HbA1c (Glycosylated Hemoglobin)
What sample is needed for HbA1c (Glycosylated Hemoglobin)?
- The blood sample is taken in the EDTA.
- Washed RBC or hemolysate is prepared stable for 4 to 7 days at 4 °C.
- A blood sample can be drawn at any time. No need for fasting or dietary needs.
What are the indications for HbA1c (Glycosylated Hemoglobin)?
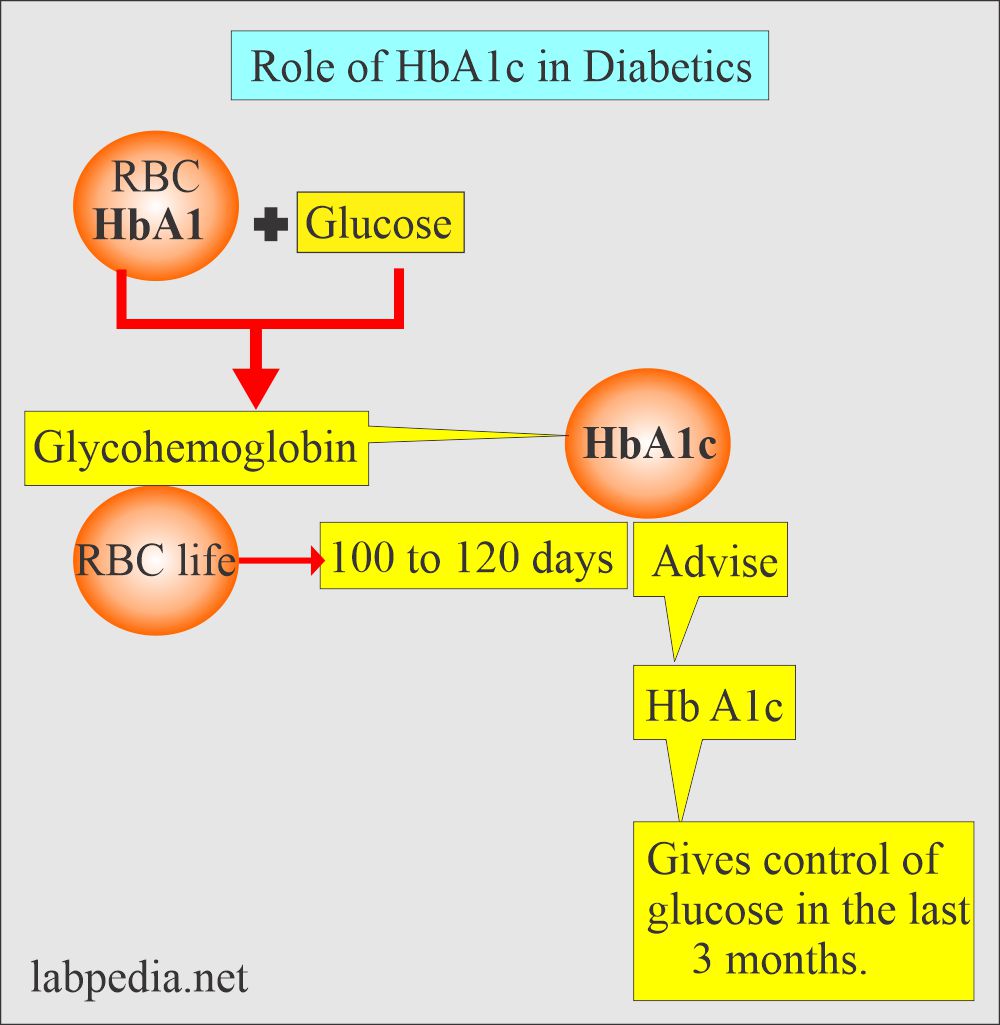
- This test is used to monitor diabetes control.
- This test shows the patient’s average glucose index over a long time (2 to 3 months).
- The index of diabetic control gives a direct relationship between poor control and the development of complications.
- It tracks glucose in the milder form of diabetes.
- It helps to determine which type of drugs may be needed.
- Predict the development and progression of diabetic microvascular complications.
- Its measurement is of value in a specific group of patients like:
- Diabetic children.
- Diabetic patients whose renal threshold for glucose is abnormal.
- Unstable diabetes type I, taking insulin.
- Type II diabetic women who become pregnant.
- Patients with changing dietary or other habits.
- It should be repeated every 3 to 4 months (some advise 2 to 3 months).
How will you define HbA1c (Glycosylated Hemoglobin)?
- Glucose combines with hemoglobin continuously and is nearly irreversible during the life span of RBCs (120 days).
- So, HbA1c will be proportional to the mean plasma glucose level during the previous 6 to 12 weeks.
- In adults, hemoglobin-A (Hb-A) constitutes 97% to 98% of normal hemoglobin. The remaining Hb-A2 is around 2.5%, and the Hb-F is 0.5%.
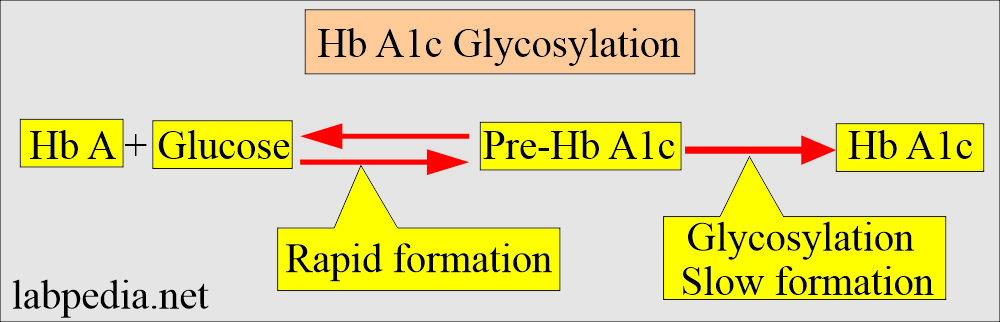
- Glucose combines with hemoglobin continuously and irreversibly during the life span of RBC (120 days), and this process is called glycosylation.
- In this process of glycosylation, hemoglobin is exposed to glucose. Initially, this bond is labile, but it later becomes stable. Once this bonding takes place, it becomes poorly irreversible.
- The HbA1c will be proportional to the mean blood glucose level during the last 6 to 12 weeks.
What are the advantages of HbA1c (Glycosylated Hemoglobin)?
- The sample can be drawn at any time.
- This test is not affected by short-term variations like:
- Food.
- Exercise.
- Hypoglycemic agents.
- Stress.
- Patient attitude or cooperation.
- It differentiates short-term hyperglycemia in nondiabetic patients like:
- Recent stress.
- Myocardial infarction.
- Gives information on glucose imbalance in a patient with mild diabetes mellitus.
- It may rise within one week after blood glucose rises due to stopping the therapy. It will not fall for 2 to 4 weeks after blood glucose decreases when treatment starts again.
- Evaluating the success of diabetic treatment and patient compliance.
What are the limitations of HbA1c (Glycosylated Hemoglobin)?
- This can not be used to find a day-to-day glucose fluctuation to adjust the insulin dose.
- It can not find a day-to-day presence of hypo or hyperglycemia.
Please discuss the pathophysiology of HbA1c (Glycosylated Hemoglobin)?
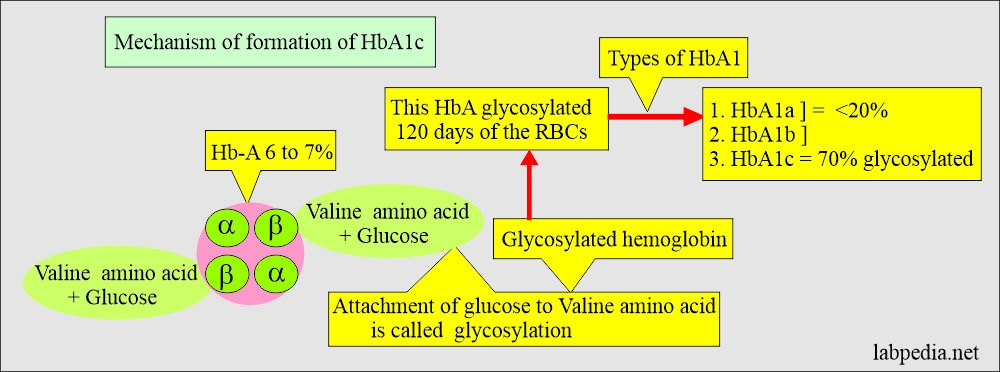
- In adults, hemoglobin is:
- Hemoglobin A is 98%.
- HbA2 is around 2.5%.
- HbF is 0.5%.
- Now, 7% of hemoglobin A consists of hemoglobin A1.
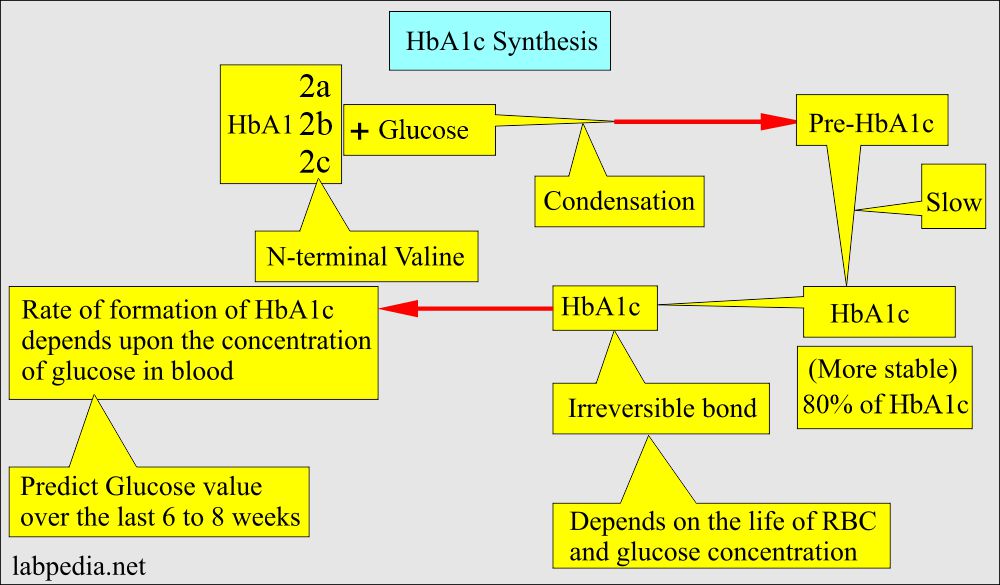
- Glucose is attached to the terminal valine amino acid of the globulin β-chain. This process is called glycosylation.
- This hemoglobin A1 combines strongly with glucose through glycosylation, called hemoglobin A1 (HbA1).
- The glycosylation process takes place when RBCs are exposed to glucose.
- Hemoglobin and glucose form a bond. Initially, it is labile; then, it becomes stable. It is very slowly and poorly reversible.
- Hemoglobin A1 consists of the following:
- HbA1a
- HbA1b
- HbA1c (This will combine more strongly with glucose).
- HbA1c combines more strongly with glucose.
- HbA1c is 70% glycosylated.
- While HbA1a and HbA1b are only 20% glycosylated.
- If we measure total HbA1, the values are 2% to 4% higher than the HbA1c.
- The amount of glycohemoglobin depends upon the glucose concentration available in the circulation and the life span of RBCs, which is 120 days.
- Therefore, glycohemoglobin estimates glucose over 100 to 120 days.
- Glycohemoglobin concentration depends upon the exposure of glucose to the RBCs.
- HbA1c may not reflect the recent change in glucose level.
- Glycohemoglobin is a normal, minor type of hemoglobin. This is blood glucose bound to hemoglobin.
- In the presence of hyperglycemia, an increase in glycohemoglobin causes an increase in the Hb A1c.
- When a measurable increase in the glycosylated or stable hemoglobin begins, it will appear in 2 to 3 weeks.
- Glycosylated hemoglobin reflects the average blood glucose level for 2- 3 months before the test.
- Glycated hemoglobin concentration reflects the mean blood glucose level concentration over the last 4 to 8 weeks.
What is the HbA1c positivity rate?:
| Blood glucose level | Positivity of HbA1c |
|
|
|
|
|
|
What is the Normal HbA1c?
Source 1
- HbA1 c (% of total Hb) = 4.0 to 5.2
- Hb A1 (% of total Hb) = 5.0 to 7.5
Source 2
- Non-Diabetic adults = 2.2 to 4.8 %.
- Non-Diabetic child = 1.8 to 4.0 %.
- Prediabetic = 5.7 to 6.4 %
- Diabetics = >6.5 %
- Diabetic HbA1c = > 8.1 % = corresponds with glucose >200 mg/dl.
What should be Diabetic control and HbA1c?
- Good diabetic control = 2.5 to 5.9 %.
- Fair diabetic control = 6 to 8 %.
- Poor diabetic control = > 8 %.
- (Values may vary according to the lab.)
- Another source
- Good diabetic control = <7%
- Fair diabetic control = 10%
- poor diabetic control = 13% to 20%
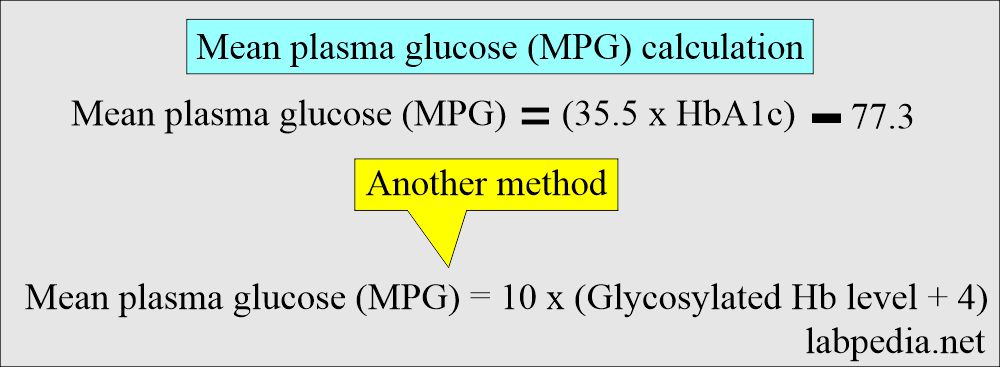
What is the mean Plasma glucose (MPG)?
- It is a mathematical calculation in which HbA1c (Glycosylated Hemoglobin and Glycated Hb) correlate with daily mean plasma glucose level (MPG).
-
- The formula is as follows :
What are the HbA1c and recommendations for the treatment of diabetic patients?
| HbA1c level | Glucose mg/dL | Glucose mmol/L | Interpretations/recommendations |
| 4 | 65 | 3.6 | Non-diabetic |
| 5 | 100 | 5.55 | Non-diabetic |
| 6 | 135 | 7.5 | Non-diabetic |
| 7 | 170 | 9.5 | ADA target |
| 8 | 205 | 11.5 | Treatment needed |
| 9 | 240 | 13.5 | Treatment needed |
| 10 | 275 | 15.5 | Treatment needed |
| 11 | 269 | 14.9 | Treatment needed |
| 12 | 298 | 16.5 | Treatment needed |
| 13 | 326 | 18.0 | Treatment needed |
| 14 | 355 | 19.7 | Treatment needed |
What is HbA1c, and what are the estimated blood glucose levels?
| HbA1c level | Glucose level mg/dL |
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
What is the Formula for the conversion of mg/dL to mmo/L?
= Glucose in mg/dL /18 = Glucose in mmol/L
Glucose in mmol/L x 18 = Glucose in mg/dL
What are the causes of increased HbA1c levels?
- Newly diagnosed diabetic patient.
- Uncontrolled diabetic patient.
- Nondiabetic hyperglycemia is seen in:
- Cushing’s syndrome.
- Acromegaly.
- Corticosteroids therapy.
- Pheochromocytoma.
- Acute stress.
- Glucagonoma.
- Patient with splenectomy.
- Alcohol toxicity.
- Iron deficiency anemia.
- Lead toxicity.
- Opiates toxicity.
- Chronic renal failure with or without hemodialysis.
- Salicylates treatment.
What are the causes of decreased HbA1c levels?
- Shortened RBC’s life span.
- Hemolytic anemia.
- Hemoglobinopathies.
- After a blood transfusion.
- Chronic blood loss.
- Vitamin C or E intake in excess.
- Pregnancy.
- Following a blood transfusion.
What are the causes of a false raised level of HbA1c?
- Renal failure.
- Raised level of triglycerides (hypertriglyceridemia).
- In Chronic Alcoholics.
How you can lower the HbA1c?
- Exercise.
- Diet control.
- Medication.
- Or a combination of these.
What is the significance of HbA1c in diabetic patients?
- The incidence of retinopathy increases in patients with an HbA1c level between 6.0 to 7.0%
- Fewer chances for retinopathy when the HbA1c level is <6.5%.
- HbA1c level in diabetic patients is recommended at <7.0%.
- HbA1c should be checked at least twice a year.
- It is suggested that HbA1c levels >6.5% favor diabetes mellitus.
How can Diabetes type 2 risk can be lowered?
- It can be lowered around 58% of the cases by:
- Reducing the weight of about 7% of your body weight.
- Exercise like brisk walking for 30 minutes, 5 days a week.
Questions and answers:
Question 1: Which glycosylated hemoglobin has more binding with the glucose?
Question 2: What is the recommendation of the HbA1c for diabetic patients?