Growth Hormone (GH)
What sample is needed for Growth Hormone (GH)?
- This test is done on serum (clotted blood 3 to 5 ml).
- A serum sample is preferred.
- Plasma (EDTA) has lower values with some methods.
- The patient should fast and rest for at least 30 minutes before taking the blood.
- It is stable for 8 hours at 2 to 8 °C.
- It can be kept for a more extended period at -20 °C.
What are the precautions for Growth Hormone (GH) estimation?
- Perform the test immediately because the half-life of GH is 20 to 25 minutes.
- Immediately refrigerate the serum.
- The patient should be fasting after midnight.
- The patient must fast and rest 30 minutes before the sample is taken because this may increase the level.
- Avoid stress and low blood glucose, and exercise during the sample collection.
- EDTA plasma gives lower values.
- Random measurement is not helpful because of episodic variation in the GH level.
- Drugs that may increase the level are Amphetamine, Estrogen, Dopamine, Insulin, Methyldopa, Levodopa, Histamine, and Nicotinic acid.
- Certain drugs that decrease GH levels are Phenothiazine and Corticosteroids.
What are the indications for Growth Hormone (GH)?
- Growth hormone (GH) is done to identify its deficiency in:
- Adults with short stature.
- Delayed sexual maturity.
- Or other growth abnormalities.
- To diagnose gigantism or acromegaly,
- This can be used to identify the pituitary hypofunction or hyperfunction.
How will you define Growth Hormone (GH) and its structure?
- Growth hormone (GH) is a peptide secreted by the pituitary gland’s acidophilic cells.
- Hypothalamus hormones:
- Growth hormone-releasing hormone (GHRH) stimulates Growth hormone (GH) release.
- Somatostatin inhibits the release of Growth hormone (GH).
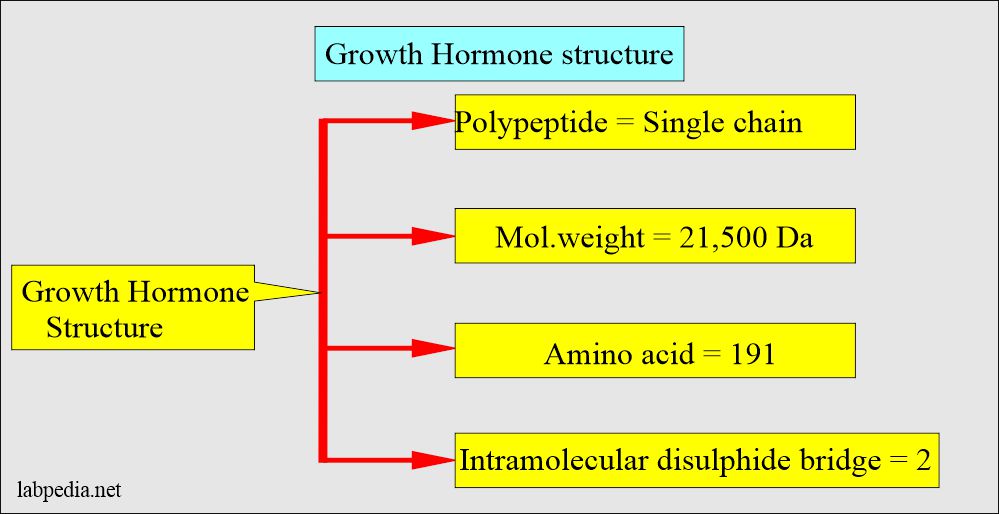
- The growth hormone is a single-chain polypeptide with a molecular weight of 21,500 Da and 191 amino acids.
- It has two intramolecular disulfide bridges.
- Its structure is similar to prolactin.
- This is one of the hormones involved in growth produced by the pituitary gland.
- Somatotropin is a man-made hormone.
- It is stored in the cells as intracellular granules.
- Growth hormone production is pulsatile.
How will you discuss the pathophysiology of growth hormone (GH)?
- Growth hormone (GH) plays a role in growth from birth until the end of puberty.
- GH promotes protein synthesis and stimulates skeletal growth.
- Various factors increase Growth hormone (GH) secretion.
- Growth hormone (GH) is produced by the anterior pituitary gland’s acidophilic cells and stored within the intracellular molecules granules.
- Growth hormone (GH) secretion occurs predominantly during sleep in irregular pulses or bursts.
How will be Growth Hormone secretion?
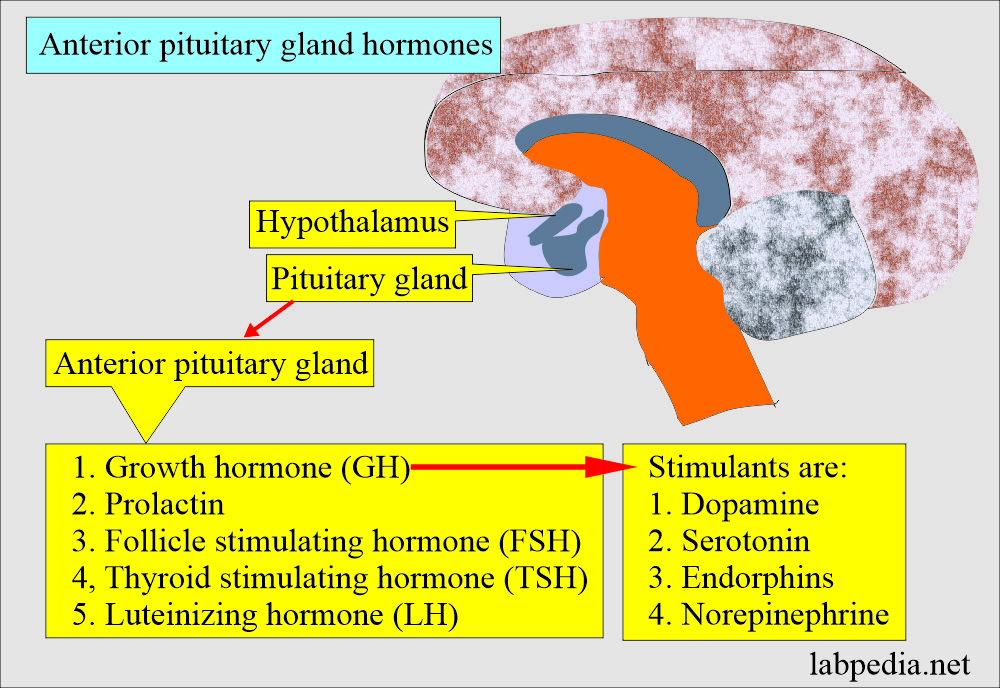
- Anterior pituitary gland cells (acidophilic cells) secrete:
- Growth hormone.
- Prolactin.
- Thyroid-stimulating hormone (TSH).
- Follicle-stimulating hormone (FSH).
- Luteinizing hormone (LH).
- Hypoglycemia stimulates the pituitary gland to secrete GH. It is an antagonist to insulin. This was used as a stimulation test but was not safe.
- Arginine is used to activate the secretion of GH.
- Growth hormone (GH) increases glucose by:
- Inhibiting the entry of glucose into the muscle cells.
- By inhibiting glycolysis.
- By inhibiting the formation of triglycerides from the glucose.
what is the Growth hormone (GH) controlling mechanism?
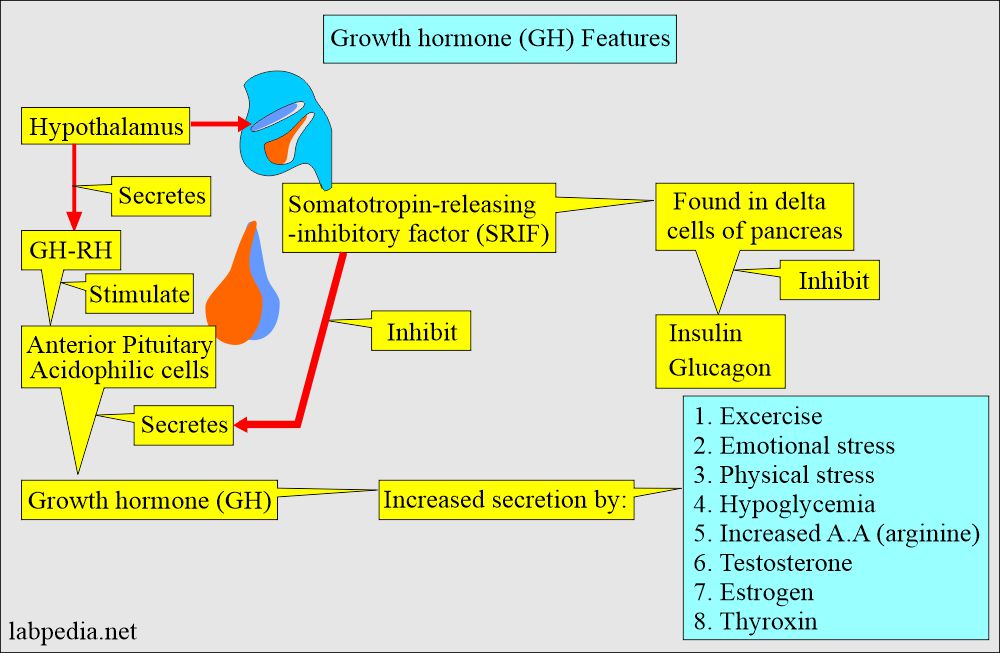
- Two hypothalamic factors secreted into portal circulation from nerve terminals in the median eminence control the growth hormone release.
- Growth hormone-releasing hormone (GH-RH). It will stimulate GH release into the circulation.
- Somatotropin release-inhibitory factor (SRIF) will inhibit the GH release into the circulation.
- SRIF is found in the pancreatic islets’ delta cells and other digestive tract sites.
- SRIF also has another important function: inhibiting insulin and glucagon release.
- Growth hormone (GH) affects many tissues through a group of peptides (Somatomedins).
- Increased level of Somatomedins leads to an increase in the production of Somatostatin, which is released from the hypothalamus.
What are the variations in Growth hormone (GH) production?
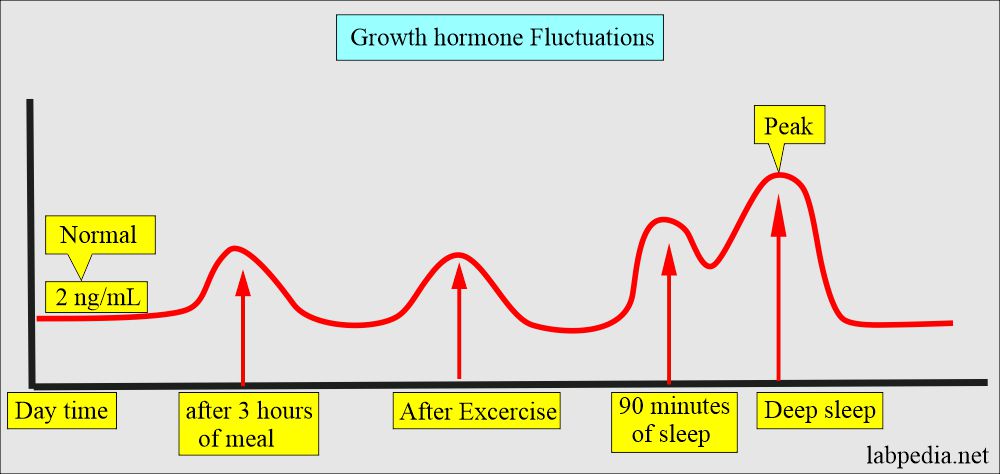
- GH has diurnal variation in concentration.
- Stimuli leading to increase of Growth hormone (GH):
- Exercise.
- Physical and emotional stress.
- Ingestion of protein.
- In hypoglycemia.
- Spike occurs after 3 hours of meals or exercise.
- The level is low during the day and is around 5 ng/mL (another reference says <2 ng/mL).
- For adults and children in the evening, it is the highest level.
- The secretion of GH is episodic and variable; sometimes, the level may reach 40 ng/ml in a healthy subject.
- The highest values are noted during the deepest sleep level. So its level is increased during sleep.
- So the best time is 60 to 90 minutes after deep sleep.
- Or do the exercise for 30 minutes and get the GH sample, which will be at the highest level.
- The GH may increase ten times the normal level during sleep.
- So the best time is 60 to 90 minutes after deep sleep.
- GH test may be used to monitor the acromegaly treatment.
- Obesity reduces the release of GH and insulin response.
- Hypoglycemia stimulates the pituitary to secret GH.
- The ability to secrete GH to conventional challenges decreases with age.
- GH is tested in case of retarded growth or short stature.
What are the stimuli for the growth hormone (GH) secretion?
| The stimulus for the secretion of Growth hormone (GH) | Time of peak level of Growth hormone (GH) |
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
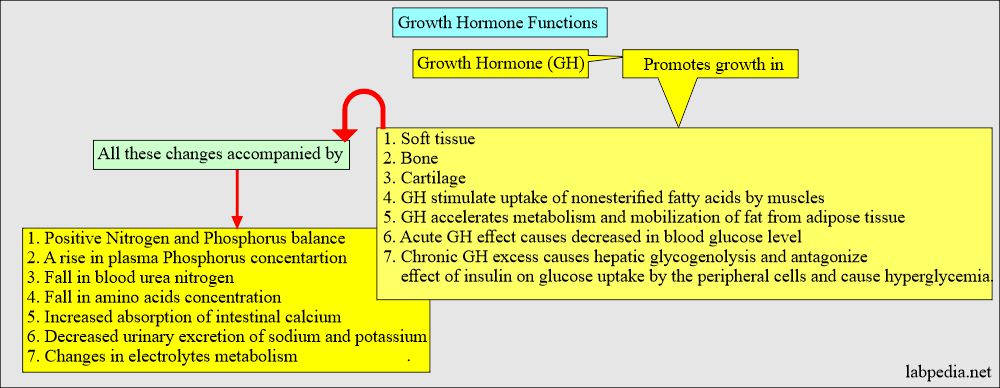
What are the functions of the growth hormone (GH)?
- GH insufficient amount leads to:
- Limited growth.
- Its deficiency leads to dwarfism.
- Delay in maturity.
- GH overproduction leads to :
- Its excess leads to gigantism.
- Acromegaly. (Increase in bone thickness and width).
- It promotes protein synthesis in muscles.
- It promotes the synthesis of protein in the liver.
- It stimulates skeletal muscle growth.
- It directly stimulates amino acid uptake.
- GH is important for anabolic and repair functions and proper skeletal growth.
- GH has an anti-insulin effect on carbohydrate metabolism.
- In fasting, insulin secretion decreases, and GH secretion increases, stimulating the body to use fatty acids instead of glucose.
What is the Clinical presentation of growth hormone (GH) excess?
- Excess GH is seen in the eosinophilic or chromophobe adenomas of the pituitary gland.
- 75% of these tumors can be diagnosed on CT scans or MRIs.
- Prolonged exposure to GH leads to overgrowth of the skeleton, muscles, and soft tissues.
- It is usually seen in adults and is called Acromegaly.
- This condition is called Pituitary gigantism, when excess GH is seen before long bone growth is complete.
What are the various types of growth hormone (GH) tests?
- A growth stimulation test can be done to evaluate the deficiency.
- An exercise stimulation test can be advised for GH.
- Brick exercise increases GH.
- This test can be done in the morning after an overnight fast or at any time.
- The patient is advised to exercise vigorously for 20 minutes.
- Collect the blood immediately after the termination of exercise.
- If GH is >7 ng/ml, it is less likely for deficiency.
- 3 to 6 ng/mL is an intermediate response, considered a suspected case.
- The growth suppression test is done in gigantism and acromegaly in adults.
- An oral glucose tolerance test is very helpful for increasing glucose levels. Normally, GH is suppressed. However, in acromegalic patients, there is a slight or no decrease in GH.
- Give 75 to 100 grams of glucose in 5 minutes, then get the sample for GH at 30, 60, 90, and 120 minutes.
- In an insulin-induced hypoglycemia stimulation test, hypoglycemia triggers the release of GH and ACTH from the pituitary glands in a normal person.
- Give I/V insulin in overnight fasting patients.
- Insulin 0.1 to 0.15 U/Kg body weight is injected I/V.
- Collect the blood sample after 30 30-minute rest period for GH, ACTH, and cortisol.
- Collect blood samples at 30, 60, and 90-minute intervals.
- Estimate glucose, GH, ACTH, and cortisol.
- The patients may become symptomatic and develop hypoglycemia <40 mg/dL.
- This test is contraindicated in patients with seizures and ischemic heart disease.
- GH level reaches a peak level of >10 ng/mL.
- Cortisol level reaches a peak value of >20 µg/dL.
- Direct Growth hormone (GH) can be measured by bioassay, receptor assay, and immunoassay.
Acromegaly:
How will you define acromegaly?
- Acromegaly is produced in adults by the growth hormone (GH) increase.
- the most common cause may be the eosinophilic adenoma of the pituitary gland.
- Roughly 2/3 of the patients are female.
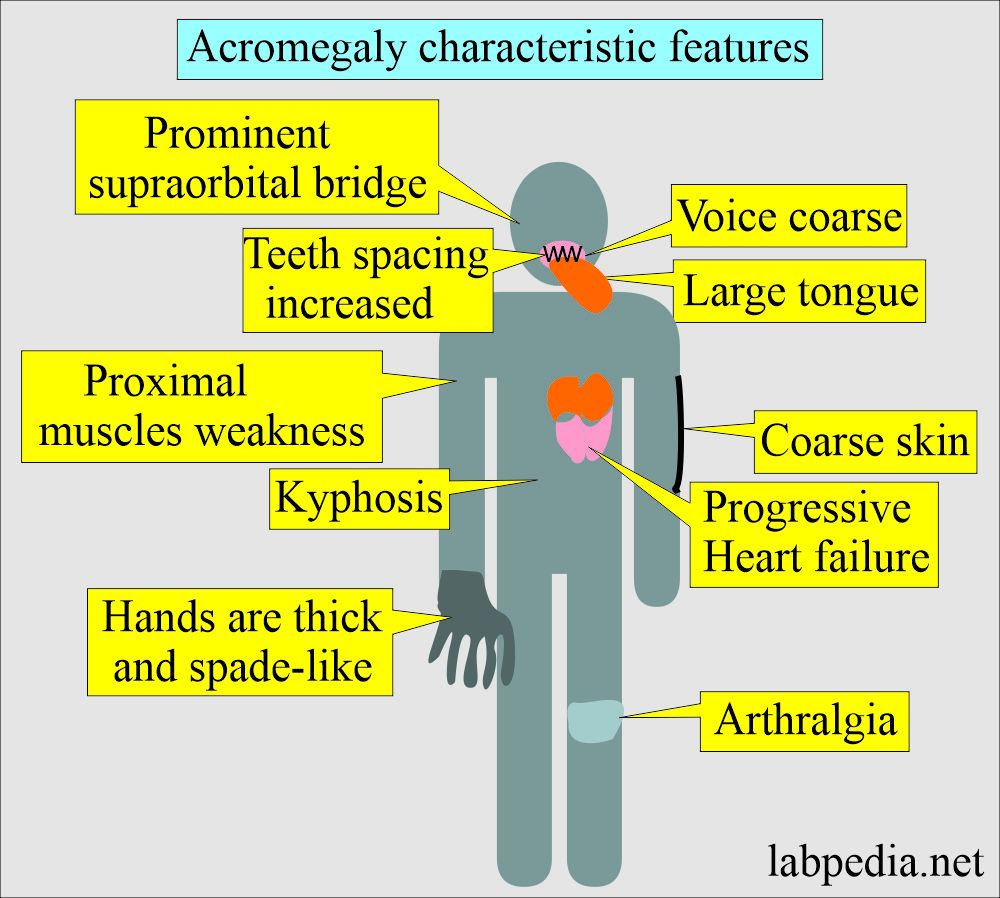
How will be the presentation of the acromegaly?
- The excess of GH leads to Acromegaly.
- Pituitary gigantism is seen before the long bone growth is complete.
- The physical appearance of the patient can diagnose this.
- There is an overgrowth of soft tissue and bone.
- There is coarse, oily skin.
- There is a large tongue.
- There are prominent supraorbital ridges.
- The teeth spacing is increased.
- Hands are thick, spade-like.
- The patient will have arthralgia and kyphosis.
- The voice is coarse.
- The patient may develop proximal muscle weakness.
- Sweating and headaches are common.
- The patient will have progressive heart failure.
- The reversibility of the physical changes depends upon the duration of the disease.
- Acromegaly may lead to severe disability or death due to cardiac or neurological complications.
- There is an abnormal response of GH to oral glucose administration.
- The normal person shows <1 ng/ mL of GH after an oral dose of glucose.
What are the Complications of Acromegaly?
- The patient may develop diabetes mellitus.
- The patient will have hypertension and cardiomegaly.
- There is obstructive sleep apnea.
How will you diagnose Acromegaly?
- Acromegaly diagnosis depends upon the increased level of Growth hormone (GH).
- Advise the glucose tolerance test and collect a blood sample at 0, 30, 60, and 90 minutes.
- Estimate both glucose and GH.
- The values will be suppressed at around <1.0 ng/mL.
- Another test is IGF-1 (insulin-like growth factor-1), whose concentration increases in acromegaly.
How will you treat the Acromegaly?
- Acromegaly due to adenoma is a transsphenoidal resection of the tumor.
- Another method is gamma knife multiport irradiation.
- Somatostatin (SST) long-acting needs only one dose per month.
What will be the presentation of deficiency of growth hormone?
- This is usually seen in hypothalamic and pituitary tumors.
- Growth is a dwarf and short-stature in the child.
How will you diagnose growth hormone (GH) deficiency?
- Advice: Two stimulating tests like insulin hypoglycemia or arginine.
- Measure GH at 30, 60, and 90 minutes.
- Normal patients show an increase of GH >8.0 ng/mL.
What is normal growth hormone (GH)?Source 1
| Age | ng/mL |
| Cord blood | 8 to 41 |
| Newborn | |
| One day | 5 to 53 |
| One week | 5 to 27 |
| Children 1 to 12 months | 2 to 10 |
| Adult | |
| Male | 0 to 4 |
| Female | 0 to 18 |
| > 60 years | |
| Male | 1 to 9 |
| Female | 1 to 16 |
- To convert into SI units x 1.0 = µg/L
Source 2
| Men | <5 ng/mL or <5 µg/L) |
| Women | <10 ng/mL or <10µg/L) |
| Newborn | 10 to 40 ng /ml |
| Child | 0 to 10 ng/ml |
- The random level of GH provides little diagnostic information.
- The single estimation may not be helpful because of the variation in the level of GH during the day.
What are the causes of increased Growth hormone (GH)?
- Pituitary gigantism (Acromegaly = up to 400 ng/ml).
- Ectopic GH secretion, e.g., Stomach neoplasm, lung.
- Renal failure.
- Cirrhosis.
- Stress, exercise, prolonged fasting.
- Uncontrolled diabetes mellitus.
- Anorexia nervosa.
- Starvation and malnutrition.
- Hypoglycemia.
- Major surgery.
- Exercise.
What are the causes of decreased growth hormone (GH)?
- Pituitary dwarfism, hypopituitarism.
- Adrenocortical hyperfunction.
- Hyperglycemia.
- Delayed sexual maturity.
- Growth hormone deficiency.
Questions and answers:
Question 1: When is the peak level of GH?
Question 2: What are the complications of acromegaly?