Ferritin (serum Ferritin Level)
Ferritin (Serum Ferritin Level)
What Sample is needed for Ferritin?
- This test is performed on a serum that remains stable for 7 days at 2 to 8 °C.
- This can be stored at -20 °C for 6 months.
What are the Precautions for Ferritin?
- Avoid vigorous mixing, which can denature ferritin.
- Avoid freezing and thawing of the sample.
- In screening tests for early detection of iron overload, ferritin is not a better indicator than measurement of serum iron, TIBC, and transferrin saturation.
- After the meal, iron will increase ferritin levels. This is because iron stimulates ferritin production, increasing iron storage.
- Radioimmuno-substances increased the value when using RIA.
- Gaucher’s disease, both acute and chronic, causes a false rise in ferritin levels.
- Drugs containing iron will increase the ferritin level. There is increased ferritin to store the iron.
What are the Indications for Ferritin?
- This is the most sensitive test for diagnosing iron-deficiency anemia.
- This test is recommended to assess iron stores in the body.
- Advised to see the response to iron therapy.
- It differs from iron-deficiency anemia and anemia of chronic disease.
- It monitors the iron status in patients with chronic renal diseases with or without dialysis.
How will you define Ferritin?
- Ferritin is the major body iron storage compound (chief iron-storage protein).
- Bone marrow, tissue, and hemosiderin stain iron, but ferritin will not take a stain.
- A serum ferritin level decreases, accompanied by a decrease in tissue ferritin; this will correlate with an iron decrease in iron deficiency anemia.
- Ferritin is the most sensitive test for iron deficiency anemia.
Iron metabolism
How will you discuss the Pathophysiology Of Iron metabolism?
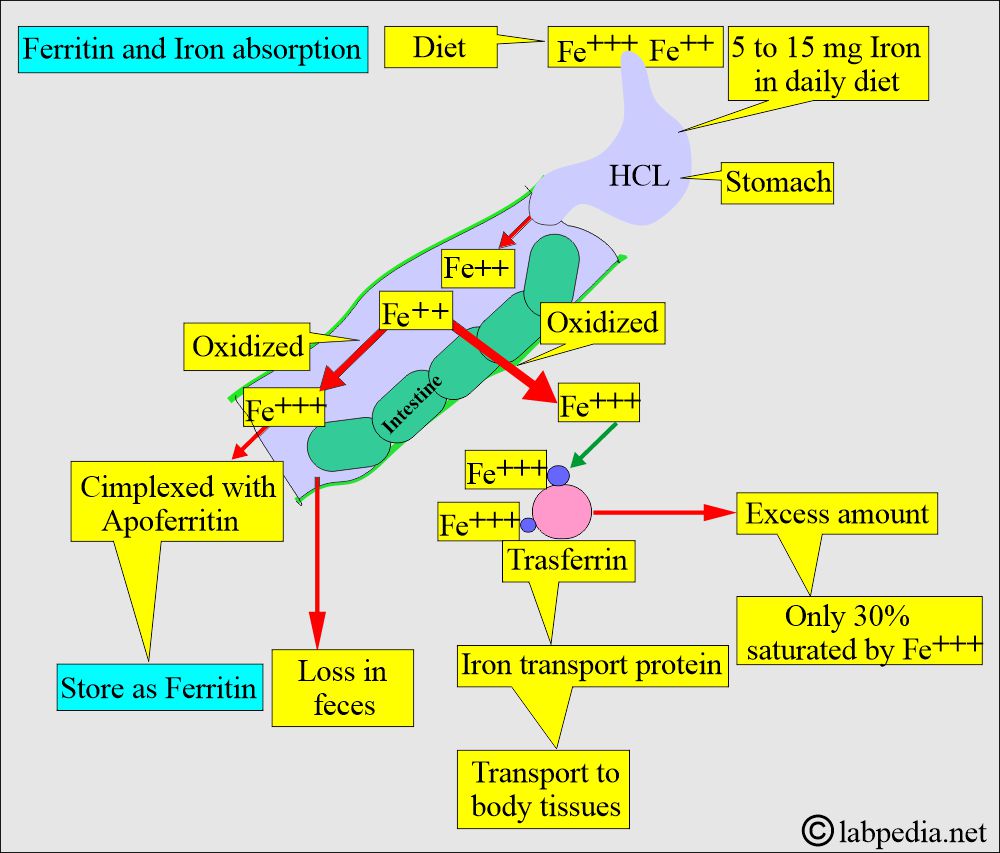
- Iron in the diet is absorbed (5% to 10%) by the intestinal epithelial cells (mainly the duodenum and upper jejunum). Then it enters the bloodstream and is used by RBCs in the bone marrow.
- The minimum daily iron requirement for non-pregnant women is 1 mg.
- Pregnant and lactating women need more than 1 mg of iron per day.
- During the 2nd and 3rd trimesters, the daily iron requirement is 5 to 6 mg.
- 1000 calories of the diet contain 6 mg of iron.
- 2500 calories consumed by an adult will provide 15 mg of iron/day from the diet.
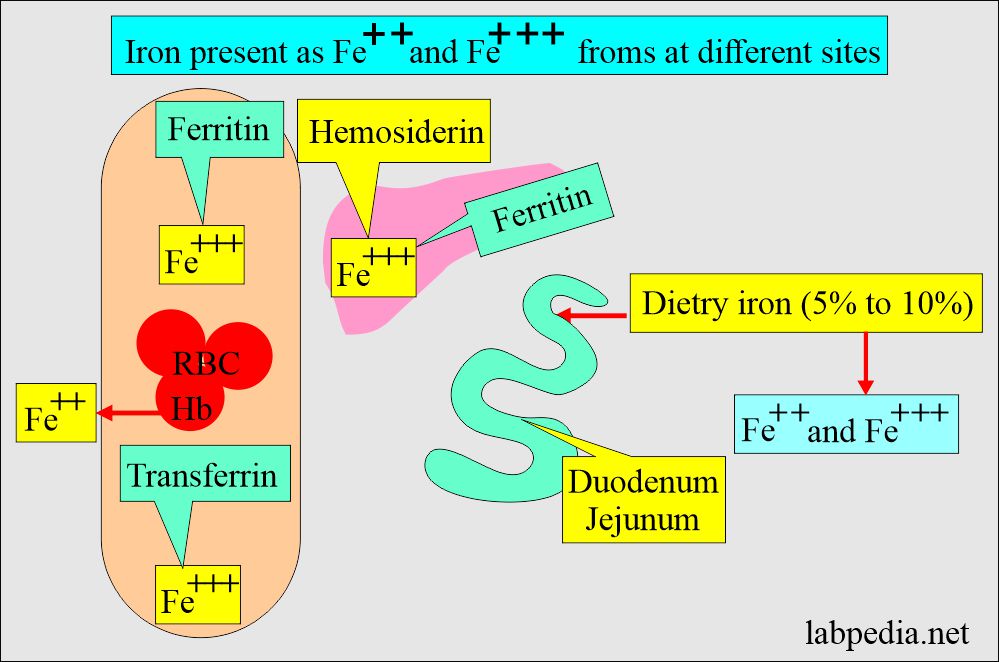
What types of Iron exist in the blood and tissue?
- Dietary iron is in ferrous (Fe2+) and ferric (Fe3+) forms.
- In Hemoglobin, it is in the Fe2++ form.
- Transferrin has a ferric (Fe3+) form and is present in the serum.
- Ferritin exists in a ferric (Fe3+) form and is present in serum and tissues.
- Hemosiderin is in the ferric (Fe3+) form and is present in bone marrow and tissue.
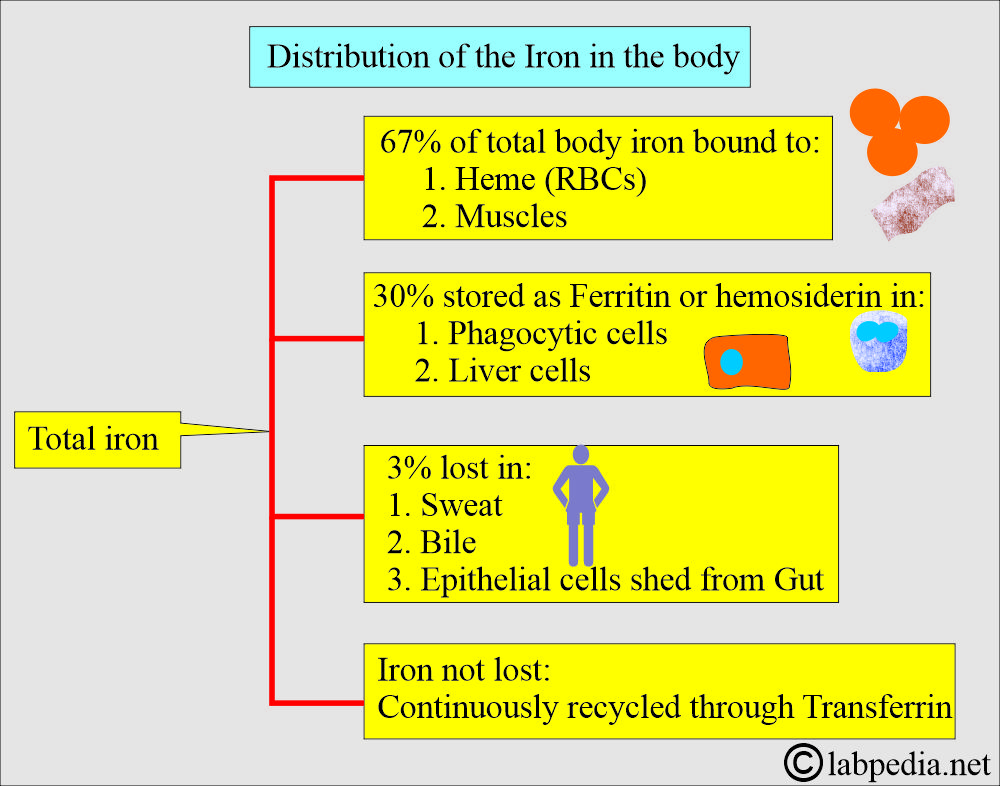
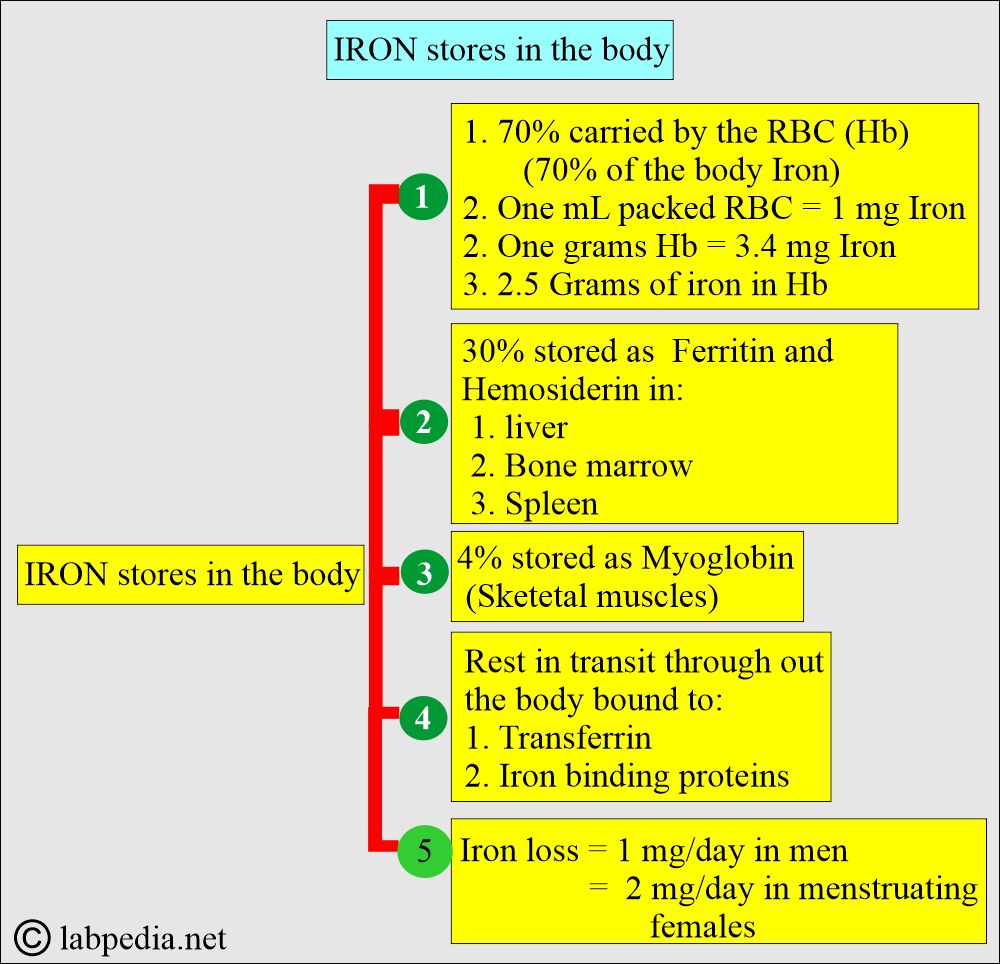
How is the Total iron distribution in the body?
- Iron in the body is distributed in various forms. 67% of the total body is present in the heme of RBCs, and some amount in muscles.
- 30% of iron is stored as ferritin or hemosiderin in the phagocytic and liver cells.
- The remaining 3% is lost in the urine, sweat, feces, bile, and gut.
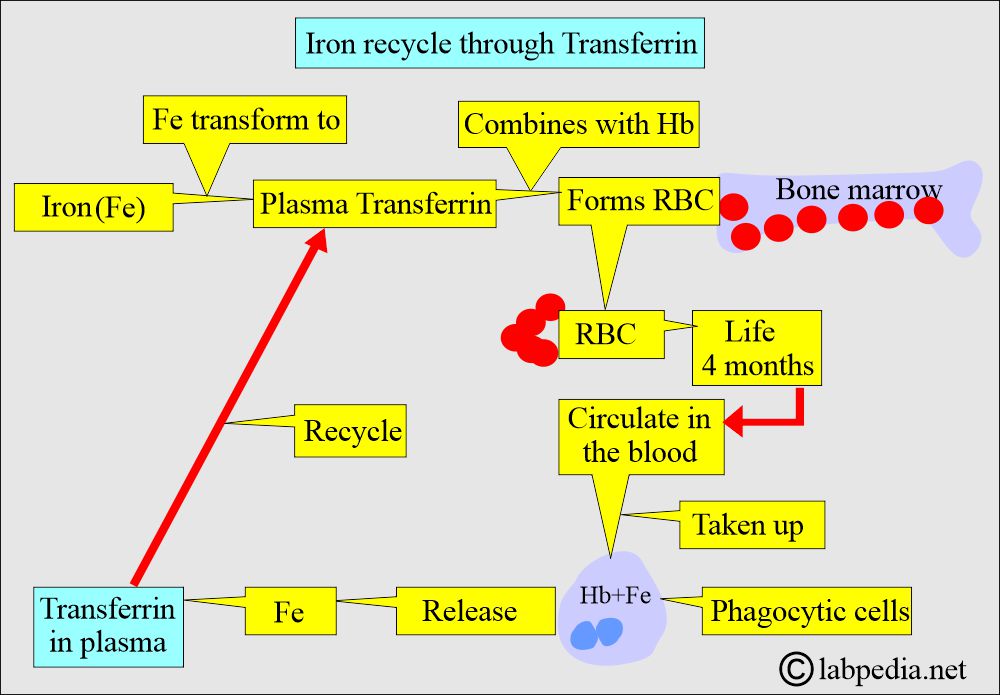
- The iron that is not lost is continuously recycled through transferrin.
How is iron removed from the body?
- Iron forms transferrin, binds to Hb, and supports RBC maturation.
- RBCs enter the circulation and, after around 4 months, are taken up by the phagocytic cells.
- Iron is released by phagocytic cells into the plasma and binds to transferrin.
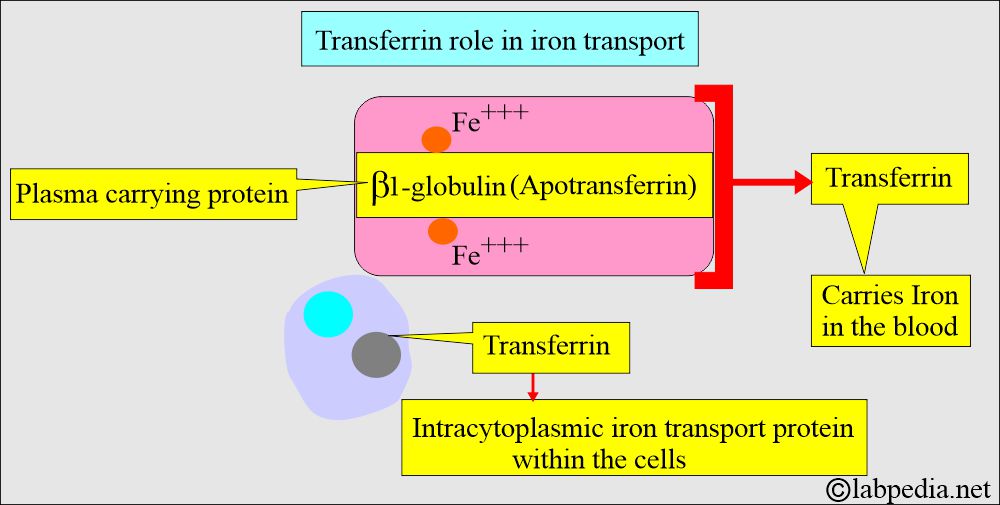
- To understand ferritin, we need to know about Transferrin.
- Apotransferrin is β1-globulin with attached two iron molecules; Fe+++ is called Transferrin.
Ferritin (Serum Ferritin Level)
What are the Ferritin basic facts?
- Ferritin is a good indicator of iron stores in the body. Serum ferritin (an iron-storage protein) correlates with body iron stores.
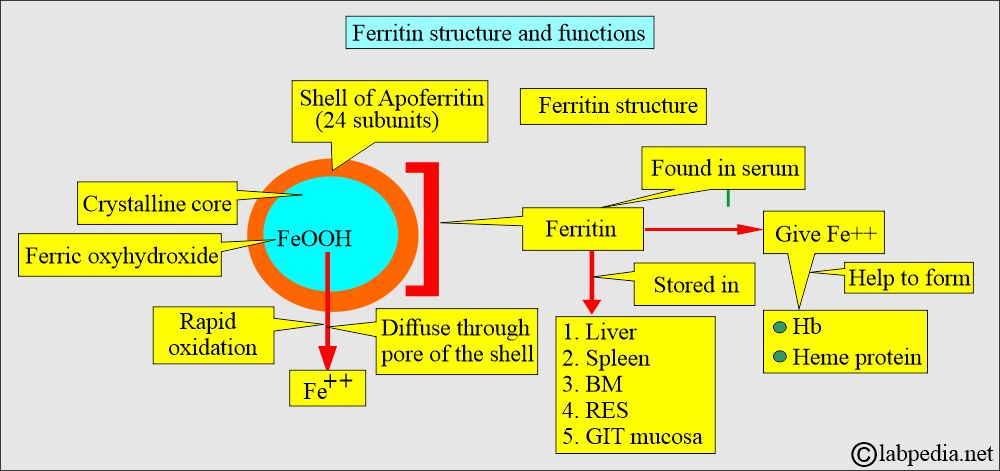
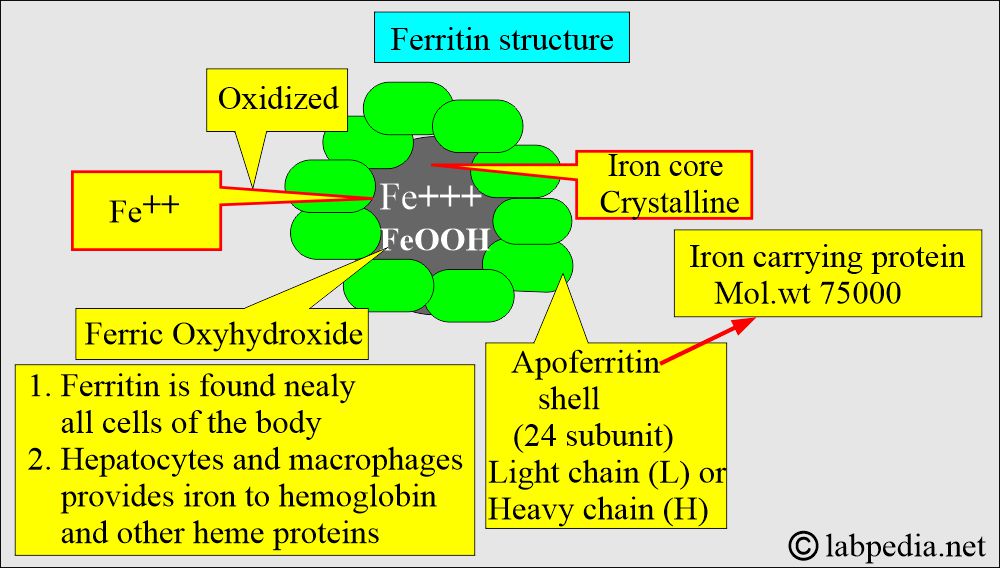
- Ferritin consists of an apoferritin shell with 24 subunits and a crystalline core with iron in the form of FeOOH (ferric oxyhydroxide).
- Ferritin is the primary storage compound for iron, found in the liver, spleen, bone marrow, gastrointestinal mucosa, and reticuloendothelial system.
- It is easily mobilized for utilization by the body.
- It is an indirect measure of the iron store.
- Hemosiderin is the aggregate of ferritin. Iron is released more slowly from hemosiderin for use by the body than from ferritin.
How will you describe the Ferritin structure?
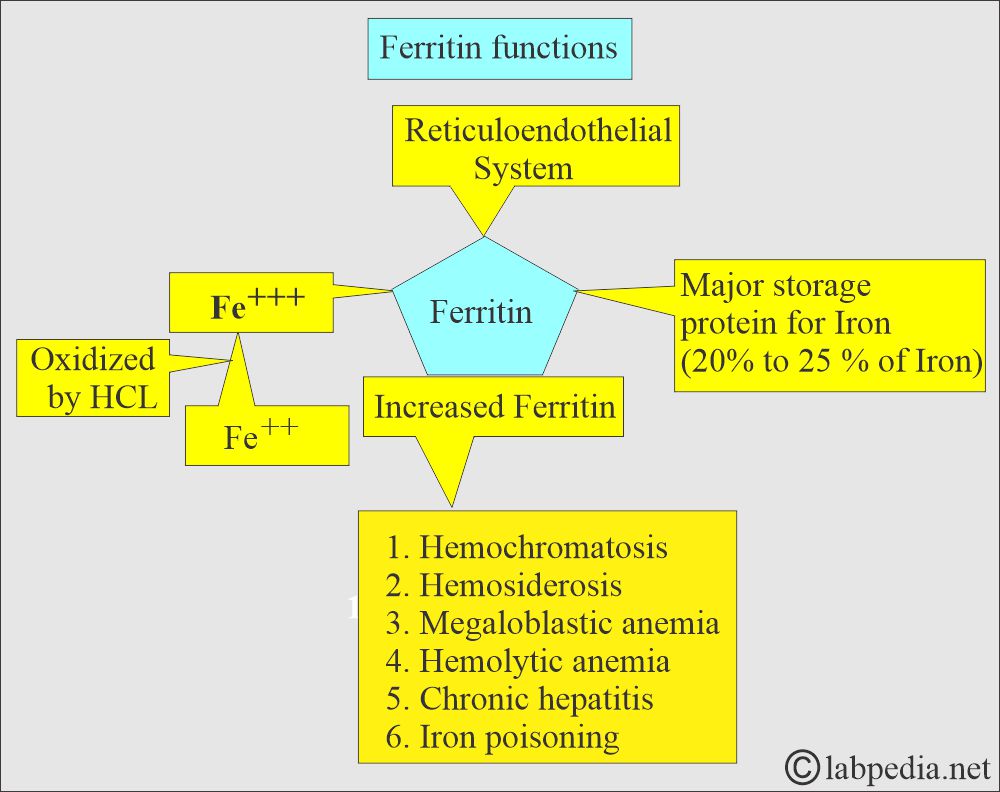
- It is the complex of ferric hydroxide and protein apoferritin formed in the reticuloendothelial system.
- Ferritin = Ferric oxyhydroxide + Apoferritin
- Ferritin has the shape of a hollow sphere that permits the entry of a variable amount of iron for storage (as ferric hydroxide phosphate complexes).
How will you discuss Ferritin pathophysiology?
- Iron uptake by ferritin requires prior oxidation of Fe++ (ferrous) to Fe+++(ferric). This takes place in the stomach, where HCl is present.
- When the body’s iron stores are high, mucosal epithelial cell ferritin is high, and transferrin is low.
- Ferritin is present in the blood in very low concentrations.
- Normally, ∼ 1% of the plasma iron is present in the form of ferritin.
- 40 to 80 mL of blood is lost during the menstrual cycle, and 20 to 40 mg of iron.
- Plasma ferritin concentration declines very early in the development of iron deficiency before changes in hemoglobin appear.
How much ferritin is stored in male/female?
- Ferritin is the major storage protein of iron.
- The ferritin stored in men is roughly 800 mg.
- In healthy females, it is 0 to 200 mg.
- 1 ng/ml of ferritin = Roughly 8 mg of iron stores.
- Iron loss in urine and sweat is <1 mg/day.
- The intestine regulates iron absorption.
- Transferrin is in excess in plasma, but only 30% of it is saturated with iron.
What is the significance of Ferritin?
- Ferritin contains 20% to 25 % iron.
- Ferritin concentration is a good measure of iron stored in the body, both in normal and iron-deficient individuals.
- In conditions of iron overload and some chronic diseases, serum ferritin is not a reliable estimate of iron stores.
- Ferritin level rises persistently in males and postmenopausal women.
- The decrease in ferritin levels indicates reduced iron storage and an increased risk of iron-deficiency anemia.
- Pregnancy is associated with decreased ferritin levels.
- Ferritin levels are also used in patients with chronic renal disease to monitor iron stores.
- Increased ferritin level is a sign of excess iron seen in:
- Hemochromatosis.
- Hemosiderosis.
- Iron poisoning.
- Recent blood transfusion.
- Megaloblastic anemia.
- Hemolytic anemia.
- Chronic hepatitis.
- When Ferritin is combined with serum iron levels and total iron-binding capacity (TIBC), it helps differentiate types of anemia.
- Ferritin, iron, and transferrin saturation concentrations are low in iron deficiency anemia.
- TIBC and transferrin levels are raised.
- Ferritin level is more specific than iron concentration or TIBC for diagnosing iron deficiency.
- Ferritin decreases before anemia or other changes appear.
Does Ferritin act as an acute-phase protein?
- Yes, Ferritin may act as an acute-phase protein.
- It may be elevated, which does not indicate iron storage, like:
- Acute inflammatory diseases.
- Infections.
- Metastatic cancers and lymphomas.
- Alcoholism.
- Collagen diseases.
- Uremia.
- It rises 1 to 2 days after infection onset, and the peak is reached by 3 to 5 days.
What is the Normal ferritin level?
Source 6
| Age and sex | Ferritin level in ng/mL | Ferritin level in mcg/L |
|
|
|
|
|
|
|
|
|
Another source
- Children = 7 to 140 ng/ml.
- Newborn = 25 to 200 ng/ml
- <One month = 200 to 600 ng/mL.
- 2 to 5 months = 50 to 200 ng/mL.
- 6 months to 15 years = 7 to 142 ng/mL.
- Adult male = 20 to 250 ng/ml
- Adult Female = 10 to 120 ng/ml
Type of anemia Ferritin level - Male, anemia of chronic diseases
- <100 ng/mL
- Female, anemia of chronic diseases
- <20 ng/mL
- Iron deficiency anemia
- <10 ng/mL
- Iron overload
- >220 ng/mL
Source 2
- Male = 12 to 300 ng/mL (12 to 300 µg/L)
- Female = 10 to 150 ng/mL (10 to 150 µg/L)
- Children
- Newborn = 25 to 200ng/mL
- One month = 200 to 600 ng/mL
- 2 to 5 months = 50 to 200 ng/mL
- 6 months to 15 years = 7 to 142 ng/mL
What are the conditions under which the Ferritin level is increased?
- Ferritin levels may increase with age in males and postmenopausal females.
- A marked increase was seen in iron overload, e.g., Hemochromatosis and certain liver diseases.
- A slight increase is seen in acute leukemia.
- Inflammatory diseases like pulmonary infections, osteomyelitis, and chronic UTIs.
- Autoimmune diseases such as rheumatoid arthritis and SLE.
- Certain chronic liver diseases.
- Acute myeloblastic and Lymphoblastic leukemia.
- Hodgkin’s lymphoma and breast cancer.
- It may be seen in viral hepatitis or after toxic liver injury. In that case, ferritin is released from the damaged liver cells.
What are the conditions under which the Ferritin level is decreased?
- Iron deficiency anemia, where ferritin level is <10 ng/ml.
- Heavy menstrual bleeding.
- Persistent bleeding of the GIT.
- Poor absorption by the GIT.
How will you discuss various types of anemia and lab workup?
| Disease | Ferritin | Transferrin sat. | Iron | TIBC |
|---|---|---|---|---|
|
Normal | Low | Low | Normal |
|
Low | Low | Low | Increased |
|
Increased | Increased | Increased | Low |
|
low | Low | Low | Increased |
|
Low | Low | Low | Increased |
|
Increased | Increased | normal | Low |
|
Increased | Increased | Increased | Low |
|
Increased | Low | Low | Low |
|
Increased | Increased | Increased | Increased |
|
Normal | Low | Increased | Increased |
TIBC = total iron-binding capacity.
Transferrin sat. = Transferrin saturation.
Questions and answers:
Question 1: What is the role of transferrin?
Question 2: What is the role of ferritin?