Leishmaniasis, Cutaneous and visceral leishmaniasis (Oriental Sore and Kala-azar)
Leishmaniasis
What sample is needed for Leishmaniasis?
- Prepare a smear from the lesion of the patient.
- Spleen, tissue or aspirate, and (FNA) of lymph nodes.
- Splenic puncture.
- Nasal smears.
- Bone marrow aspirate.
- Culture from the above samples.
- Buffy coat of peripheral blood.
What are the indications for Leishmaniasis?
- This helps in the diagnosis of Cutaneous Leishmaniasis or oriental sore.
- For diagnosis of visceral leishmaniasis.
How will you define Leishmaniasis?
- A protozoan of the genus Leishmania causes leishmaniasis.
- Leishmania includes many species, which may cause more than one clinical syndrome.
- Leishmania causes three syndromes:
- Visceral leishmaniasis is called Kala-Azar.
- Cutaneous leishmaniasis is localized or widespread.
- Mucosal leishmaniasis.
How will you discuss the pathophysiology of Leishmaniasis?
- Leishmaniasis is caused by a protozoan of the genus Leishmania, which causes many syndromes.
- The sandfly transmits cutaneous Leishmania (CL).
- The genus of protozoa comprises parasites of worldwide distribution.
- It is best known in the Middle East and occurs in the Far East. It is not seen in Japan.
- It is seen in various areas of Africa, Central and South America, the Island of the Caribbean, and occasionally the European side of the Mediterranean area.
- Several species of which are pathogenic to humans. All species are morphologically indistinguishable.
- These are divided into the Clinical syndromes they produce:
- Visceral (Kala-Azar):
- This is a chronic systemic disease associated with the following:
- Leishmania donovani.
- Leishmania infantum.
- Leishmania chagasi.
- Cutaneous (Localized or widespread).
- Mucocutaneous.
How would you classify Leishmania?
- L. donovani.
- L. tropica.
- L. Mexicana.
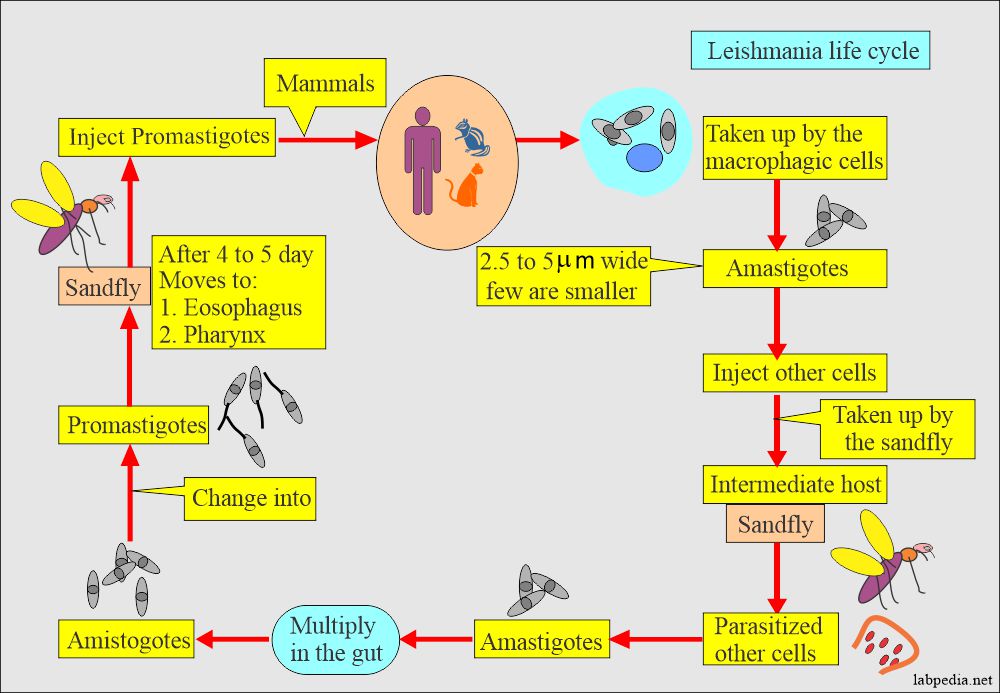
How will you summarize the Leishmania life cycle?
- Leishmania is zoonotic and carried by rodents, dogs, and foxes transmitted to humans by biting sandflies (Phlebotomus).
- Promastigote invades phagocytic cells (macrophages) from the sandfly bite and transform into nonmotile amastigotes.
- Amastigotes multiply in the macrophagic cells of lympho nodes, spleen, liver, and bone marrow.
How will you discuss the Cutaneous leishmaniasis?
- Cutaneous leishmaniasis is divided into Old-world and New-world types.
Leishmania tropica:
- L. Tropica complex consists of the following:
- L. tropica.
- L. major.
- L. aethiopica.
- This complex causes Oriental sore, also called Baghdadi boil, old world cutaneous leishmaniasis, or Delhi ulcer.
- This is transmitted by sandflies belonging to the genus Phlebotomus.
- Epidemiology:
- These lesions are seen in the Mediterranean littoral, Armenia, Azerbaijan, Uzbekistan, Turkmenistan, Afghanistan, India, Pakistan, and Iran.
- The dog may be the natural host, but it does not look like an effective reservoir for a human.
- Incubation time is 2 months to 3 years.
- Cutaneous leishmaniasis generally causes skin lesions, persisting for months, sometimes years.
- The skin lesions usually develop within several weeks or months after exposure.
- These lesions are usually on the face.
- The lesions typically evolve from dry papules to nodular plaques to ulcerative lesions.
- These ulcers are usually 2 cm in Diameter or more with typical itching.
- These lesions have raised borders and central depression, which can be covered by scab or crust.
- Rarely do some lesions persist as nodules.
- These lesions are painless but sometimes may give rise to pain when infected.
- The healing process typically results in atrophic scarring.
Leishmania Major:
- It produces an acute infection with a duration of 3 to 6 months.
- The lesion primarily occurs on the lower limbs.
- These lesions are moist and tend to ulcerate very early.
- There may be secondary lesions on other sites.
- This disease is seen in Turkmenistan, Uzbekistan, Iran, Kazakhstan, Syria, Israel, Jordan, Africa, Algeria, Sahara, Tunisia, Sudden, Nigeria, Niger, Mali, Senegal, and Kenya.
Leishmania Mexicana:
- This causes new world cutaneous leishmaniasis
- It causes a Chiclero ulcer or Bay sore.
- It is found in Belize, the Yucatan peninsula, and Guatemala.
- It is endemic in these areas.
- The amastigotes are found in the skin lesions of humans, wood rats, and cats.
- Lesions are usually single, and 40% involve ears.
- This may give rise to the diffuse cutaneous lesion.
How will you discuss the Signs and symptoms of Leishmaniasis?
- The first sign of the infection is a red papule.
- There is itching, which may grow to 2 cm or more in diameter.
- In L. major infection, the papule is covered with serous exudate and ulcerates early.
- In L. tropical, papules are dry and ulcerate only after several months.
- This cutaneous form may be seen as:
- Diffuse cutaneous leishmaniasis may be due to lake cell-mediated immunity.
- Leishmaniasis recideva is due to good antibody and cellular response. In this case, the central lesion heals, and the peripheral area is active.
How will you diagnose cutaneous leishmania?
- Organisms are diagnosed by direct smear and microscopy.
- Culture will be positive from the lesion.
Mucocutaneous Leishmaniasis:
- It is the least common syndrome, and it occurs in Central and South America.
- It follows after the cutaneous leishmania.
What causes mucocutaneous Leishmaniasis?
- Leishmania braziliensis causes mucocutaneous leishmaniasis, also called espundia and uta.
- There is the formation of an ulcer on the oral-nasal mucosa.
- This is common in Brazil.
- The cutaneous lesions are multiple and large.
- Secondary infection plays a role in the persistence of the large size lesion.
- Signs and symptoms:
- Sometimes, it spreads to the mucous membranes.
- The entire nasal mucosa and the hard and soft mucosa are involved.
- The nasal septum will be destroyed.
- But unlike syphilis, the bone is not involved.
- The ulceration leads to losing all soft parts of the nose, lips, and palate.
- Death may occur in these patients due to secondary infection.
- A similar disease is also seen in Sudan and Ethiopia.
- How will you diagnose mucocutaneous leishmania?
- Organisms are identified by histologic examination in scrapings or biopsy from the lesion.
- Culture can be done and is positive in 50% of the cases.
- Positive immunofluorescent antibody test.
- PCR gene amplification for Leishmania DNA or culture.
Visceral leishmaniasis (Kala-Azar)
What causes visceral leishmaniasis (Kala-Azar)?
- Leishmania donovani causes it.
Leishmania donovani:
- Three types of Leishmania Donovani complex cause it:
- L. Donovani donovani.
- L. Donovoni chagasi.
- L. Donovani infantum.
- It causes visceral leishmaniasis, called Kala-azar or black disease, Dumdum fever.
- This occurs in India, Burma, Bangladesh, Thailand, and Sumatra.
- Also seen in the Central African Republic, Sudan, Kenya, Gambia, Gabon, Northern Uganda, and Niger.
- This was seen in China, but now it is controlled.
- Vector is Phlebotomus sandflies.
- L. tropica has been found in some cases, including a few cases in India and veterans from the Gulf War.
- The causative agent is a parasite of the reticuloendothelial system.
- This is not confined to the reticuloendothelial cells of the subcutaneous tissue and mucous membranes but may be found throughout the body.
- What are the signs and symptoms of Kala-azar?
- The Visceral leishmaniasis (also known as Kala-Azar).
- No skin lesions are seen, rarely except a papule at the site of the bite.
- Fever.
- Weight loss (cachexia, wasting).
- Hepatosplenomegaly (usually, the spleen is more prominent than the liver).
- It returns to normal after the treatment.
- Bone marrow, when involved, gives rise to:
- Pancytopenia, i.e., anemia (normocytic and normochromic), leukopenia, and sometimes thrombocytopenia.
- TLC is usually below 4000/cmm and is between 2000 to 3000/cmm.
- There is a monocytosis.
- High total protein level and a low albumin level, with hypergammaglobulinemia.
- Lymphadenopathy may be noted in some geographic regions, such as Sudan.
- HIV-coinfected patients may have atypical manifestations, such as gastrointestinal and other organ systems involvement.
- What is the meaning of Kala-azar?
- It means black (kala) fever (Azar). These are severe (advanced) cases of visceral leishmaniasis.
- Kala-azar or severe visceral leishmaniasis untreated is typically fatal due to:
- Directly from the disease.
- Indirectly from complications, such as hemorrhage or secondary bacterial infection.
- If untreated, the mortality rate may reach 100% within two years (WHO).
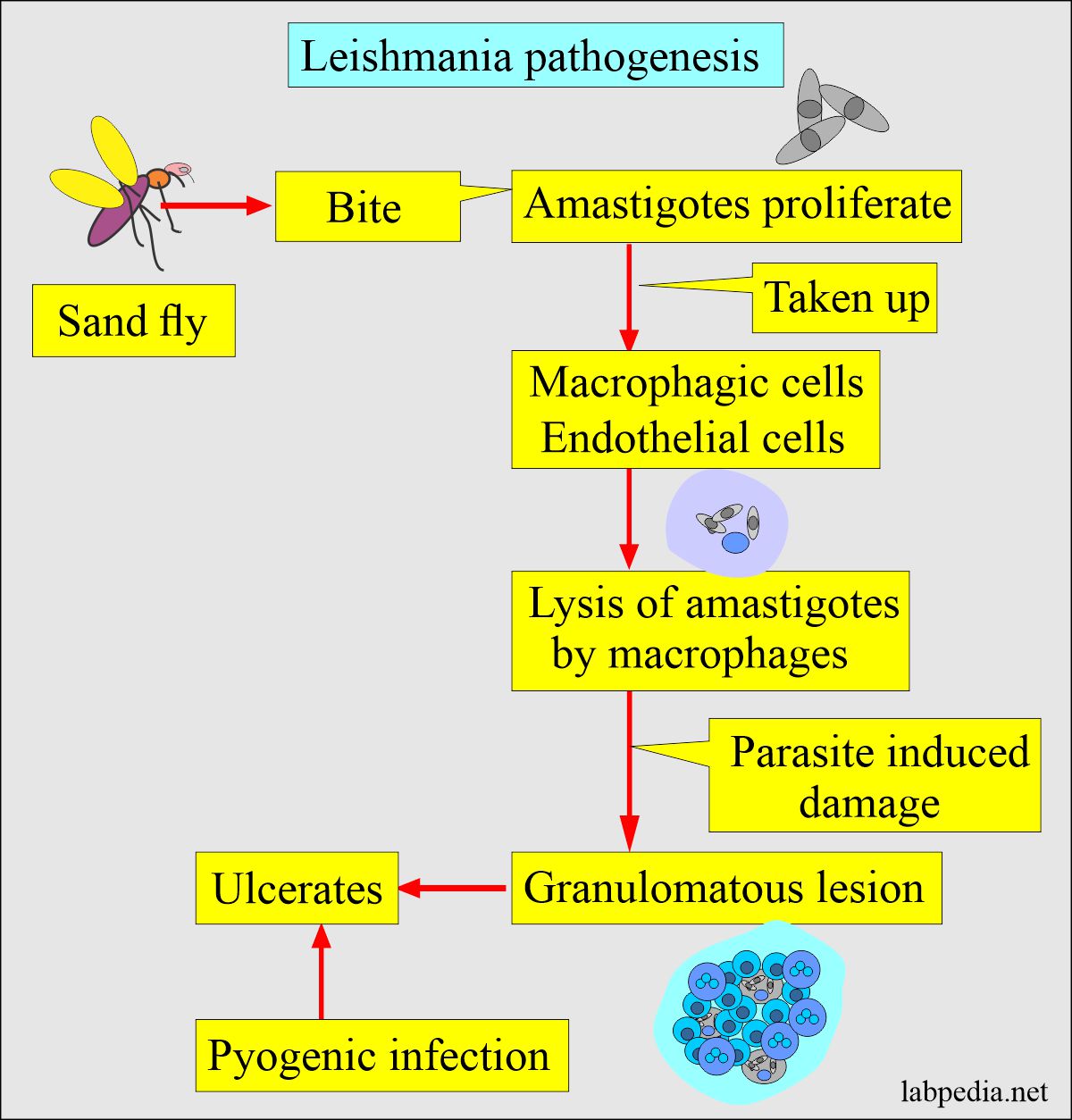
How will you discuss the Pathogenesis of the lesion (Leishmaniasis)?
- The fly, when biting the host, then amastigotes proliferate.
- The macrophages and the endothelium of the small capillaries take these up.
- Macrophagic cells cause the lysis of amastigotes.
- The organism infects the mononuclear cells of the reticuloendothelial system.
- The incubation period varies from 2 weeks to more than 2 years and is mostly 3 to 8 months.
- A chronic granulomatous reaction leads to local nodule formation due to parasite-induced damage.
- This may ulcerate, and there is the possibility of pyogenic infection.
What is the mode of the spread of Leishmania?
1. Leishmania spreads through the bite of the female sandfly (Phlebotomus).
2. Humans are a natural source of a reservoir. Other reservoirs are dogs, wild canines, rodents, and humans.
How will you diagnose Leishmaniasis?
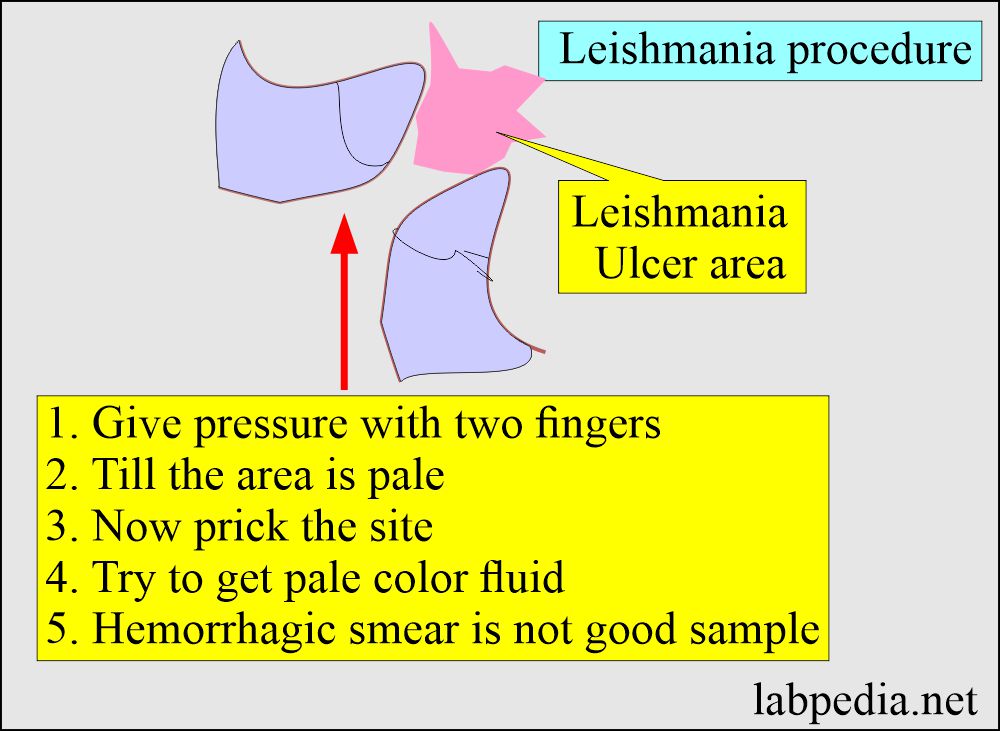
What is the procedure to get a positive yield in cutaneous lesions?
- If the ulcer is on the arm or feet, first try applying pressure to stop the blood supply to that area.
- Now prick and try to get yellow color material or serum-like material.
- Make a smear from this material.
- Another method is to take a sample like Fine needle aspiration (Author’s personal experience ).
- The FNA method is done at the periphery of the ulcer and gets a good sample most of the time.
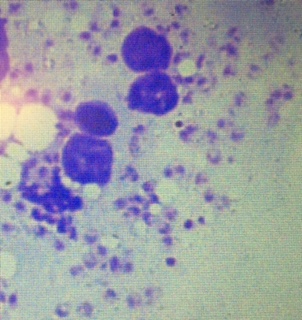
Give an interpretation of the cutaneous smears?
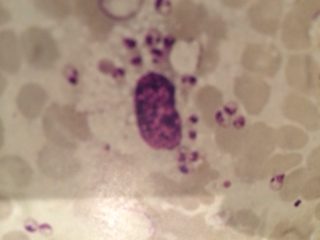
- In a good smear, you will see a lot of LT bodies in the histiocytes and outside on the smear.
- Also, can find a single separate LT body
Find amastigotes from the various areas:
- L. tropica is diagnosed by making the smear from the deeper area of the skin lesion.
- These smears are stained with Giemsa (or Wright’s) stains. Typical amastigotes are seen.
- Material aspirated from the bone marrow (64% to 86% positive), spleen (95 to 98% positive), or enlarged lymph nodes (roughly 64% positive).
- Make a smear from the nasal secretion in case of a mucocutaneous lesion.
- From the buffy coat of peripheral blood (67% to 99% positive).
- The culture of aspirates or peripheral blood.
- Can find the Leishmania antibody using the known parasitic antigen.
- Leishmania amastigotes (LT body) are seen in the monocytes, and a few are seen as single in the smear.
- Serological tests:
- Serological tests are in the form of ELIZA, IFA, CIE, direct agglutination, and IHA.
- ELIZA and indirect fluorescent antibody assay.
- PCR of the tissue or WBC buffy coat has been used in NIH.
- A marked increase in serum globulin (IgG) with decreased albumin and a reversed A/G ratio.
- Culture: Incubate at 26°C from the lesion, taking up to 4 weeks.
- Hematological tests:
- ESR is raised due to increased serum globulin.
- There is anemia and leucopenia.
- There is thrombocytopenia due to hypersplenism and decreased bone marrow proliferation.
- There may be proteinuria and hematuria.
- In chronic cases, you may see amyloidosis.
How will you treat Leishmaniasis?
- The best drug is Sodium stibogluconate (antimony sodium gluconate (Pentostam).
- Pentostam 20 mg/Kg body weight is injected I/V or I/M for 20 days for cutaneous leishmaniasis.
- This dose can be repeated in the resistant cases at 10-day intervals.
- A maximum of three courses can be given.
- Pentostam 20 mg/Kg body weight is injected I/V or I/M for 20 days for cutaneous leishmaniasis.
- Another drug is:
- Meglumine antimonate (Glucantime).
- Initial 50 mg/Kg body weight given for 10 to 12 days for cutaneous leishmaniasis.
- For mucocutaneous, give treatment for 15 days and repeat after 15 to 20 days if healing is incomplete.
- Pentamidine.
- Oral Ketoconazole 400 mg daily for 4 to 8 weeks effectively treating longstanding cutaneous leishmaniasis.
- Steroids
- Meglumine antimonate (Glucantime).
Question 1: What is the best way to get a good smear from the skin.
Question 2: What is Kala-Azar.


very nice ………
Thanks. Please see the link.
https://labpedia.net/leishmaniasis-cutaneous-and-visceral/