Erythrocyte Sedimentation Rate (ESR), vs C-Reactive Protein (CRP)
Erythrocyte Sedimentation Rate (ESR)
What is the sample for Erythrocyte Sedimentation Rate (ESR) and C-reactive protein?
- The whole blood sample is taken in the EDTA (anticoagulant). It measures the rate of sedimentation in one hour.
- Or take blood in a 3.8% trisodium citrate solution.
- The sample is stable for 2 hours at 25 °C and 12 hours at 4 °C.
- We need serum for C-reactive protein (CRP).
What are Indications for Erythrocyte Sedimentation Rate (ESR)?
- It can be done in occult diseases.
- For the diagnosis of acute and chronic infections.
- For collagen vascular diseases.
- In advanced malignancies.
- In tissue necrosis and infarction.
- ESR can be used to monitor disease therapy, especially for autoimmune diseases. It will correlate with the disease’s severity or improvement in the disease course.
- It is useful for diagnosing and monitoring temporal arteritis and polymyalgia rheumatica.
- It is also used for monitoring Hodgkin’s lymphoma.
What is the Pathophysiology of Erythrocyte Sedimentation Rate (ESR)?
How will you define ESR?
- It Is the measure of RBCs settling in diluted plasma over a specified period.
- This is a numeric value in mm over a period of 60 minutes.
What is the principle of ESR?
- This is directly proportional to RBC mass and inversely to plasma viscosity.
- The ESR is the rate at which RBCs settle out of anticoagulated blood in one hour.
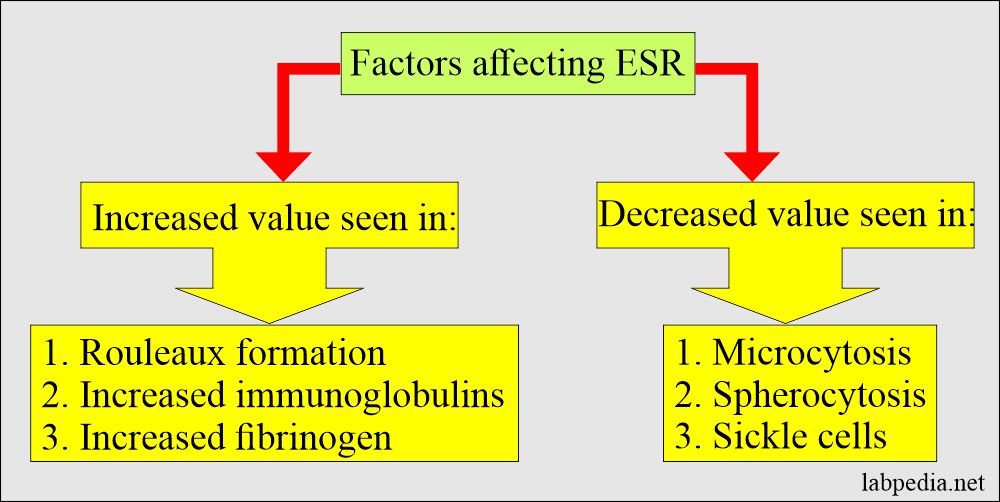
- RBCs give rise to more rouleaux formation in abnormal conditions like inflammatory conditions and the necrotic process, resulting in aggregation of the RBCs, which makes them heavier and more likely to fall rapidly so that there are increased RBCs mass, which increases the ESR due to faster settling of RBCs.
- There are two methods:
- Wintrobe method.
- Westergren method.
- This is a nonspecific but not diagnostic test.
- The ESR correlates with the plasma fibrinogen level and depends on the rouleaux formation of RBCs.
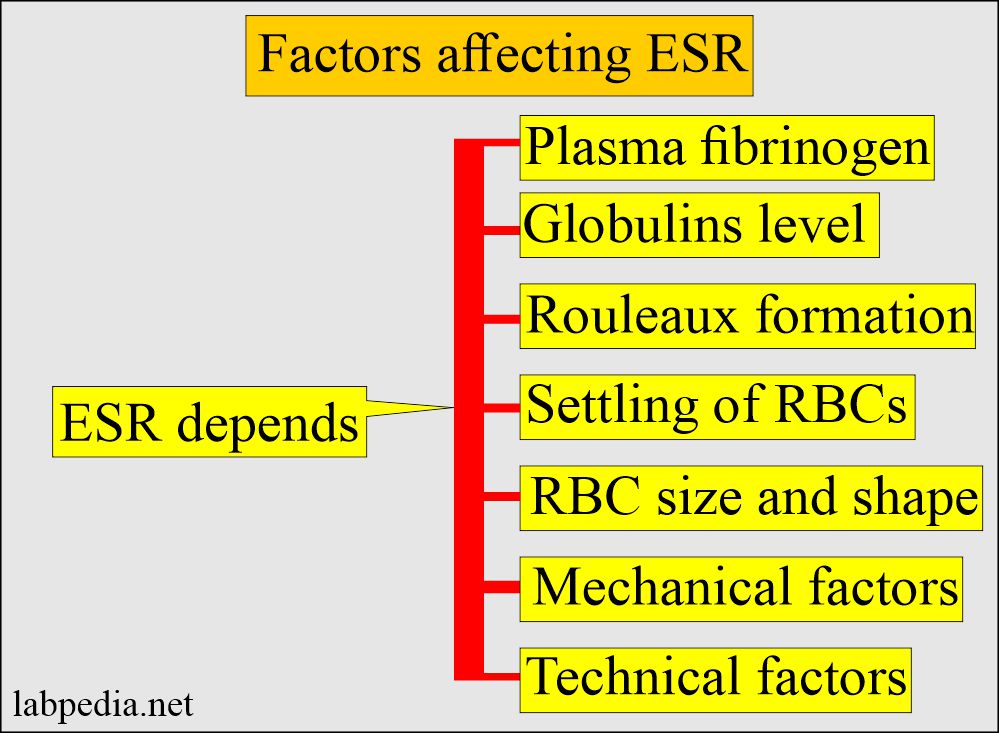
What factors will affect ESR?
- The inflammatory, neoplastic, infections and necrotic diseases increase protein, mainly fibrinogen content of plasma, which leads to raised ESR levels.
- ESR is advised in occult diseases.
- Poikilocytosis, therefore, tends to inhibit sedimentation.
- Increased flattening of RBC, as in obstructive liver disease, leads to accelerating sedimentation.
- ESR should not be used to screen the asymptomatic patient for disease,
- When ESR has been raised, a careful history and clinical examination will usually diagnose the disease.
- This is a nonspecific test for diagnosing chronic diseases like Tuberculosis and raised in malignancies and autoimmune diseases.
- Whenever any patient has raised ESR, he/she needs a thorough workup.
- ESR is raised with aging and anemia.
Whaen Patients with >100 mm /hour ESR have a 90% predictive value for serious diseases?
- Malignancy, particularly myeloma.
- Infection.
- Collagen vascular disease.
- Rheumatoid Arthritis.
- Renal Disease.
- Sarcoidosis.
When will you see raised ESR?
- Paraproteinemia.
- Multiple myelomas.
- Macroglobulinemia.
- This test is useful for diagnosing and monitoring temporal arteritis and polymyalgia rheumatica.
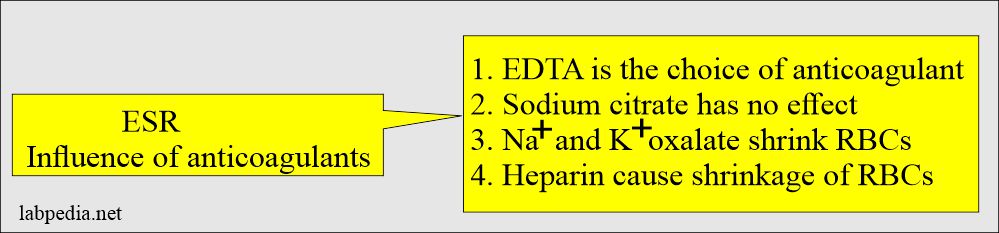
What is the effect of Anticoagulants on ESR?
- Sodium citrate and EDTA do not affect the ESR.
- Sodium or potassium oxalate shrinks the RBCs.
- Heparin also causes shrinkage of the RBCs and gives rise to increased false ESR value.
- So EDTA is the choice of anticoagulant.
What are the limitations of ESR?
- First of all, this is a nonspecific test.
- Some, time is not elevated in the active disease.
- ESR may be influenced (increased) by other factors like pregnancy, anemia, and a few other diseases.
- Fibrinogen concentration.
- Serum cholesterol level.
- Globulin concentration, specifically gamma globulins.
- Rouleaux formation decreases the surface area.
- Sickle cells fail to form rouleaux formation, so there is low ESR.
What is the Normal ESR?
- Male = 0 to 15 mm/hour.
- Female = 0 to 20 mm/hour.
- >50 years
- Male = 0 to 20 mm/hour.
- Female = 0 to 30 mm/hour.
- Child = up to 10 mm/hour.
- Newborn = 0 to 2 mm/hour.
Another source
- Men = 0 to 5 mm/hour.
- Women = 5 to 15 mm/hour.
- There is a progressive increase in old age.
What are the conditions where ESR is falsely low?
- Sickle cell anemia.
- Spherocytosis.
- Hypofibrinogenemia.
- Polycythemia.
What are the conditions where the ESR value is reduced?
- High blood glucose (hyperglycemia).
- In the case of raised phospholipids.
- In the case of raised albumin.
- In the case of raised WBCs.
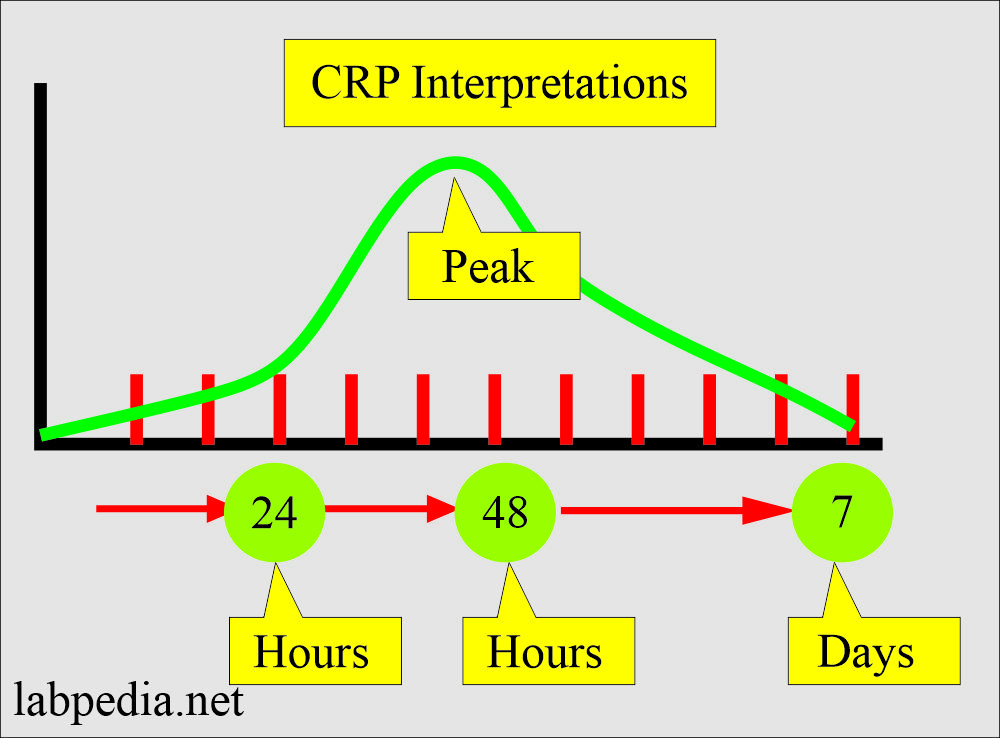
What is the difference between ESR versus CRP?
| Clinical parameters | ESR | CRP (C-reactive protein) |
| Normal level |
Men = 0 to 5 Women = 5 to 15 mm/hour |
<1.0 mg/dL |
| Sensitivity | Less sensitive | More sensitive |
| Pathophysiology (etiology) | Fibrinogen level goes up in the serum, which causes RBCs to clump | Dead and dying cells release chemical factors which stimulate the liver to produce CRP |
| Increase in the level with respect to antibody | No relation to antibody | CRP Increases before the increase in the antibody level |
| Response to inflammation | Late response |
|
| After the inflammation | Take more time | Disappears early |
| Acute myocardial infarction | No relation |
|
| Coronary anginal attack | No relation | Normal |
- ESR is a nonspecific test, but it is one of the best tests to find any abnormality in the body. Whenever you find raised ESR, never ignore it but have a thorough workup of the patients. It definitely shows some underlying disease.
Questions and answers:
Question 1: What is the sensitivity of ESR and C-reactive protein?
Question 2: Is there any relation of antibodies to ESR?