Ulcerative Colitis and Crohn’s Disease
Ulcerative Colitis
How will you define Ulcerative Colitis?
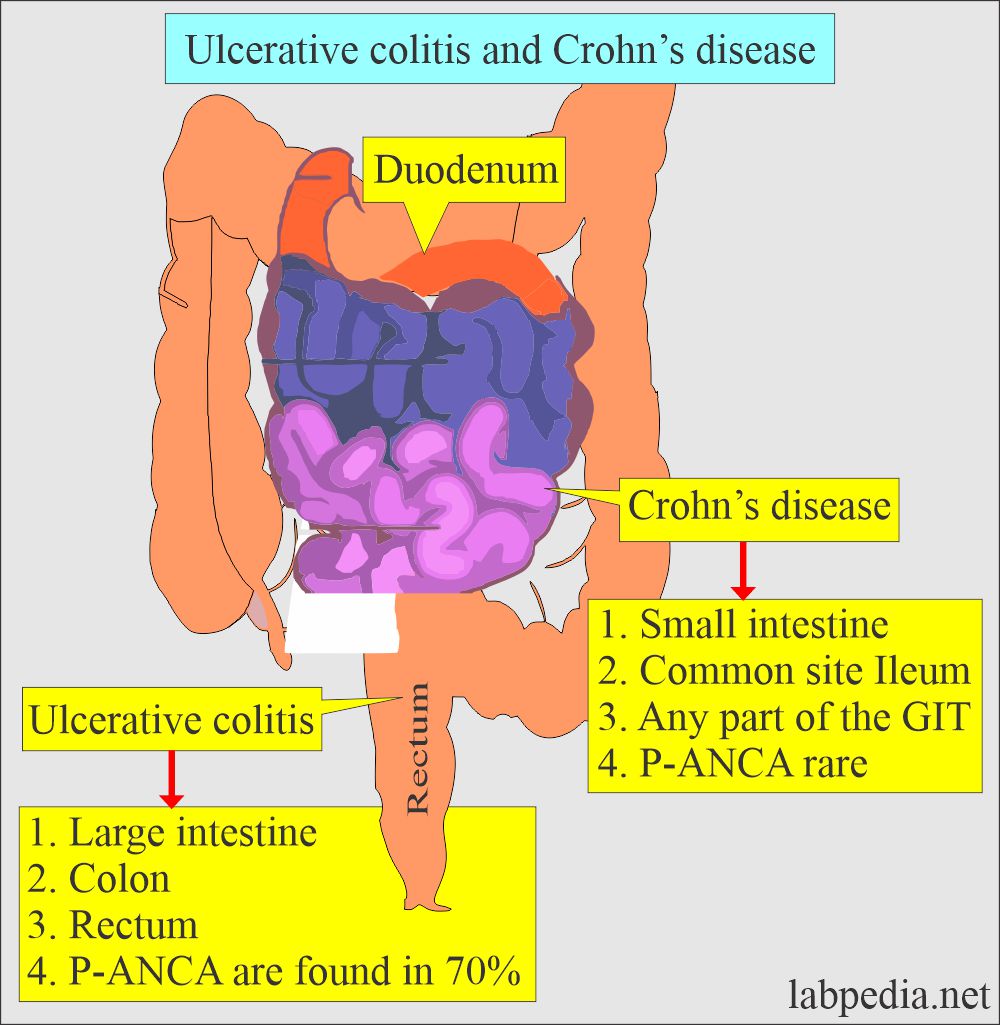
- Ulcerative colitis is an inflammatory bowel disease (IBD) that affects only the large intestine (colon and rectum).
- It is marked by the diffuse, superficial inflammation of the colonic mucosa, starting in the rectum and spreading to the neighboring length of the colon.
- The small intestine is mostly not involved.
What is the pathogenesis of Ulcerative colitis?
- This is considered to be an autoimmune disease.
- This is due to inflammation caused by the immune system, mainly in the large intestine.
- Ulcerative colitis is classified as:
- Proctitis, limited to the rectum.
- Proctosigmoiditis or left-side colitis, where it extends to splenic flexure.
- Pancolitis, where it extends to the transverse colon.
- The severity of ulcerative colitis depends upon the length of the colon and the severity of the inflammation.
- Mild disease.
- Moderate disease.
- Severe disease.
- Fulminant ulcerative colitis.
What are the histologic features of ulcerative colitis?
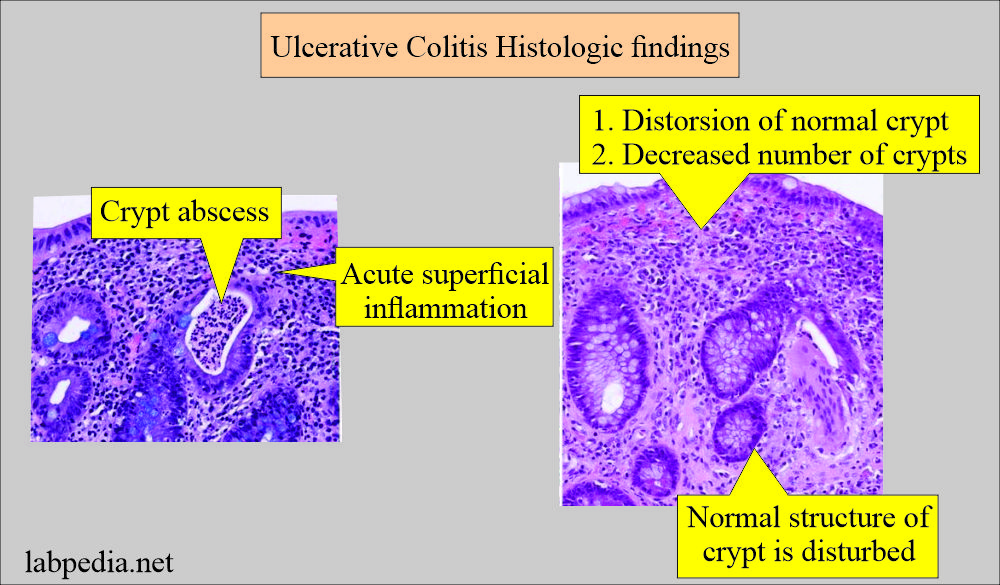
- Histologically, we can see the following changes:
- Acute superficial inflammation with distortion of the normal crypt structure.
- Next stage, you may see a crypt abscess.
- There is no inflammation in the dormant stage of ulcerative colitis, but the normal architecture of the crypts is disturbed; there are branched abnormal crypts.
What are the signs and symptoms of Ulcerative colitis?
The following are the signs and symptoms of Ulcerative colitis.
- Ulcerative colitis is insidious in onset. There is no history of abrupt onset.
- Diarrhea, often with blood or pus.
- Diarrhea is the passage of mucus without a stool, indicating the extent of the colon’s involvement.
- Abdominal pain and cramping preceding bowel movements are common.
- Abdominal pain or tenderness on palpation indicates transmural inflammation, which is a sign of severe disease.
- Rectal pain.
- Rectal bleeding: A small amount of blood is passing with stool, and this is a consistent feature.
- Bleeding is variable; it may be gross or microscopic.
- The urgency to defecate, and there is tenesmus.
- Inability to defecate despite the urgency.
- Systemic symptoms seen are:
- Night sweating.
- Nausea and vomiting.
- Weight loss.
- Fatigue.
- Fever.
- Extraintestinal symptoms may include eye, skin, liver, and joint inflammation.
- In children, failure to grow.
How will you diagnose ulcerative colitis?
- The diagnosis of ulcerative colitis depends upon the following:
- Clinical history of the patients.
- Finding on endoscopy.
- Histologic findings on biopsy.
- The barium enema is replaced by endoscopy.
How will you treat Ulcerative Colitis?
It includes:
- Medicine.
- Diet.
- Surgery.
Crohn’s disease
How will you define Crohn’s disease?
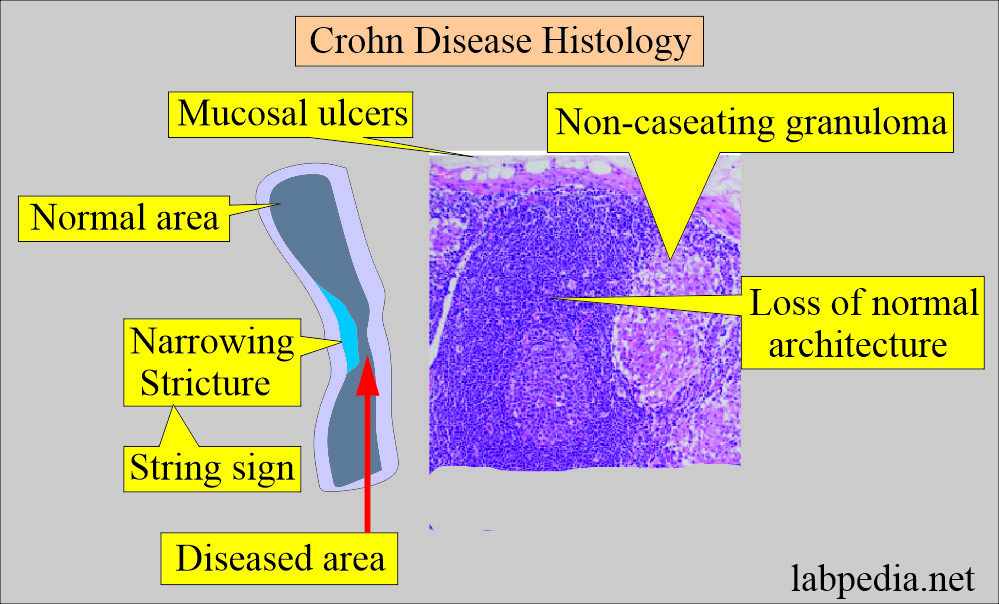
- Crohn’s disease is focal, asymmetrical, and transmural inflammation of the digestive tract.
- In some cases, you may see granuloma formation.
- The inflammation is patchy.
How will you discuss the pathogenesis of Crohn’s disease?
- It is an inflammatory bowel disease. In comparison, Crohn’s can affect any part of the gastrointestinal (GI) tract from mouth to anus.
- Its cause is unknown.
- Inflammation is patchy, may be transmural, and can involve any segments of the gastrointestinal tract.
- Crohn’s disease inflammation may lead to complications like stricture and fistula of the intestine.
- You may find noncaseating granulomas. These granulomas are seen in only 30% of the patients.
- Granulomas are not important for the diagnosis of Crohn’s disease.
- Diet and stress were suspected, but now doctors know these factors may aggravate but don’t cause Crohn’s disease.
- A number of factors, such as heredity and a malfunctioning immune system, likely play a role in its development.
What are the histologic findings of Crohn’s disease?
- Crohn’s disease produces a spectrum of inflammation.
- There may be superficial inflammation like ulcerative colitis.
- There may be fibrosing stricture.
- Inflammation may cross the intestinal wall and produce fistulas. This process may lead to mesenteric inflammatory mass or perienteric abscess formation.
- Noncaseating granulomas occur in >60% of cases and only 6% of ulcerative colitis cases.
What are the signs and symptoms of Crohn’s disease?
The following are the main signs and symptoms of active Crohn’s disease.
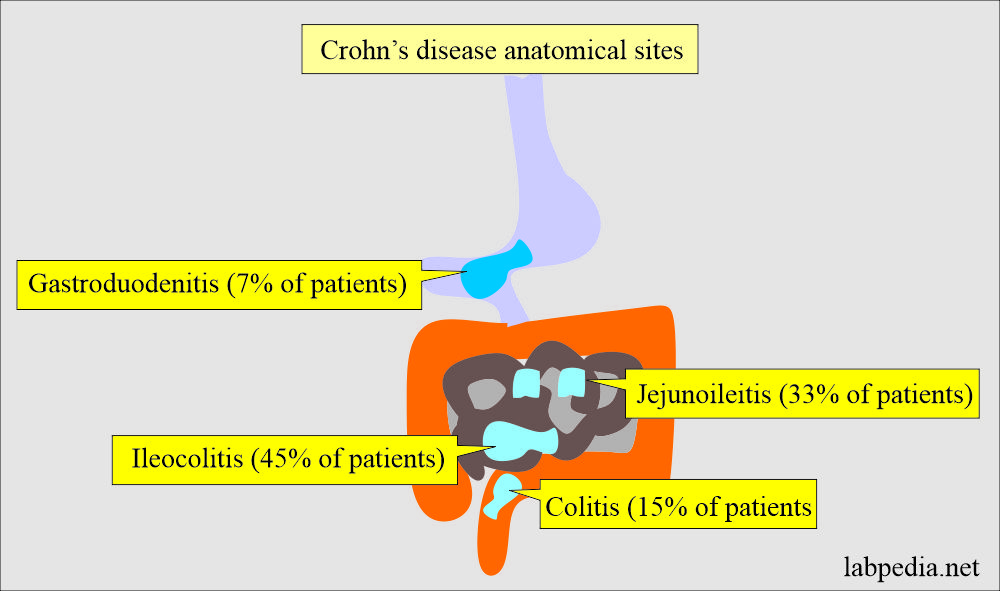
- Crohn’s disease most frequently affects the terminal ileum and cecum, but it can also affect various parts of the gastrointestinal tract.
- Chron’s disease of the esophagus, stomach, and duodenum.
- Chron’s disease of jejunoileitis.
- Chron’s disease is ileitis and ileocecal areas.
- Chron’s disease colitis.
- Crohn’s disease involves different anatomical sites.
- Perianal Crohn’s disease.
- Diarrhea with cramps.
- Fever and fatigue.
- Abdominal pain and cramping.
- Blood was seen in the stools.
- Mouth ulcers.
- There is a decrease in appetite.
- There is weight loss.
- The perianal area is involved.
How will you diagnose Crohn’s disease?
- Crohn’s disease is diagnosed based on the following:
- Clinical history of the patient.
- Radiographic changes.
- Endoscopy findings.
- Histologic criteria on biopsy tissue.
- Most patients are anemic. This is due to iron deficiency, vitamin B12, or folic acid.
- Anemia may be a chronic disease.
- Leucocytosis is common.
- Thrombocytosis is common, and this may be related to inflammation or iron deficiency.
- ESR is raised. C-reactive protein is positive.
- Serum albumin is reduced due to inflammation or enteric protein loss.
- Serological test: Anti-Sac-charomyces cerevisiae antibody and antibody to the outer core of the E.coli are positive.
- Radiographic findings are diagnostic of Chron’s disease.
- Barium studies will show complications like strictures or fistulas.
- Colonoscopic studies of Chron’s disease are more diagnostic.
- It will show the sparing of the rectum with focal inflammatory changes in the proximal colon and terminal ileum.
- The histology of the biopsy shows an aphthous ulcer.
- Minute ulceration extends as linear or transmural.
- There is a mixed inflammatory infiltrate of lymphocytes, plasma cells, and neutrophils.
- Nonspecific chronic noncaseating granuloma is seen on biopsy or resected segments of the intestine.
How will you treat Crohn’s disease?
- It depends upon the location, extent, and severity of the disease,
- Treatment is focussed on remission and then trying to maintain the remission.
- It is treated like irritable bowel syndrome.
- Surgery is indicated in a few cases with complications.
- Can try anti-inflammatory agents like Aminisalicylates and corticosteroids.
How will you differentiate Ulcerative Colitis from Crohn’s Disease?
| History/Pathologic findings | Ulcerative colitis | Crohn’s disease |
| History of smoking | Non-smoker or ex-smoker | Mostly smoker |
|
There may be :
|
There may be:
|
| Location | ||
|
— | ++ |
|
++ | + — |
| Skip lesion | — | + |
|
++ | — |
|
— | ++ |
Gross appearance |
||
|
++ | — |
|
+ — | ++ |
|
+ — | ++ |
|
+ — | ++ |
|
— | ++ |
|
++ | — |
Microscopic appearance |
||
|
++ (Quite common) | — (Not seen) |
|
— (Only 6% of the cases) | ++(>60% of the cases) |
|
— | ++ |
|
— | ++ |
|
— | ++ |
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
Questions and answers:
Question 1: What is the characteristic feature of ulcerative colitis?
[question-answer number=”2″ question=” Can you differentiate between ulcerative colitis and Crohn’s disease?” answer=” Yes, you can differentiate by the history, radiological findings, and endoscopic biopsy.”?