Chapter 7: Immune cells, Nonspecific immune cells
IMMUNE CELLS
Immune Cell Types
- Specific or acquired immune cells
- T-Lymphocytes
- B-Lymphocytes
- Non-Specific Immune Cells
- Neutrophils
- Mast cells
- Basophils
- Eosinophils
- Platelets
Primary Lymphoid Organs
- Bone marrow
- Thymus gland
- In fetus – yolk sac, liver, and spleen.
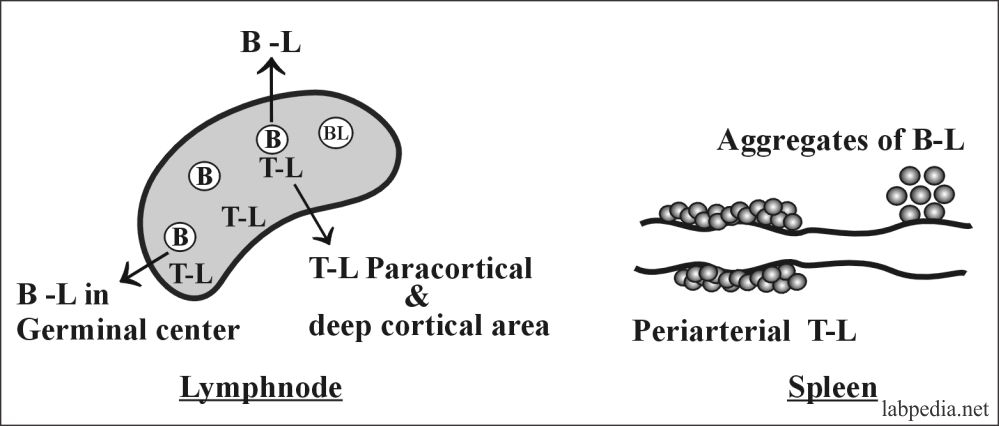
Secondary Lymphoid Organs
- Lymph nodes.
- Spleen.
- Diffuse lymphoid cells of GIT and respiratory tract.
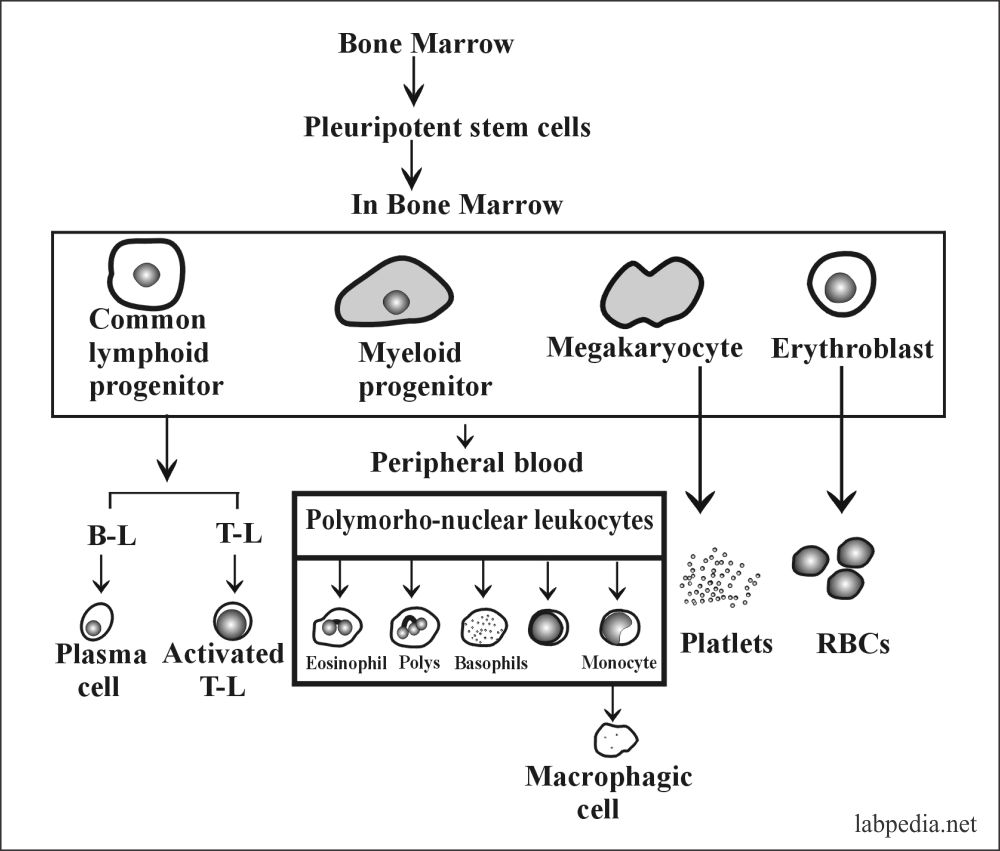
In the bone marrow, the mother cells called pluripotent stem cells transform into a stem cell, which ultimately transforms into various components of the immune system.
MONONUCLEAR PHAGOCYTIC SYSTEM (MN CELL)
The mononuclear macrophagic cells were known as scavenger cells.
Now its role is a complex cell of the immune system and the major role is in the defense against the various types of infections.
Macrophages and their precursors, the monocytes can migrate easily into the tissue from the blood. These monocytes will reinforce and replace macrophagic cells.
The mononuclear phagocytic system needs to replace the old term of the reticuloendothelial system.
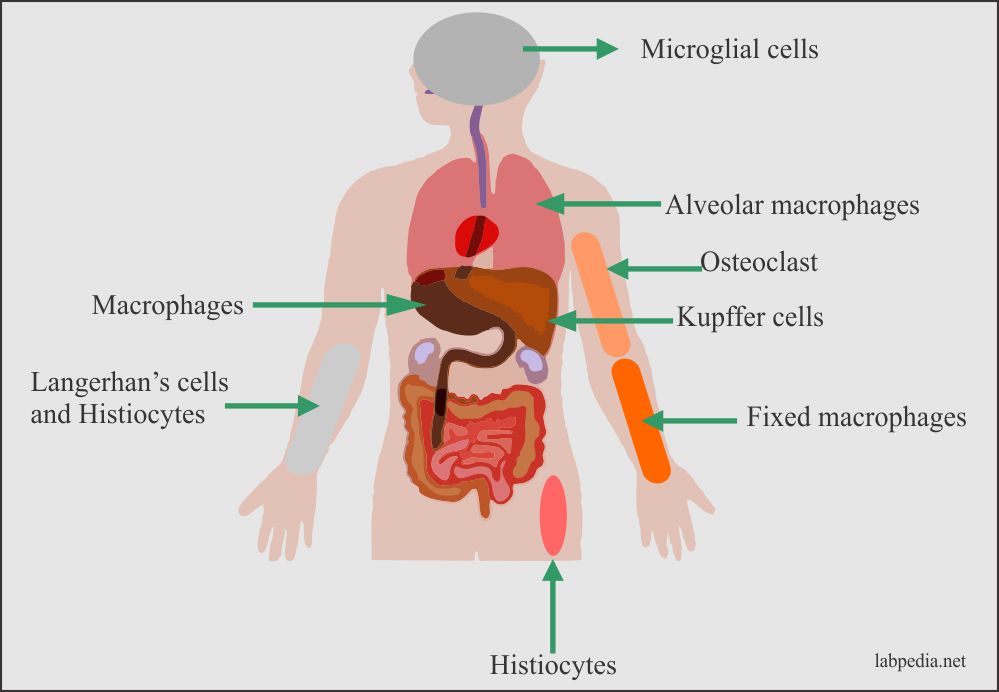
The Mononuclear Phagocytic system cells distribution:
- Promonocytes and the precursor cells in the bone marrow.
- Monocytes are in the peripheral blood.
- Tissue macrophagic cells (Histiocytes) are in the tissues.
- Development of the monocyte- macrophagic system:
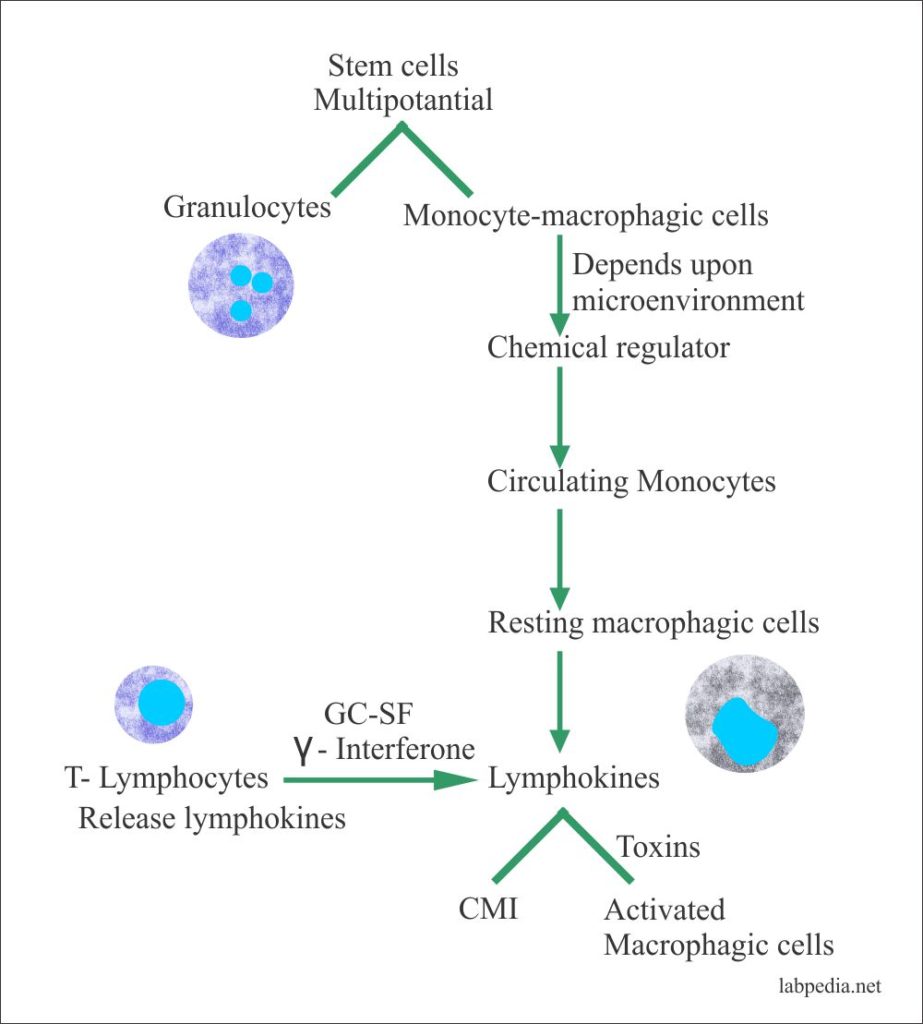
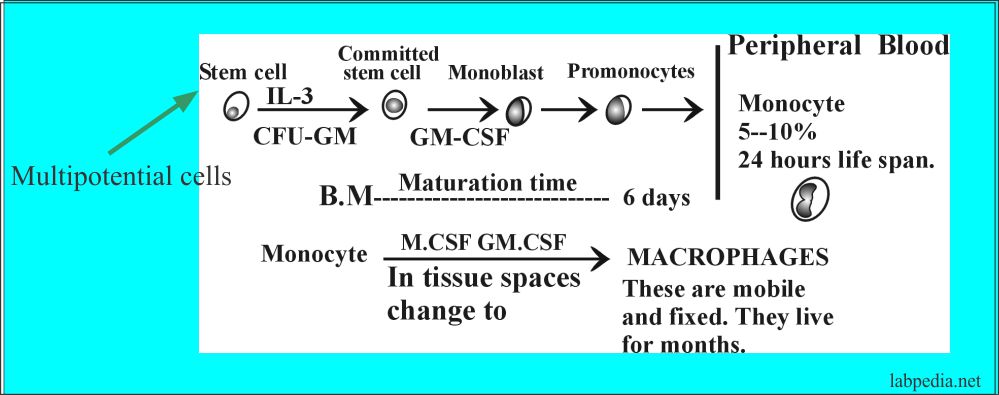
- Monocytes-macrophagic cells develop from the stem cells which are pluripotential cells.
- Then under the influence of lymphokines secreted by the T-lymphocytes (GCSF and γ-interferon) give rise to activated macrophages and Cell-mediated immunity (CMI).
- All these changes take place in the microenvironment and chemical regulators.
- Development of Monocyte-macrophagic system
-
- This is called the system because of the:
- The common origin of the cells taking part.
- These have similar morphology.
- These have common functions like phagocytosis mediated by:
- Receptor for IgG.
- Complement C3.
Phagocytic cells are:
- Professional: These have receptors for IgG and C3b.
- Nonprofessional: These are facultative phagocytic cells like epithelial cells, endothelial cells, and fibroblasts. They become phagocytic when there is a need.
Macrophagic cells are activated by γ-interferon, which is produced by Th1 cells.
Examples of MN phagocytic cells are:
| Location | Name |
| In Liver | Kupffer’s cells |
| In Connective Tissue | Macrophages (histiocytes) |
| In Bone | Osteoclast |
| In CNS | Microglial cells |
| In Lung | Alveolar Macrophagic cells (dust phagocytes) |
| In Skin | Langerhan’s cells and histiocytes |
| Blood vessels | Fixed macrophages |
Table V – MN Phagocytic Cells
Functions of MN Phagocytic Cells:
- The main function of the MN phagocytic system is phagocytosis. They do three inter-related functions in the defensive system like:
- Pinocytosis.
- Phagocytosis.
- Secretion of biologically active molecules.
- Antigen-presenting process (APC) and leads to immune response.
- Chemotaxis.
- Defense against the microbes.
- Destroy the cancer cells.
- Macrophages remove tissue debris, repair wounds, and remove embryonic tissue.
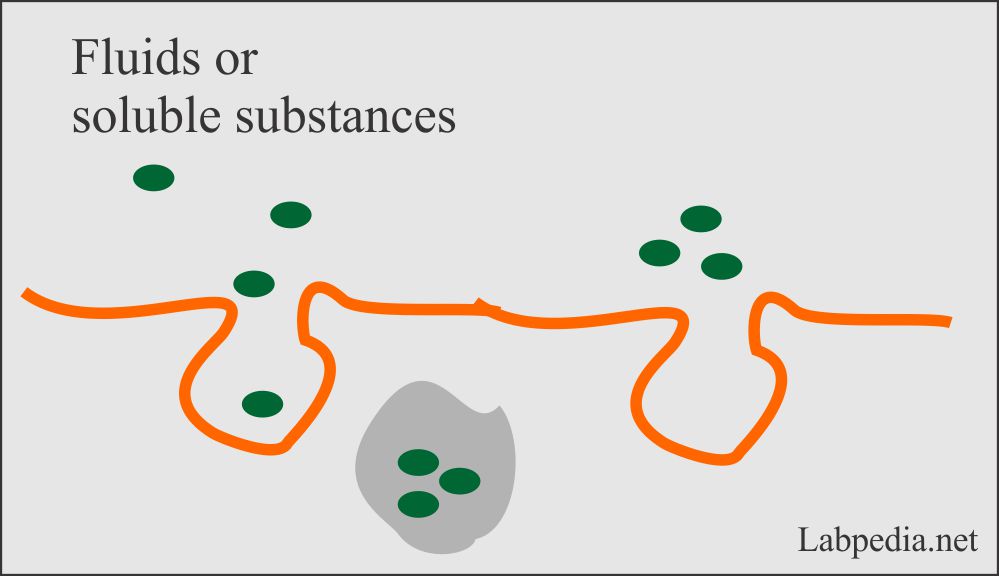
Pinocytosis
Definition:
- This is the process in which phagocytic cells can ingest fluids and solutes with a size of <0.1 nm.
- Basically, pinocytosis primarily used for clearing extracellular fluids and this is part of the immune defense.
- In this process, it generates ATP from the wastes of alternative substances such as lipids in contrast to phagocytosis.
- In the kidney, their cells can separate nutrients and fluids from the urine by pinocytosis.
- Mechanism of pinocytosis:
- The basic concept of pinocytosis is that It involves a cell taking in very small drops of extracellular fluids.
- The cell membrane will wrap around the drop and pitch it off into the cell.
- The molecules inside of the created vesicles can then digest it or absorbed it into the cytosol.
- Pinocytosis is also seen in the intestinal epithelial cells for the absorption of the fat droplets.
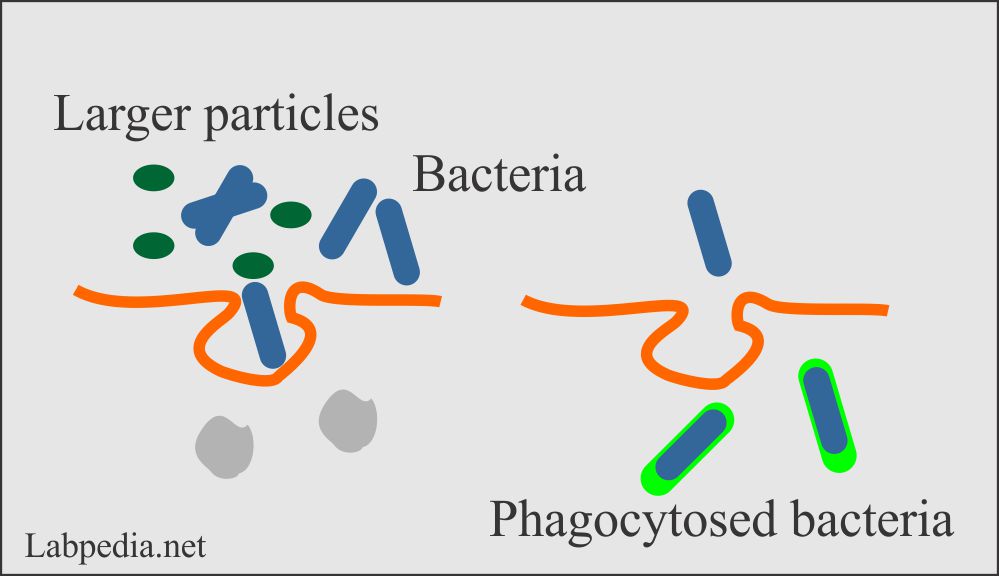
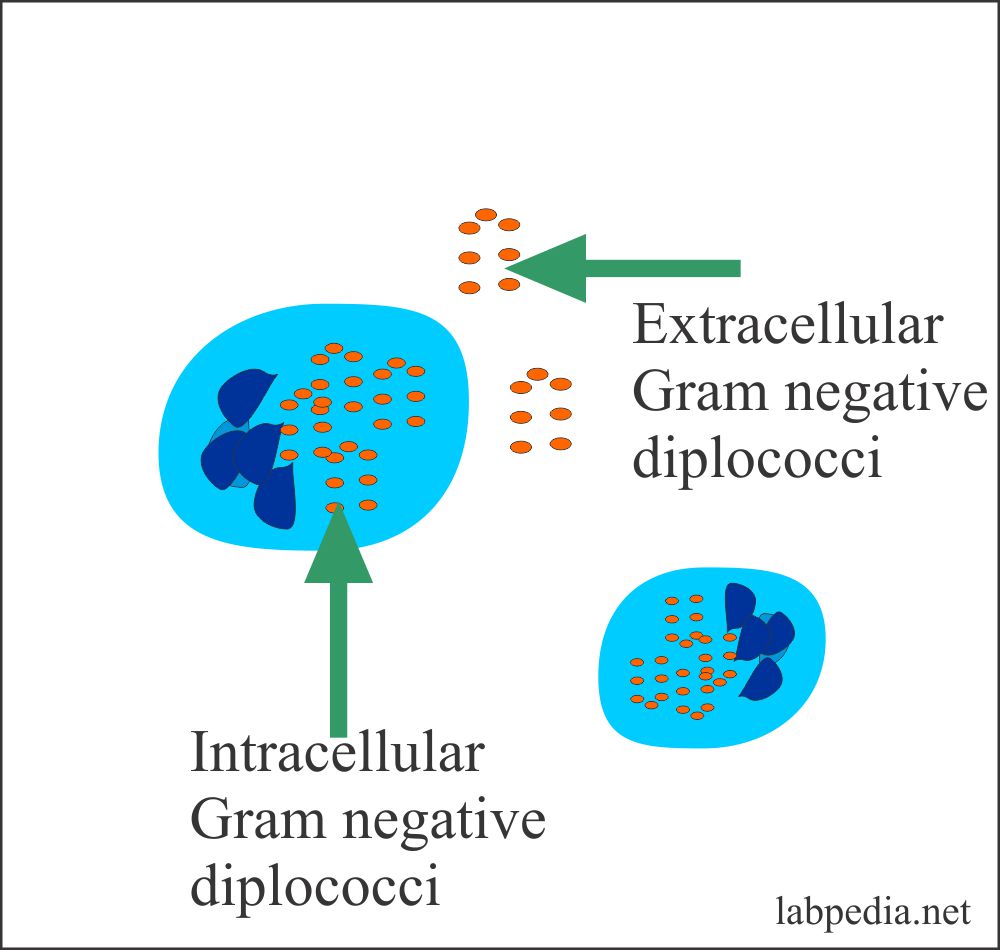
Phagocytosis
In this process, phagocytic cells can ingest the particulate where the size is >0.1nm. The best example is bacteria.
- Phagocytosis is the fundamental function of ingesting and killing the microorganism e.g.:
- Intracellular parasites.
- Some fungi.
- Extracellular pathogens like pneumococci from the blood circulation.
- Phagocytose particulate and aggregated soluble material from the blood circulation.
- The activated macrophages have the ability of microbicidal and tumoricidal function.
- By phagocytosis, these cells dispose of dead or dying cells.
- Macrophages of the spleen ingest the aged RBCs.
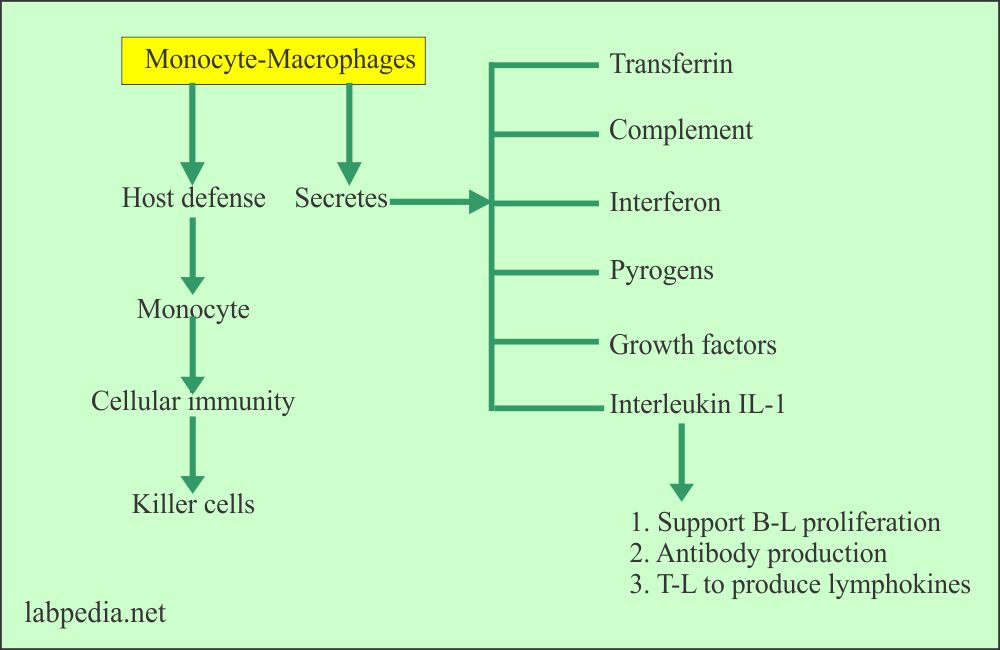
- Monocyte-macrophages secretes many factors for host defense.
- In cellular immunity, monocytes become killer cells.
A. Process of Phagocytosis may be:
- Immunological with the help of IgG and C3b.
- Nonimmunological is the direct ingestion of the material.
- Phagocytic activity increases when there are inflammation and tissue damage due to the release of chemicals that attract the macrophagic cells.
- Activated macrophagic cells move to the site of inflammation more easily than the resting macrophages.
- Macrophages have the ability of diapedesis, that they can move from the endothelium to the site of inflammation by the microbes.
- Chemotaxis factors are from complements, neutrophils, lymphocytes, and cancer cells.
- Proteolytic enzymes are present on the surface of monocytes and that will reject the tumor cells.
- Recognition of the antigen on the macrophagic cells surface by the T-lymphocytes and the second helper is the MHCII molecules.
- The process of phagocytosis takes place in stages:
- C5a and LTB4 attract the phagocytic cells, activate them, promote diapedesis.
- Chemotaxis takes place by the secretion of chemoattractants.
- The monocytes appear after the neutrophils at the site of inflammation.
- Now the phagocytes reached near the bacteria and engulf them. This is mediated through the Fc receptor.
- The last stage is the digestion of the engulfed bacteria.
- This digestion process takes place through anaerobic glycolysis.
- There are lytic enzymes in the lysosomes for this process.
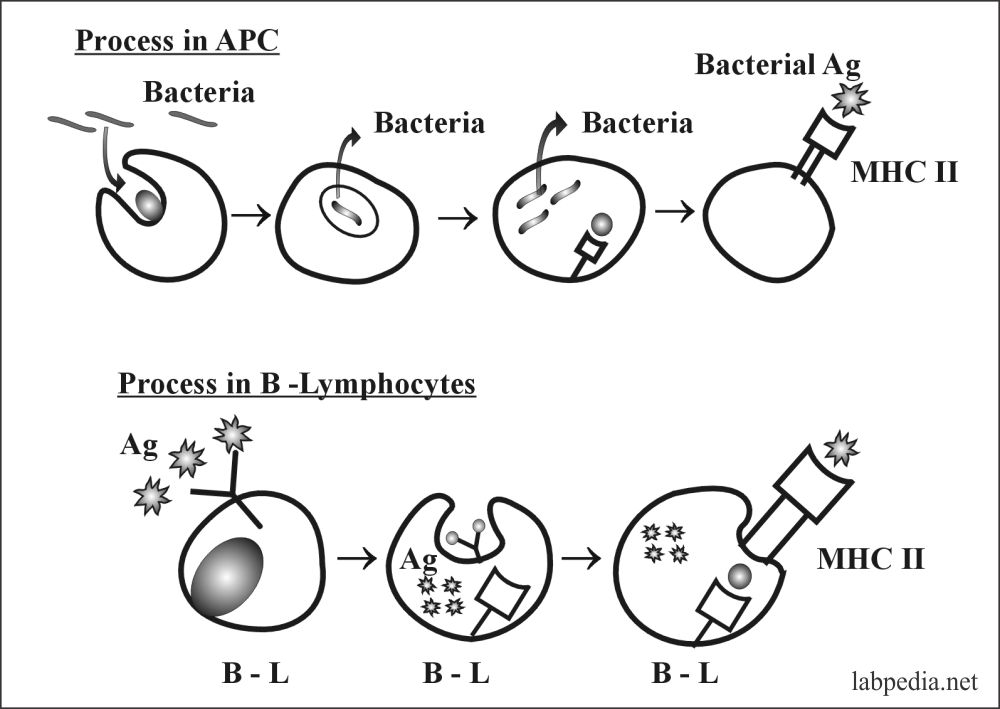
B. Antigen presentation to immune cells (APC) role of the MN phagocytic cells:
- These cells have APC (antigen-presenting cells) function with the help of MHC class I and class II molecule.
- Macrophagic cells process the antigen and make it a more biochemically modified form of the antigen which is more reactive to lymphocytes particularly T-helper cells and start the immune process.
C. Production of Monokines by monocyte-macrophages:
They can produce:
- Transferrin.
- Components of complement.
- Prostaglandins.
- IL-I (monokines).
- Interferon-α.
- TNF-α.
D. Chemotaxis:
- They are actively motile to chemotaxis leading to chemotaxis.
- Chemoattractants like C5a and LTB4 activate phagocytic cells and promote diapedesis and chemotaxis.
E. Production of the growth Factor:
MN phagocytic cells produce IL-I that promotes differentiation of B-L and T-L.
F. Production of Toxic Metabolites:
Phagocytes produce toxic metabolites, which cause lysis of bacteria and fungus. Also, produce proteolytic enzymes.
G. Cell-Mediated Immunity (CMI):
These are important cells in cell-mediated immunity (CMI).
H. Mechanism of toxic Injury to Antigen by Mononuclear Phagocytic cells:
Toxic Injury to the Antigen is due to the following toxic material produced by the phagocytic cells:
- Free O radicals
- Superoxide anions
- OH Free radicals (hydroxyl)
- OCL- hypochlorous anion
- O-singlet oxygen
- H2O2 (hydrogen peroxide)
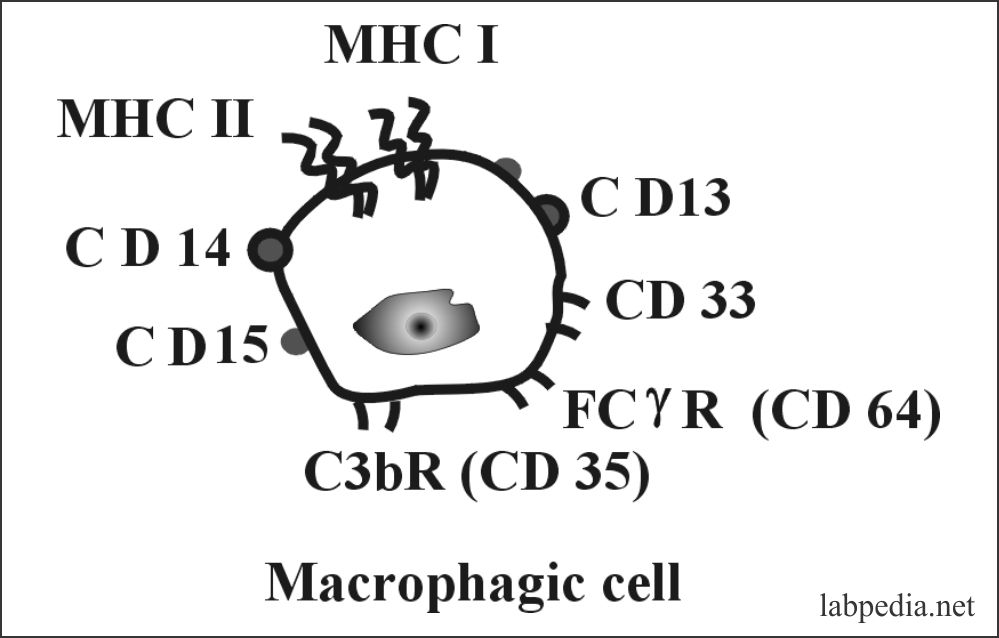
I. Characteristics of MN Phagocytes Cells:
- Receptors
- These cells have Fc γ-receptor for IgG and receptor for C3b.
- Surface Markes:
- These are CD13, CD33, and CD11b R for FcγR and C3b. MHC class I and II molecules are present. CD4 molecules are present but at low concentration. CD11b/CD18- leucocyte function-associated Ag 1(LFA-1) is present.
- CD14 is a specific marker and function is unknown. CD4 molecules are present in low concentrations.
- Macrophagic cells have the potential of phagocytosis because of the presence of the FcγR receptor and the C3b receptor.
- Macrophagic cells can perform phagocytosis nonspecifically and immunologically.
Difference between Monocytes and Macrophages:
| Characteristic features | Monocytes | Macrophages |
| Size of the cell | 15 to 18 µm | 25 to 80 µm |
| N:C ratio | 2:1 or 1:1 | 1:2 or 1:3 |
| Nuclear morphology | Folded nucleus | Round |
| Nuclear position | Central | Eccentric |
| Nuclear chromatin | Blue-purple, fine reticular pattern | Clumped chromatin |
| Nucleoli | None | 1 to 2 |
| Cytoplasm | Pale-grey blue/ abundant and pseudopods | Abundant with vacuoles |
| Cytoplasmic granules | Numerous fine, pale red throughout the cytoplasm | Numerous azurophilic granules |
H. Diseases associated with monocyte-macrophages malfunction:
- The susceptibility to infection is confirmed and associated with the dysfunction of the monocytes-macrophages.
- The best example is defective phagocytic killing is associated with chronic granulomatous diseases, e.g. subcutaneous abscess, abscess in the lung, liver, spleen, and lymph nodes.
- Qualitative dysfunction of the monocyte-macrophages leads to lipid storage diseases like Gaucher’s disease and Niemann-Pick disease.
| Abnormality of monocyte-macrophages | Diseases associated with the abnormality |
| Impaired phagocytosis |
|
| Defect in the release of macrophagic activating factors |
|
| Defective monocyte toxicity |
|
| Defect in the phagocytic killing |
|
| Defect in the migration |
|
| Qualitative disorder of monocyte-macrophages |
|
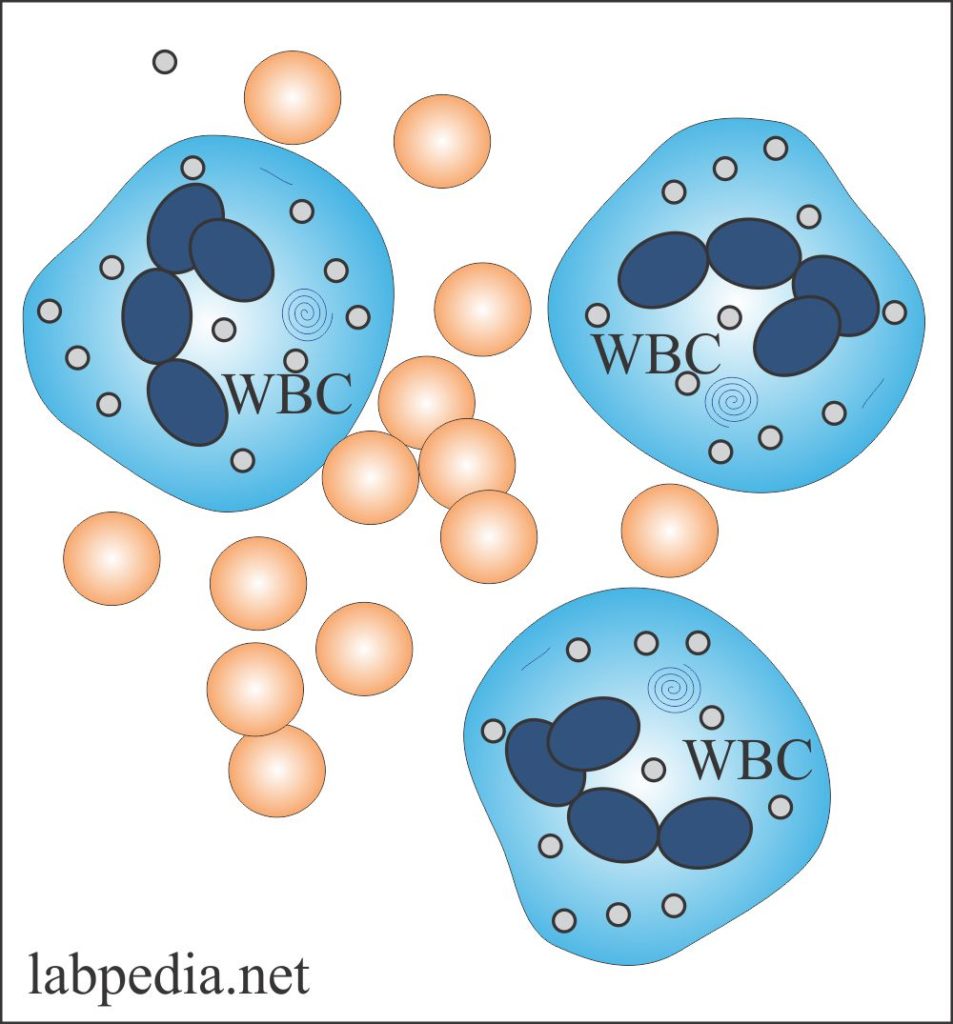
NEUTROPHILS
- Functions:
- Neutrophils (neutrophilic polymorphonuclear leukocytes) are the primary source of defense.
- They have a major role in the defense of bacterial and fungal infections.
- These are the principal cells with the property of phagocytosis.
- Structure:
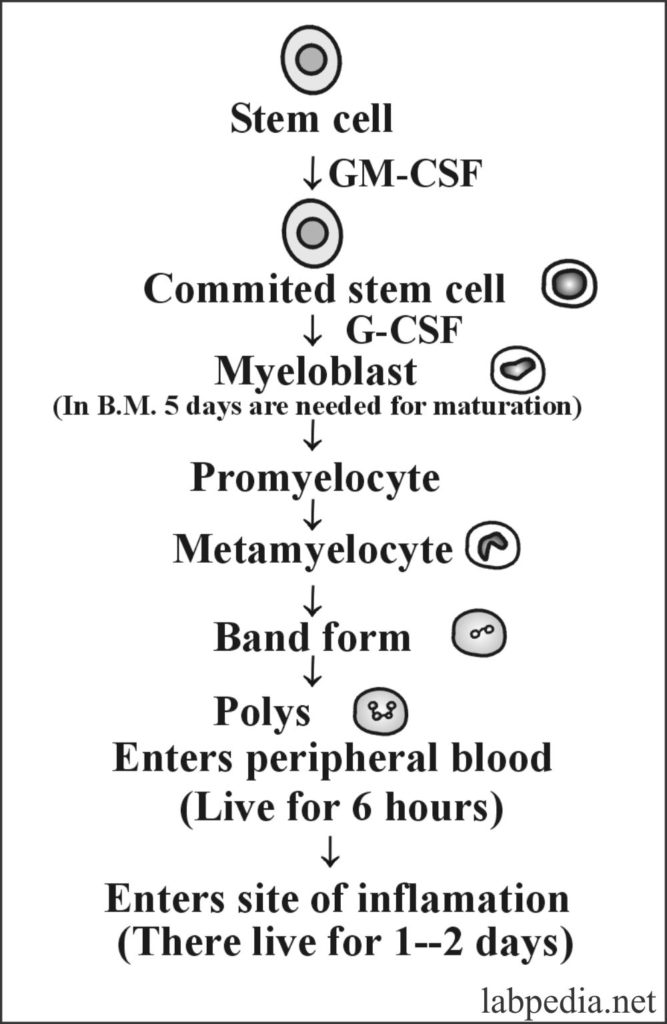
- In the peripheral blood, these are 60% (50-70%) of the total leucocyte count. Their half-life in peripheral blood is 6 hours and in the tissue spaces is 1-2 days.
- These have a multilobate nucleus, which can make rapid transit from the blood through tight gaps in the endothelium.
- These are the main components of acute inflammation and these are activated by infection to kill the offending organism.
- More than 100 billion polys are in circulation of 70 Kg body weight /24 hours.
- More than 100 billion polys are in circulation of 70 Kg body weight /24 hours.
- There are two types of polys:
- Circulating neutrophils
- Neutrophils attach to the endothelium and by diapedesis reach to the site of inflammation.
- Development of the neutrophils:
- These cells develop from the stem cells in the bone marrow by the variety of various growth factors.
- Neutrophils number can increase 10 times during acute inflammation.
A. Neutrophil cytoplasmic granules:
Neutrophils have two types of Granules in the cytoplasm:
- Primary or azurophilic granules appear during their development in the bone marrow. These are bluish and 33% of the total granules in the cytoplasm. e.g. hydrolytic enzymes, myeloperoxidase, lysozyme (microbicidal) and other is collagenase.
- Secondary granules are 67% of the total granules in the cytoplasm. These are lysozyme, collagenase, histaminase, vit B12 binding proteins and some of these are specific like lactoferrin.
B. Activation of Neutrophils:
Neutrophils are stimulated by several stimuli like C5a, C3a, LTB4, and Interleukin 8.
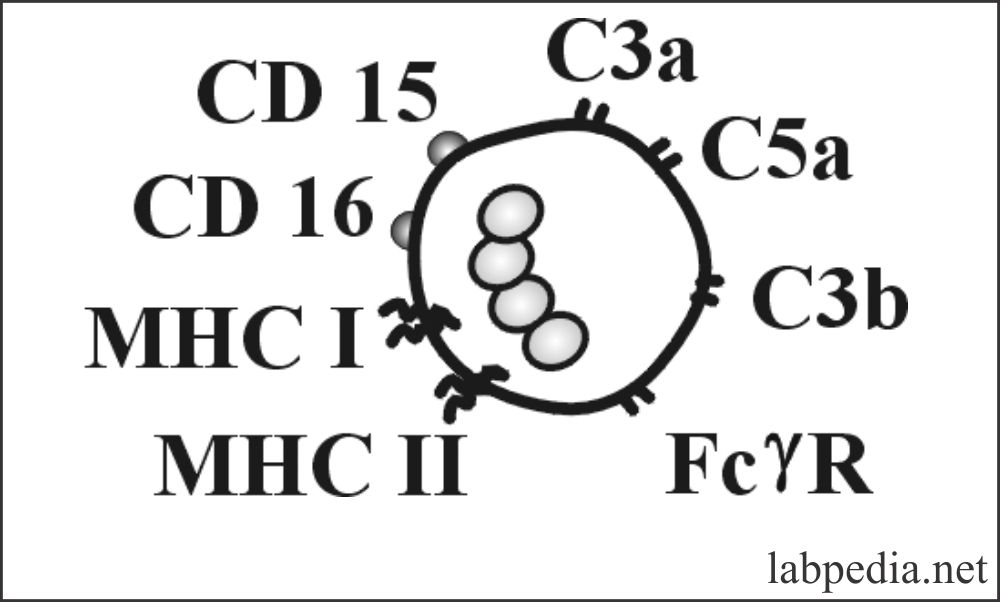
C. Important Features of Neutrophils (surface markers):
- 70-90 % of peripheral blood polys have an Fc-γ receptor.
- Other receptors are for Fc α-receptor (for IgA), C3b, LTB4, C5a, and C3a.
- CD molecules are CD11b, CD15, and CD16.
- There are receptors for GM-CSF, G-CSF.
- There are no receptors for IgD and IgE.
- There is the presence of MHC class I and II molecules.
D. Functions of Neutrophils:
- Neutrophils are attracted by chemotaxin and lead to chemotaxis. The most common chemotactic factors are C5a, IL 8, and LTB 4.
- They take part in opsonization (phagocytosis).
- They take part in ADCC (Antibody-Dependent Cellular Cytotoxicity).
- These can hydrolyze natural and synthetic substrates like polysaccharides, proteins, and lipids.
E. Abnormal neutrophils functions:
- Patients with neutropenia are prone to repeated infection.
- The above group has:
- Repeated attacks of pneumonia.
- Recurrent bacterial infection.
- Disseminated repeated cutaneous pyogenic infection.
- Life-threatening bacterial and fungal infection.
- The above group has:
- In case of defective neutrophils mobility, more chances for:
- Rheumatoid arthritis.
- Cirrhosis of the liver.
- Chronic granulomatous diseases.
- Lazy leucocyte syndrome.
- Marked defect in the neutrophils response to chemotaxis is seen in:
- Diabetes mellitus.
- Sepsis.
- Congenital abnormalities of neutrophils are:
- Chediak-Higashi anomaly.
- iC3b receptor deficiency.
- Chronic granulomatous diseases.
- Specific granules deficiency.
- Myeloperoxidase deficiency.
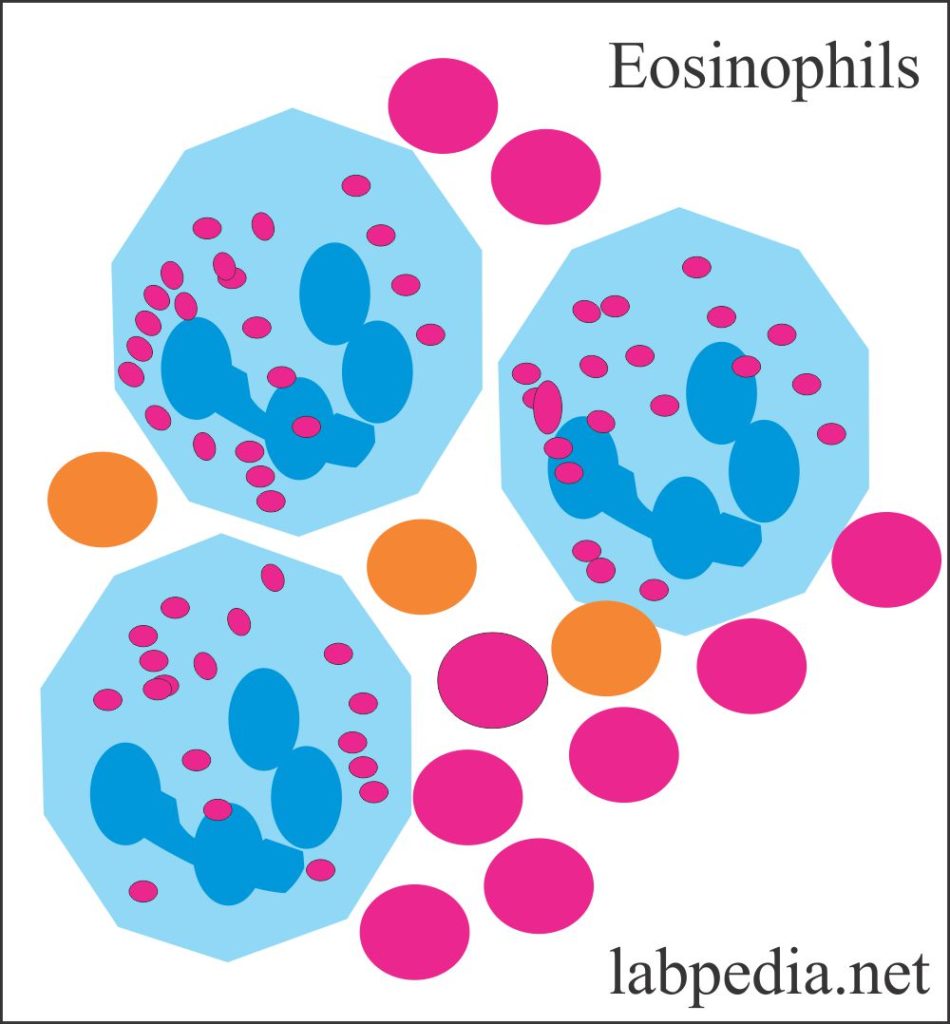
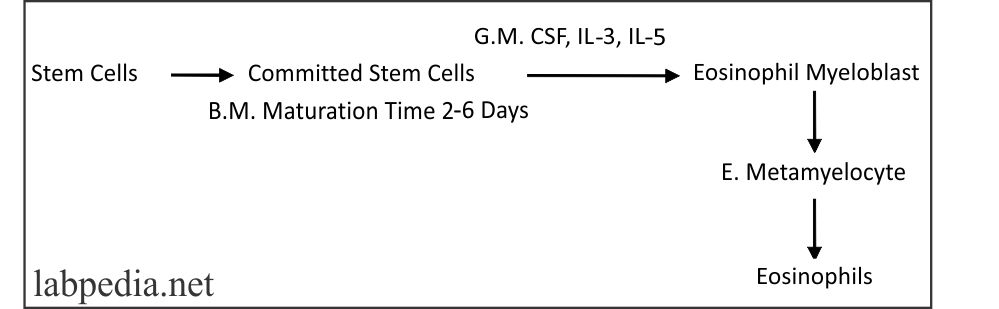
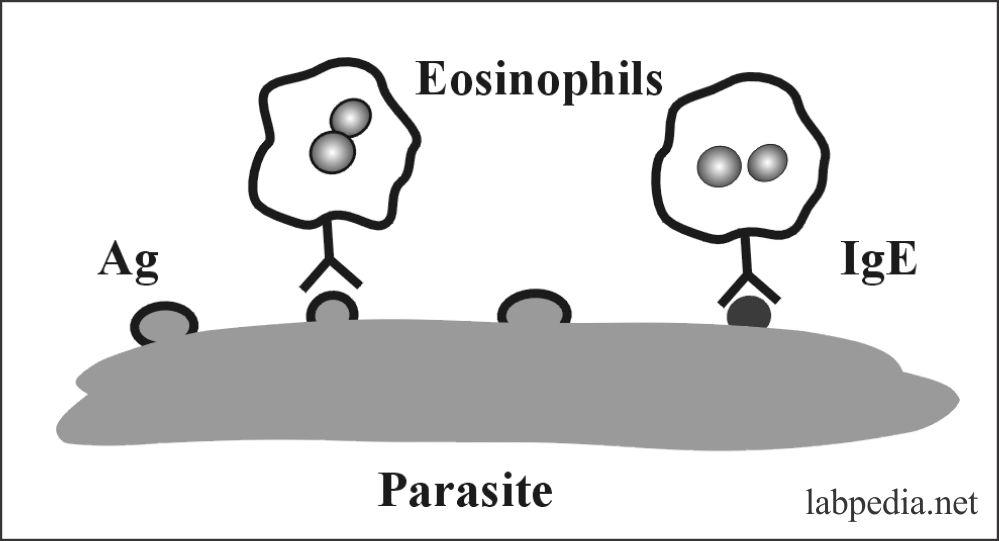
EOSINOPHILS
- Eosinophils are considered to be a homeostatic regulator of inflammation.
- These cells suppress the inflammatory response to prevent excessive inflammatory reactions.
- They also play the host defense mechanism because of their ability to kill the parasites.
- These are bone-marrow-derived granulocytes. These are bilobed and 1-5 % of total leukocytes. Their size 12-17 mm in diameter.
- Circulating half-life is 6-12 hours while in connective tissue they survive for several days.
- For every circulating eosinophil, there are 200 eosinophils in bone marrow, and 500 eosinophils in connective tissue.
A. Eosinophil Granules:
There are of two types of granules:
- Primary granules: These are poorly characterized granules in a lipid vesicle, which provide release of LTC4, LTD4, and PAF.
- Specific granules: These are:
- Major basic proteins.
- Eosinophil cationic proteins (ECP).
- Eosinophils neurotoxin. This is toxic to helminths while ECP is potentially bactericidal.
- Eosinophil peroxidase.
B. Surface Markers and Receptors of Eosinophils:
- There are receptors for C3b, IgE (IgεR11), and IgG (IgγR).
- IgγR is low affinity as compared to IgεR present on mast cells and basophils.
- 10 to 30% Eosinophil show IgG receptor (IgγR).
C. Activation of Eosinophils:
Eosinophils are activated by a variety of mediators for which there are receptors like – Receptor for C3b, C4b, C5a, and LTB4. Other receptors are for – IL3 and IL5.
D. Functions of Eosinophils:
- Eosinophils have the potential for phagocytosis (ADCC).
- These have an important role, particularly in a parasitic infestation.
- These have an anti-inflammatory role by the release of histaminase enzymes.
- They produce PAF, leukotrienes, and prostaglandin.
- They can destroy bacteria, fungi, and parasites.
MAST CELLS AND BASOPHILS
Mast Cells
- Mast cells derived from the hematopoietic stem cells and survive for months or years in vascular tissue and the most organs.
- Mast cells VS basophils:
- The tissue basophils are the mast cells, both are closely related in their function and biochemical characteristics.
- Both take parts in a similar manner in acute and delayed allergic reactions.
- Granules of both cells have similar morphological characteristics.
- Both cells contain histamine and heparin.
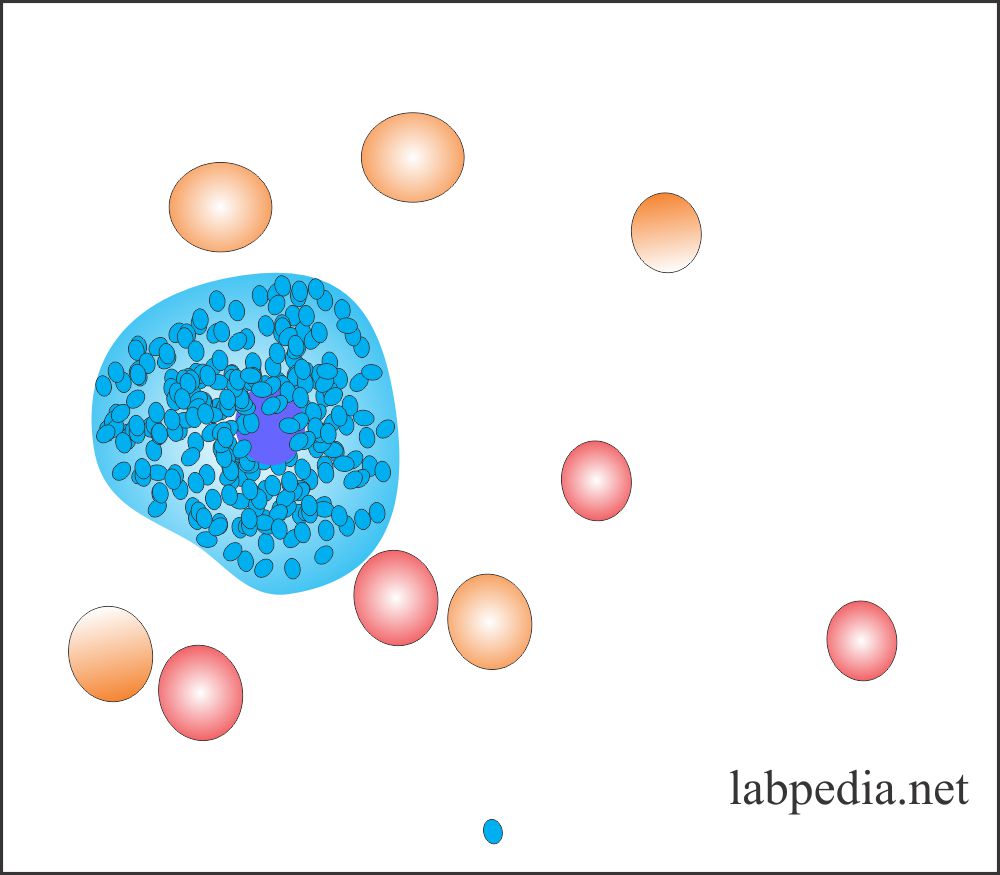
- Structure:
- Mast cell cytoplasm contains large prominent, intensely stained violet-blue granules.
- The granules are usually round and with a size of 0.1 to 0.3 µm.
- These granules can obscure the nucleus.
- The nucleus is small round or oval and is not segmented.
- Mast cells are present in various tissue like skin, lung, connective tissue, and bone marrow,
- They give IgE mediated inflammatory response.
Features of Mast Cell
- The cytoplasm contains granules, which are rich in histamine (50-200 granules/cells).
- These cells possess a high-affinity receptor for IgE (FcεR).
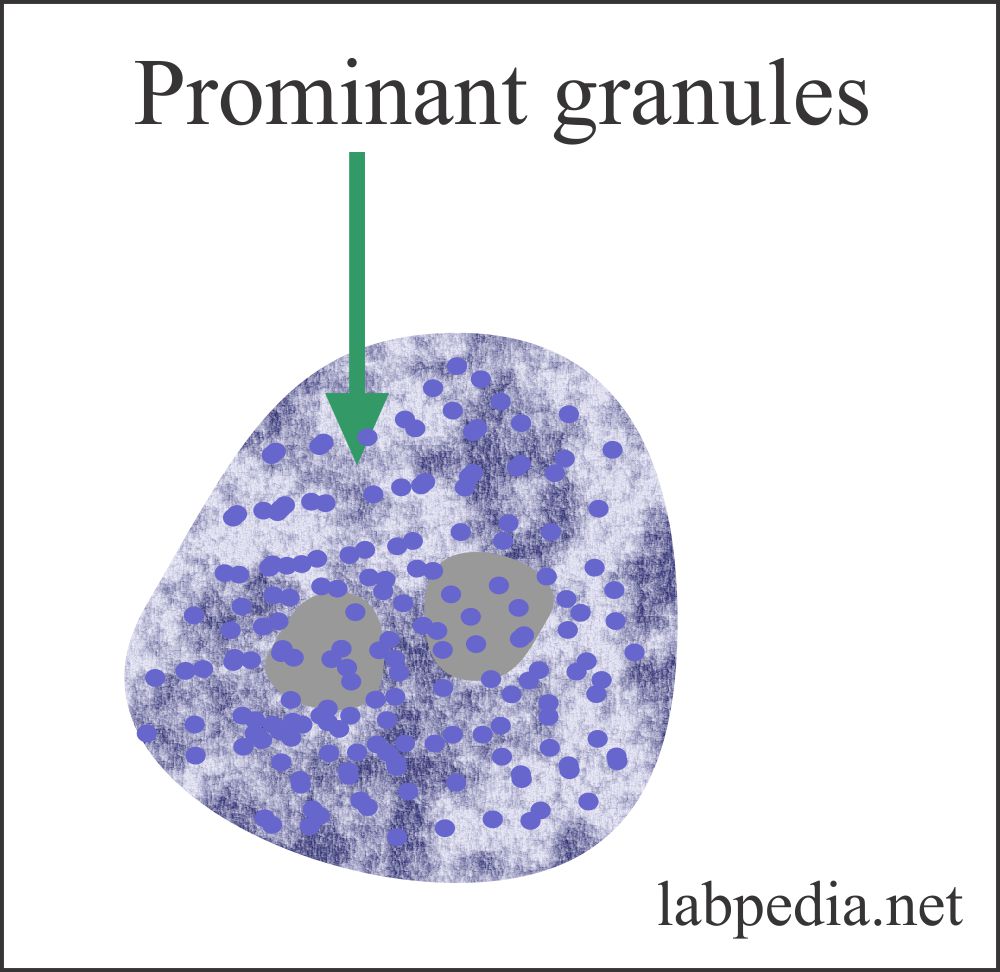
BASOPHILS
- Basophils have common features like mast cells. They also develop from stem cells.
- Stem cells under the influence of IL3, GM-CSF give rise to basophils.
- These are the smallest cells measuring 5-7 um in diameter.
- These are 0. 2 to 1% of total leukocytes in the peripheral blood.
- Cytoplasmic granules are:
- Their cytoplasm also contains histamine and heparin granules.
- The granules are very prominent and may overshadow the nucleus.
- Markers and Receptors of Basophils:
- There are receptors for IgE, C3a, C5a, and C3b.
- Functions of Basophils:
- May take part in phagocytosis.
- It can give rise to chemotaxis.
Mast Cells and Basophils Chemical Mediators:
- Primary Mediators (Preformed)
- Histamine
- Protease enzyme
- ECF-A
- Proteoglycans (heparin and chondroitin sulfate).
- Secondary Mediators
- Functions of Mast cell and Basophil:
- Mast and basophil cells have an important role in the type 1 hypersensitivity reaction.
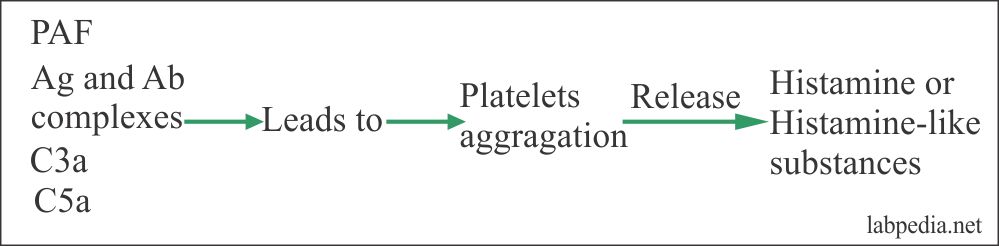
PLATELETS
- Platelets are non-nucleated cytoplasmic detachments derived from megakaryocytes.
- Platelets are half the size of RBC around 2mm in diameter.
- Receptor:
- Platelets possess receptors for IgG, IgE, and show MHC-I molecules.
- Platelets can release – Histamine and Histamine like substances.
- Functions:
- PAF, immune complexes, C3a, and C5a can lead to platelet aggregation and ultimately release of histamine and histamine like substances.
Importance of Platelets
Platelets take part in blood coagulation, in hypersensitivity reactions, and inflammatory process.