Fibrinogen (Factor 1), Afibrinogenemia, Dysfibrogenemia
Fibrinogen (Factor 1)
What Sample for Fibrinogen (Factor 1) is needed?
- The blood is collected in a 0.2 ml ESR solution and 1.8 ml blood.
- Or citrated plasma can be used. Stable for several months at -20 °C.
- Citrate 4 mg/mL is used.
- Don’t use heparin.
- Don’t collect blood in the glass tubes.
What are the Indications for Fibrinogen (Factor 1)?
- It is part of the coagulation panel.
- This is done for prolonged bleeding.
- This is done to investigate abnormal PT, APTT, or bleeding disorders.
- As a follow-up of a bleeding disorder.
- This is done to diagnose DIC.
What are the precautions for Fibrinogen (Factor 1)?
- Blood transfusion in the last month may affect the test result.
- A diet rich in omega-3 and omega-6 fatty acids will reduce the level of fibrinogen.
- Estrogen and oral contraceptives will increase the level.
- Anabolic steroids, androgens, phenobarbiturates, streptokinase, and valproic acid decrease the level.
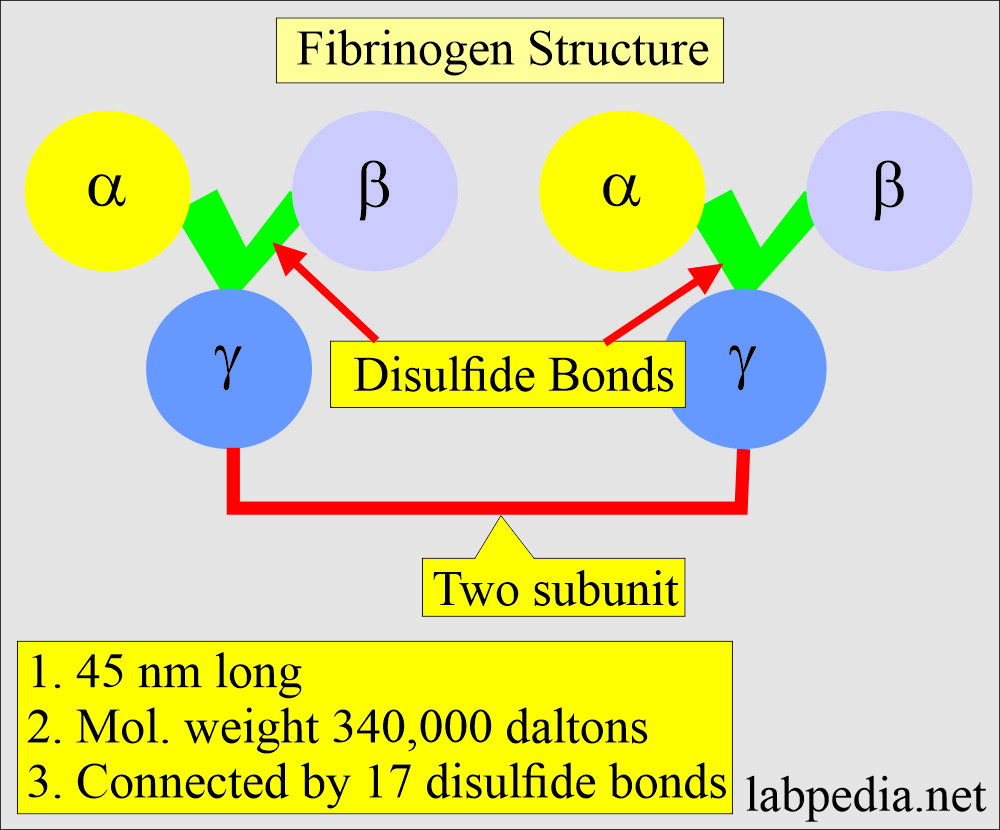
What is the structure of Fibrinogen (Factor 1)?
- Fibrinogen is a complex glycoprotein (Polypeptide) produced in the liver that, through enzyme action, is converted to fibrin.
- The molecular weight is 340,000 daltons.
- Fibrinogen consists of two identical subunits containing three dissimilar polypeptide chains:
- 2 = Aα
- 2 = Bβ
- 2 = γ
- Connected by a disulfide bond (17 pairs of disulfide bonds).
- It is 45 nm long, containing two outer D-domains, each connected to the central E domain by a coiled-coil segment.
- Fibrinogen is plasma soluble and is converted into fibrin.
- It has a half-life of three days.
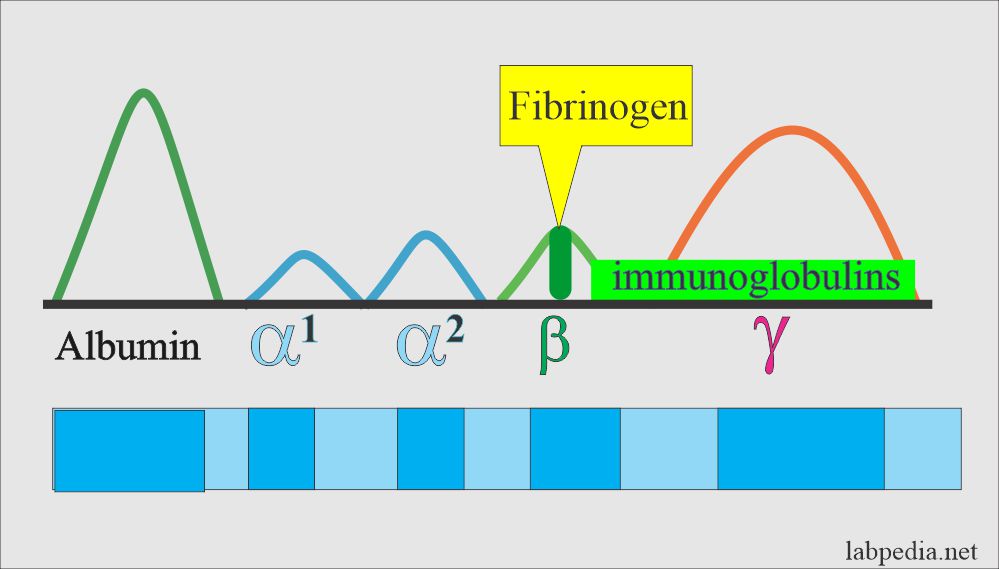
- On electrophoresis, it is present in the β- globulin fraction.
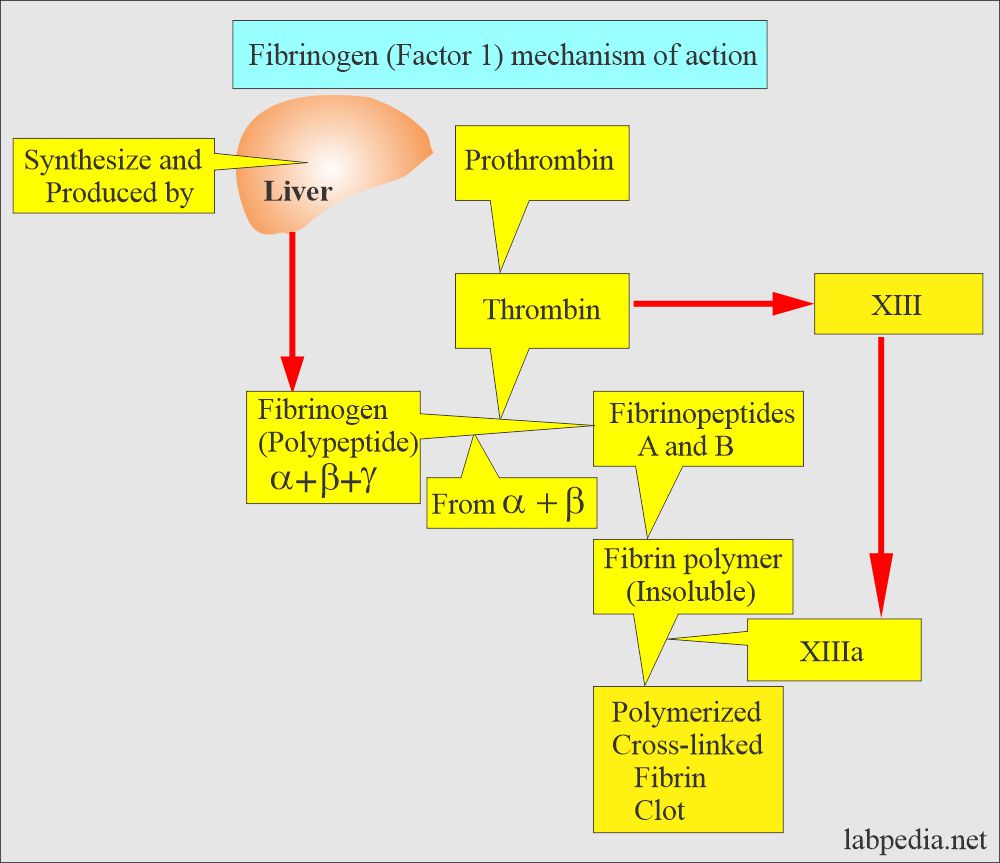
What is the role of fibrinogen (Factor 1) in the clotting mechanism?
- The fibrin with platelets forms the clot.
- Fibrinogen is essential for the clotting mechanism.
- Basically, this will occlude the blood vessel and stop the bleeding.
- Fibrin trapped the platelet aggregates at the site of vascular injury.
- Then fibrin converts unstable platelets plug to firm, stable hemostatic plugs.
- Fibrin binds to the thrombin and reduces its activity.
- This is part of a common pathway in clotting.
- Thrombin converts fibrinogen into fibrin.
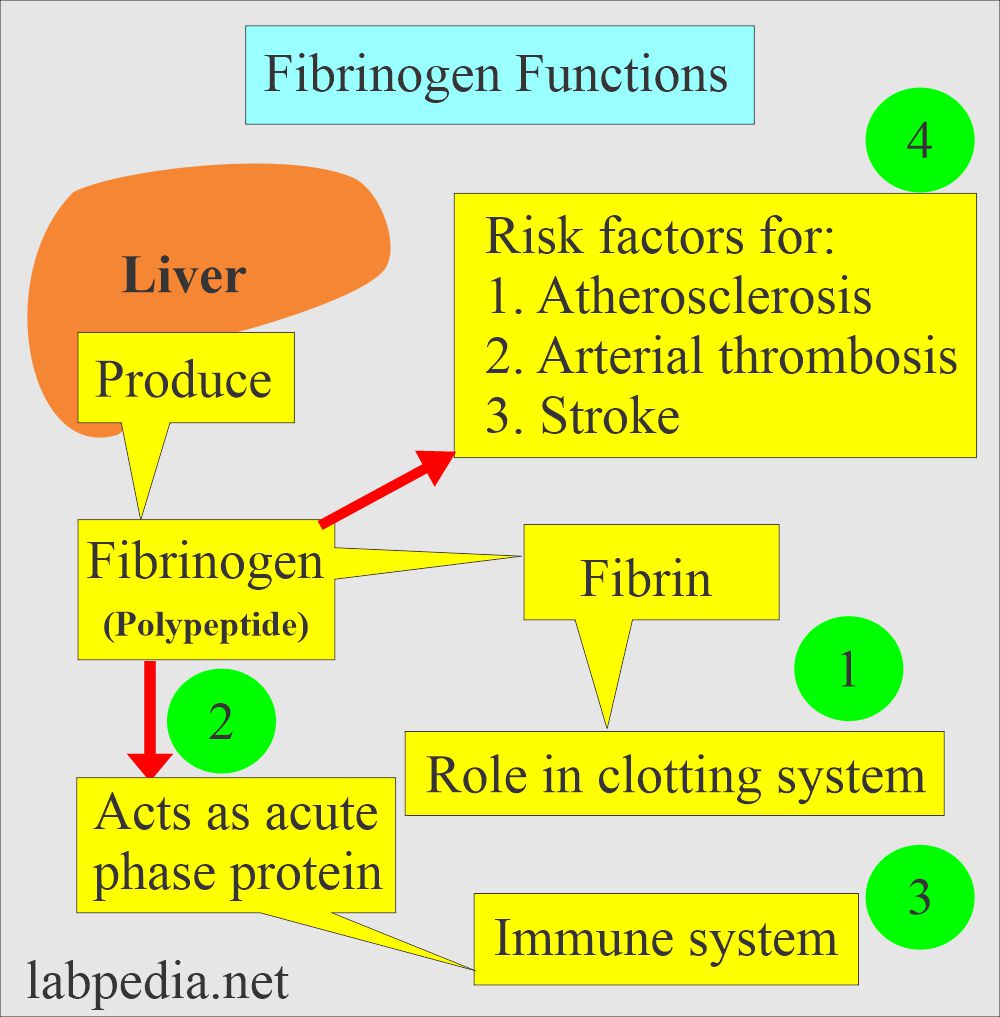
Fibrinogen (Factor 1) functions?
- The liver produces fibrinogen, and it acts as an acute-phase protein.
- Increased level of fibrinogen is a risk factor for:
- Atherosclerosis.
- Arterial thrombosis.
- Coronary heart disease.
- Myocardial infarction.
- Peripheral arterial disease.
- Stroke.
- Fibrinogen has a role in the immune system.
- Fibrinogen has the main role in the blood clotting system.
What is the normal Fibrinogen level?
Source 1
- Newborn = 125 to 300 mg/dL
- Adult = 200 to 400 mg/dL
- To convert to SI unit x 0.01 = g/L
Source 2
- Adult = 200 to 400 mg/dl or 2 to 4 G/L
- Newborn = 125 to 300 mg/dl.
- The critical value is = < 100 mg/dL (may cause spontaneous bleeding).
What are the conditions where there is an Increased fibrinogen (Factor 1) level?
- Inflammation and infections ( Rheumatoid arthritis, pneumonia, tuberculosis).
- Acute myocardial infarction.
- Coronary heart disease.
- Nephrotic syndrome.
- Cancer, Multiple Myeloma, and Hodgkin’s disease.
- Pregnancy and Eclampsia.
- Cigarette smoking.
- In the case of a stroke.
- In cigarette smoking.
- In pregnancy.
- Trauma.
What are the conditions where there is a Decreased Fibrinogen (Factor 1) level?
- Liver diseases like hepatitis and cirrhosis.
- DIC (secondary fibrinolysis).
- Cancers.
- Dysfibrinogenemia
- Primary fibrinolysis.
- Malnutrition.
- Blood transfusion: if a large volume is given, it may dilute the fibrinogen level.
- Fibrinolysins.
- Advanced carcinomas.
How will you define Afibrinogenemia?
- This is rare and usually inherited as an autosomal recessive trait.
- If the parents do not show the disease, they can still have affected children.
- When 2 carriers of autosomal recessive positive parents have children, each child has a:
- 25% chance to be affected.
- 50% chance to be an unaffected carrier.
- 25% chance to be unaffected and not a carrier.
- There is a severe lake of fibrinogen, and blood will not clot.
- What are the Signs and symptoms of afibrinogenemia?
- In the case of afibrinogenemia, if the fibrinogen level is <0.1 g/L (<60 mg/dL), it will have bleeding abnormality from mild to severe.
- This disease is present from birth.
- The first symptom is bleeding from the umbilical cord, which will not stop and is difficult to stop.
- There may be gastrointestinal bleeding.
- There may be nose bleeding (epistaxis) or bleeding from the oral mucosa.
- There may be bleeding episodes, bruises, and poor wound healing.
- Females may have excessive menstruation.
- There may be spontaneous abortion.
- There may be CNS hemorrhage.
- Evidence of bleeding in the joints.
How will you diagnose afibrinogenemia?
- The following tests are advised:
- Prothrombin time (PT).
- Activated partial thromboplastin time (APTT).
- Fibrinogen level in the blood.
- Reptilase time.
- Thrombin time.
- Prolonged bleeding time (BT) and fibrinogen level <0.1 g/L (<60 mg/dL), indicating afibrinogenemia.
- Diagnostic values are:
- Plasma fibrinogen is absent.
- BT is increased in 1/3 of the cases.
- PT, APTT, and TT are abnormal.
How will you define Dysfibrinogenemia?
- There is an abnormal fibrinogen due to a structural abnormality, which results in an abnormal function. This change is in amino acids or carbohydrate composition.
- This may be:
- Congenital or Inherited: There is an increased risk of bleeding, thrombosis, or both in the same patient or family.
- Some of the patients are asymptomatic.
- The prognosis is good. The event of thrombosis and bleeding is mild.
- Acquired: Where the fibrinogen is dysfunctional due to autoimmune diseases or liver diseases, plasma cell dyscrasia, or cancers.
- There is more bleeding than thrombosis.
- The prognosis is worse because of liver disease.
- Congenital or Inherited: There is an increased risk of bleeding, thrombosis, or both in the same patient or family.
- This leads to relatively mild hemorrhage in the case of congenital cause.
- Few of these may tend to thrombosis in case of acquired cause.
- >50% of the cases have no bleeding episodes.
- 29% to 25% of the cases have mild to moderate bleeding or thrombosis, or both.
How will you Diagnose Dysfibrogenemia?
- Prothrombin time (PT) is prolonged.
- Activated partial thromboplastin (APTT) is also prolonged.
- Thrombin time (TT) is the most sensitive test for dysfibrinogenemia in the case of bleeding tendency.
- TT may not be prolonged in the case of a tendency for thrombosis.
- Fibrin formation is abnormally slow, with prolonged TT and reptilase time,
- Reptilase time is prolonged.
How will you differentiate different types of fibrinogens?
| Laboratory test | Hypofibrinogenemia | Afibrinogenemia | Dysfibrogenemia |
| Fibrinogen level | Decreased | Not detectable | Normal/Abnormal form |
| Fibrinogen immunoassay | Abnormal | Absent | Normal |
| Platelets aggregation | Normal | Abnormal | Normal |
| Prothrombin time (PT) | Prolonged | Prolonged | Prolonged/Normal |
| Bleeding time (BT) | Normal | Prolonged | Normal |
| APTT | Prolonged | Prolonged | Prolonged/Normal |
| Thrombin time (TT) | Prolonged | Prolonged | Prolonged |
| Reptilase time | Prolonged | Prolonged | Prolonged |
- The critical value of Fibrinogen (Factor 1) = <60 mg/dL.
Value for the layman:
- This is advised when there is a history of bleeding or bruises.
- If the patient has epistaxis.