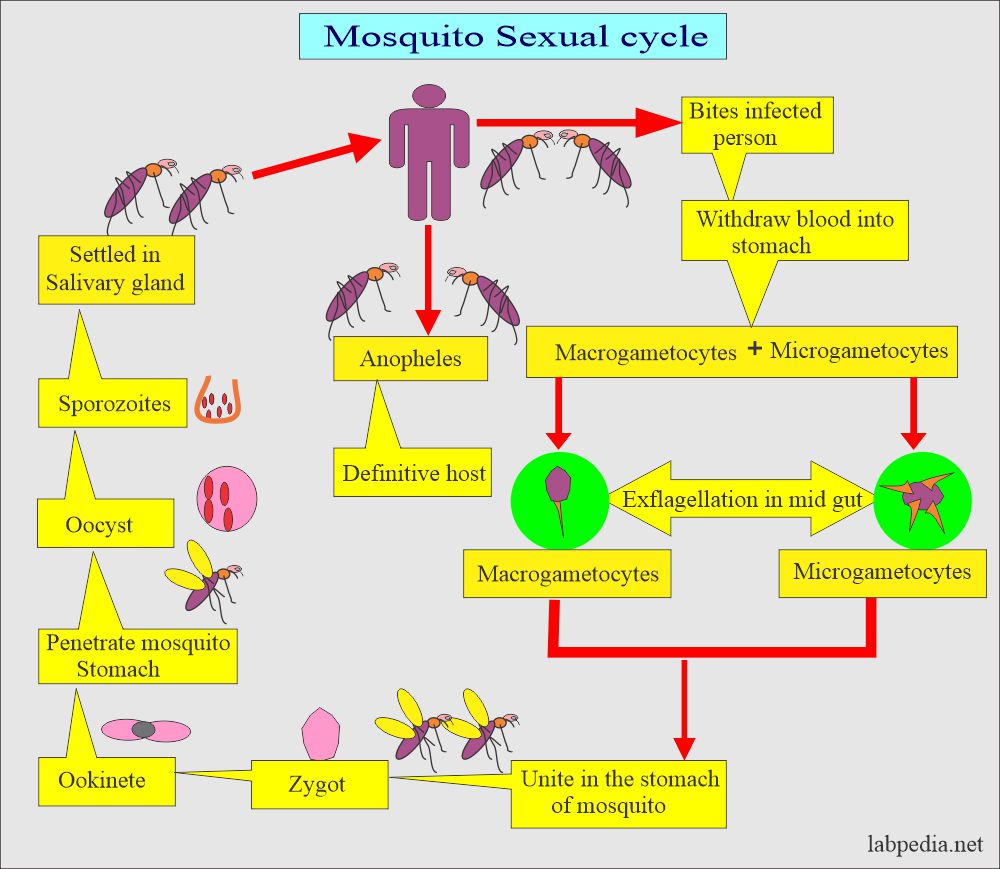
What is the life cycle of the mosquito (Sexual cycle)?
- When the mosquito bites the infected humans, it sucks the blood, and these gametocytes go along the blood.
- In mosquitoes, RBCs, bursts, and gametocytes are released. These will become more mature forms of Gametes.
- Male and female gametes fuse to form diploid zygotes.
- Zygotes develop into actively moving ookinetes that burrow into the mosquito midgut wall and form oocysts.
- Growth and division of each oocyst produce thousands of active haploid forms called sporozoites.
- After 8-15 days, the oocyst bursts, releasing sporozoites into the mosquito’s body cavity. These sporozoites travel to and invade the mosquito’s salivary glands.
- Mosquitoes are ready to infect humans.
What is the clinical presentation of the malaria parasite?
- The Typical patient is initially asymptomatic following the mosquito bite.
- Many RBCs rupture once the erythrocytic phase starts, releasing merozoites and toxic material.
- This is the time when patients get their first attack of malaria:
- First, chills for 10 to 15 minutes and then fever for 2 to 6 hours or more.
- When the fever settles to normal, then the patient gets profuse sweating.
- This cycle may vary with the type of malaria.
- The patient may have a headache, lethargy, anorexia, nausea, and vomiting.
- There may be diarrhea.
- There is anemia.
- The central nervous system may be involved.
- Kidney involvement may lead to nephrotic syndrome.
What are the complications of a Malaria parasite?
- The patient may have:
- Cerebral malaria.
- Anemia.
- Organ failure.
- Some patients may have respiratory difficulties.
- Rarely there may be low blood sugar levels.
How will you diagnose a malarial parasite?
- History of the patient in suspected areas.
- Blood shows thrombocytopenia and relative monocytosis is a common pattern.
- There is leucopenia.
- Bone marrow shows erythroid hyperplasia.
- The blood smear shows:
- Make a blood smear when the patient has a fever. Thin and Thick smears are made.
- The thick smear is more helpful in finding M.Parasites.
- A thick smear is sensitive to 2 parasites/1,000,000 uninfected RBCs.
- The thin smear is good for identifying the type of malarial parasite.
- Collect blood 6 to 8 hours weekly for 72 hours to declare negative for malaria.
- Giemsa stain is the best choice.
- Serologic methods are based on immunochromatic techniques. Tests most often use a dipstick or cassette format and provide results in 2-15 minutes.
- Polymerase chain reaction (PCR): The PCR technique detects parasite nucleic acids. It is more sensitive than smear microscopy, but it is of limited value for diagnosing acutely ill patients because of the time needed for this procedure.
- Flow cytometry to find infected RBCs.
- In the late stages, may see agranulocytosis and purpura may occur late.
How will you control mosquito-causing malaria?
- Try to eliminate breeding places:
- Fill the vacant land and pump out the water.
- Remove the junk and water-retaining debris.
- Destroy the larvae:
- Clean the drains.
- Try to remove algae from the ponds.
- Add larva-eating fish to the ponds.
- Use of the insecticide:
- The best example is DDT.
- Use of mosquito repellent:
- Pyrethroid repellent.
- N, N- diethyl meta tolbutamide.
- Use of mosquito nets.
- Use of clothes to prevent mosquito bites.
- Train people for malaria prevalence.
- Train the people for the detection of malaria, treatment, and follow-up.
What is the prevention of malarial parasites?
- No vaccine is available.
- Give prophylactic anti-malarial drugs.
- Use a mosquito net.
- Use mosquito repellant.
How will you treat malarial parasite infestation?
- Antimalarial drugs are quinidine, chloroquine, primaquine, pyrimethamine, sulfadoxine, mefloquine, tetracyclines, and proguanil.
- Chloroquine is the drug of choice and is best for P. falciparum.
- This is effective for the erythrocytic stage and not for the liver stage.
- Must use primaquine to eradicate P. ovale and P. vivax.
- There are chloroquine resistant cases of P. falciparum.
- Amodiaquin, piperaquin and pyronaridine are close to chloroquin.
- In some areas, Amodiaquine is less toxic, cheap, and effective against chloroquine-resistant P. falciparum.
- Mefloquine is effective against choloquin resistant P. falciparum.
- Quinine and quinidine are still the first lines of therapy against P. falciparum.
- Primaquine is a synthetic drug and is the drug of choice for eradicating liver-stage from P. vivax and P. ovale.
- Antibiotics and Inhibitors of folate synthesis are slow-acting antimalarial drugs.
- Halofantrine and lumefantrine are related to quinine and are effective against the erythrocytic stage.
- Malaria drug-resistant strains are emerging.
What are the characteristic features of various forms of the Malarial parasite?
| Malaria | Stages | Infected RBC size | Trophozoite | Scuffer stippling | GAMETOCYTES | Pigments (hematin) | Schizont Nuclei |
| P. vivax | All |
|
|
Present | Rounded or oval | light brown |
|
| P. Ovale | All |
|
|
Present | Rounded or oval | dark brown | 6 to 12 |
| P. malariae | All |
|
|
Absent | Rounded | dark brown | 6 to 12 |
| P. falciparum | ring- form |
|
|
Absent | Banana-shaped | black | rarely |
What are the clinical features of a Malarial parasite?
| Clinical parameters | P. falciparum | P. vivax | P. ovale | P. malariae |
|
8 to 11 days | 7 to 10 days | 7 to 10 days | 18 to 40 days |
|
Continuous, quotidian, or remittent | Irregular or quotidian | Irregular or quotidian | usually regular after 72 hours. |
|
Influenza-like | Influenza-like | Influenza-like | Influenza-like |
|
36 to 48 hours | 44 to 48 hours | 48 to 50 hours | 72 hours |
|
Severe 16 to 36 hours | Moderate to severe, 10 hours | mild for 10 hours | Moderate to severe, 11 hours |
|
2 to 3 weeks | 3 to 8 + weeks | 2 to 3 weeks | 3 to 24 weeks |
|
Very severe ++++ | ± | ± | ± |
|
Very severe ++++ | ++ | + | ++ |
|
+ | ± | – | +++ |
|
Normal size | Larger than normal, Schuffner’s dots are seen | Larger than normal, schuffner’s dots are often seen | About normal or slightly smaller |
|
About 1/5 of the diameter of RBC, chromatin is a small dot | About 1/3 diameter of RBC with heavy chromatin dots | Like vivax and malariae | single, heavy chromatin dot |
|
usually not seen in peripheral blood | as a large mass of chromatin, fine brown pigments | Chromatin is elongated and less definite. | |
|
8 to 24 or more merozoites | 12 to 24 merozoites | 4 to 16 but more common 8 merozoites | 6 to 12, but usually 8 or 10 merozoites |
| Macrogametocyte |
size like microgametocyte. Chromatin more compact |
The cytoplasm stains dark blue, and chromatin is more compact. | Abundant pigments and coarser, dark brown granules | |
|
Crescent-shaped, chromatin is diffuse, pink, cytoplasm pale blue | Round or oval, almost fill the RBC, chromatin is diffuse in large masses, pink, no vacuoles | Like vivax but smaller | like vivax but smaller and pigments more prominent |
|
10 to 12 days at 27 °C | 10 days at 25 °C to 30 °C | 14 days at 27 °C | 25 to 28 days at 24 °C |
Duration of the various cycles in malarial parasites:
| Type of malarial parasite | Sexual cycle in the mosquito | Length of asexual cycle | Length of the sexual cycle |
| Plasmodium falciparumm | 9 to 10 days | 5 to 7 days | 36 to 48 hours |
| Plasmodium vivax | 8 to 9 days | 8 days | 48 hours |
| Plasmodium ovale | 14 days | 9 days | 48 hours |
| Plasmodium malariae | 15 to 20 days | 15 to 16 days | 72 hours |
Questions and answers:
Question 1: Which malarial have banana shape gametocyte?
Question 2: Is there a vaccination for malaria?