Gilbert’s Syndrome, Signs/Symptoms and Diagnosis
Gilbert’s Syndrome
What Sample is needed for Gilbert’s Syndrome?
- The patient’s serum is needed.
- A random sample can be taken.
What are the precautions for Gilbert’s Syndrome?
- Avoid samples from the light.
How will you define Gilbert’s Syndrome?
- Gilbert’s syndrome is benign, intermittent, familial (autosomal dominant), non-hemolytic unconjugated hyperbilirubinemia.
- Jaundice is usually accelerated by pregnancy, exercise, fever, and drugs.
- Alcohol and contraceptive pills may increase unconjugated bilirubin.
- It is rarely identified before puberty
- This syndrome is characterized by mild unconjugated hyperbilirubinemia.
- Nearly all unconjugated bilirubin is detected.
- This is a benign, harmless condition because there is a mild increase in the unconjugated bilirubin.
- It is chronic, benign, intermittent, familial (autosomal dominant), non-hemolytic, unconjugated hyperbilirubinemia, usually diagnosed on routine laboratory investigations.
- Gilbert’s disease is also called Constitutional Hepatic dysfunction or familial nonhemolytic jaundice.
- Gilbert’s syndrome is benign, intermittent, familial, autosomal dominant, with non-hemolytic jaundice (unconjugated hyperbilirubinemia), usually discovered on routine laboratory tests.
- This may affect 3% to 5% of the population.
Discuss pathophysiology of Gilbert’s Syndrome?
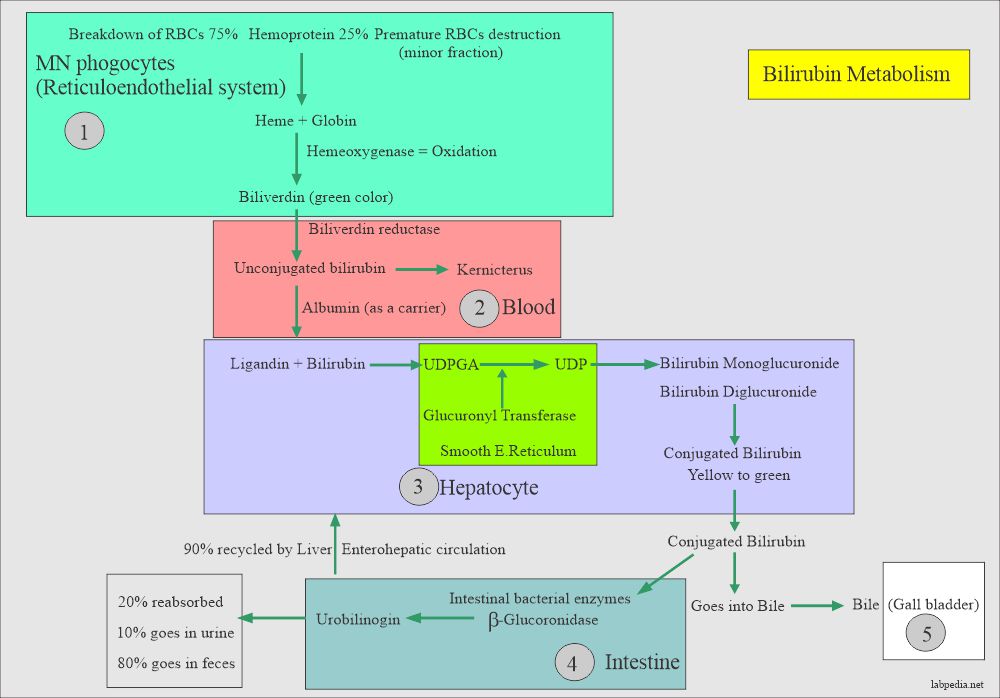
- To understand Gilbert’s syndrome, the following diagram of bilirubin metabolism explains the situation in Gilbert’s syndrome.
- Hemolysis of the RBCs gives rise to unconjugated bilirubin.
- Unconjugated bilirubin is carried by the carrier protein (albumin) to the liver.
- In the liver, conjugation takes place with the help of a glucoronyl tranferase enzyme.
- In Gilbert’s syndrome, the glucoronyl transferase enzyme is deficient.
What is the Mechanism of Gilbert’s syndrome?
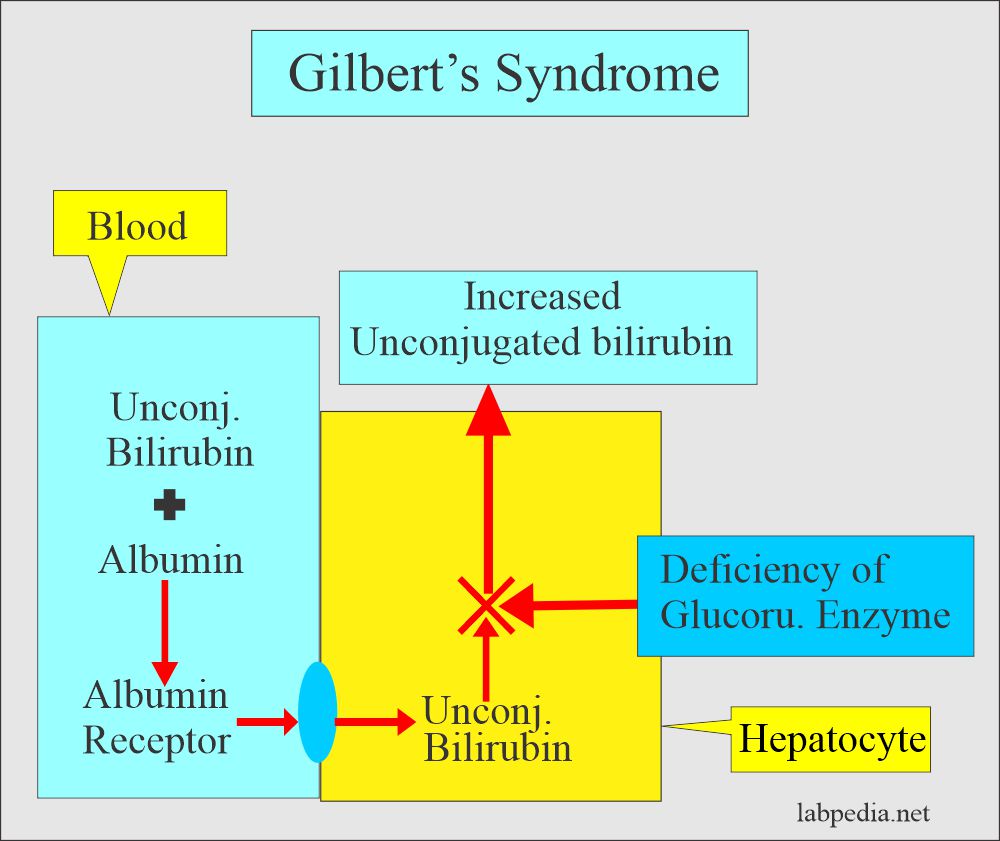
- Gilbert’s syndrome is a common, mild liver condition in which the liver doesn’t properly process bilirubin.
- Gilbert’s syndrome is a nonhemolytic condition and is an autosomal dominant character.
- Liver glucuronyltransferase activity is low due to a mutation in the bilirubin-UDP-glucuronosyl-transferase gene.
- It is a heterozygous group with raised bilirubin.
- It is inherited in an autosomal recessive pattern.
- There is an increase in unconjugated bilirubin, usually <3 mg/dL.
- Bilirubin fluctuates between 1.5 to 3 mg/dL.
- Bilirubin will increase with fasting.
- It is a benign condition and occurs in 2% of the population.
- The breakdown of red blood cells produces bilirubin.
- Hyperbilirubinemia is due to the reduced activity of the Glucuronyltransferase enzyme.
- There is no role in hemolysis, and hyperbilirubinemia is due to the deficiency of the enzyme.
- Glucuronyl transferase enzymes typically have 10% to 35% reduced activity.
- Glucuronyl Transferase enzyme is needed for the conjugation of the bilirubin.
- There is an increase in the bilirubin monoglucuronide (unconjugated bilirubin).
- Conjugation renders the bilirubin water-soluble excreted into the bile and duodenum.
- These patients are given phenobarbital, which normalizes bilirubin and hepatic bilirubin clearance.
What are the Signs and symptoms of Gilbert’s syndrome?
- Males are affected 1.5 to 7.3 times more than females.
- It is also seen in the siblings of Gilbert’s syndrome patients.
- Most patients are asymptomatic.
- The onset is shortly after birth but may be unnoticed for many years.
- There may be yellowness in the eyes and the skin in some cases.
- The most common finding is the presence of jaundice due to raised total bilirubin. This bilirubin is usually <3 mg/dL.
- The bilirubin level fluctuates and even sometimes may be normal. When these patients are followed, then 25% may show normal values.
- There is a transient slight increase in the bilirubin (unconjugated); previously, they had normal bilirubin (in <30% of the cases).
- It may rise to 18 mg/dL but usually is <4 mg/dL.
- Fasting will increase the unconjugated bilirubin.
- Bilirubin becomes normal after the normal diet in 12 to 24 hours.
- There may be fatigue.
- Jaundice may increase by the following:
- Stress.
- Fatigue.
- Intercurrent illness.
- Reduced caloric intake.
- Alcohol use.
- Rigorous exercise.
- Lake of sleep.
- Pregnancy.
- Fever.
- Various drugs.
- Alcohol intake.
- Birth control pills.
- These cases are usually diagnosed near puberty or in adult life during routine examinations.
Give Gilbert’s syndrome summary?
| Clinical parameters | Interpretations |
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
How will you Diagnose Gilbert’s syndrome?
- Exclude all other liver diseases.
- Liver functions are usually normal.
- There is no satisfactory specific test for the diagnosis of Gilbert’s syndrome.
- It may be followed for 12 to 18 months with a follow-up of liver function tests.
- Gilbert’s syndrome is confirmed if there are no constitutional symptoms or abnormal liver function tests except raised total bilirubin, which is mainly unconjugated.
- Exclusion of other diseases.
- Caloric deprivation test: If the patient’s diet is restricted to 400 calories/day, it will raise the total bilirubin level>0.8 mg/dl, suggesting Gilbert’s syndrome. Non-Gilbert’s syndrome patients will have less than this (<0.5 mg/dL).
- Bilirubin levels return to normal 12 to 14 hours after a normal diet.
- Indirect serum bilirubin is increased (Indirect bilirubin is seen in around 85% of the cases). It is usually less than 4 mg/100 ml.
- Rarely, it may increase to 18 mg/100 ml, and then it needs treatment.
- Fecal urobilinogen is decreased but maybe even normal.
- Urine shows no increased bilirubin.
- The liver function test is usually normal.
- Albumin is normal.
- Prothrombin time is normal.
- The liver biopsy is normal. It does not show any significant changes.
What is the Importance of the diagnosis of Gilbert’s syndrome?
- Some people misdiagnose this condition as chronic hepatitis.
- The absence of anemia and bilirubin in the urine differentiates this.
- Liver function tests are normal.
How will you treat Gilbert’s syndrome?
- These patients do not need treatment until bilirubin is high because the bilirubin is mostly very low.
- Give reassurance to the patient that he does not suffer from liver disease.
- Avoid acetaminophen because it is metabolized by glucuronidation. This gives rise to a toxic reaction.
Give List of Defective hepatic unconjugated bilirubin clearance due to defective uptake or conjugation?
- Gilbert’s syndrome.
- Crigler-Najjar type 1 and type II.
- Liver diseases (severe).
- Congestive heart failure.
- Drug-induced inhibition.
- Sometimes hyperthyroidism.
- Portacaval shunt.
How will you describe different types of inherited jaundice?
| Clinical parameters | Unconjugated Hyperbilirubinemia | Conjugated Hyperbilirubinemia | |||
| Gilbert’s disease | Type 1 Criggler-Najjar | Type II Criggler-Najjar syndrome | Rotor’s syndrome | Dubon-Jhonson syndrome | |
| Inherited mode | Autosomal dominant | Autosomal recessive | Autosomal dominant | Autosomal recessive | Autosomal recessive |
| Incidence | <7% of the population | Very rare | Uncommon | Rare | Uncommon |
| Age at onset | In adolescence | In infancy |
|
Early adulthood |
|
| Pathogenesis | Glucoronyl transferase enzyme deficiency (GTE) | GTE decreased | Marked decrease | Impaired conj. bilirubin excretion | Impaired cong. bilirubin excretion |
| Bilirubin level |
|
Mainly indirect | Mainly indirect |
|
|
| Clinical signs/symptoms |
|
|
|
Asymptomatic jaundice in young adults | Asymptomatic jaundice |
| Effect of phenobarbitone | Decreased to normal | There is no effect | Marked decrease | —– | —– |
| BSP (Dye excretion) test | May be mildly impaired in <40% of cases | It is absent | _____ | Positive, Initial rapid fall and then rise in 40 to 90 minutes | Positive, Slow clearance and no rise |
| Oral cholecyctography | Normal | Normal | Normal | Normal | GB usually not visualized |
| Liver biopsy | Normal | —- | —- | No pigments | Characteristic pigments |
| Treatment | Not needed | There is no treatment | Not needed | ||
Possible References Used
Questions and answers:
Question 1: What is the mechanism of Gilbert's syndrome?
Question 2: How will you treat the patients with Gilbert's syndrome?

Take care you have mentioned in mechanism of action of gilbert unconj. bilirubin would increase in fasting. But in the column that differ types you mentioned it would decrease by fasting.
Thanks for your concern. Actually, I mean that bilirubin will not go above 3 mg/dL.