Chapter 29: Acquired Immune Deficiency Syndrome (AIDS), HIV Infection
ACQUIRED IMMUNE DEFICIENCY SYNDROME (AIDS)
Definition
This is defined as a modified defect in cell-mediated immunity.
This is because of a virus leading to immune deficiency syndrome.
Historic Back Ground
1980 – T-lymphotropic virus type 1 (HTLV-I) was isolated in 1980 and HTLV-II in 1982.
1981—CDC (center for disease control) noticed 5 pneumocystis carinii in young homosexuals in Los Angeles. Another group of 26 young patients had Kaposi sarcoma.
1983 – Researcher at Pasteur Institute in Paris isolated a retrovirus from a homosexual man with lymphadenopathy. The virus was called lymphadenopathy-associated virus (LAV).
- American researchers isolated the same virus. They gave it the name human T – lymphotropic retrovirus (HTLV) type III.
1984 – The American researcher Dr. Gallo and his team proved that HTLV III was the cause of AIDS.
- Later on, it was proved that LAV and HTLV III was the same virus and was given the name HIV (human immune deficiency virus) to avoid the names’ confusion.
- The original HIV type I (HIV-I) was the cause of AIDS; the second virus was added as HIV – type II (HIV-II ) and was identified in 1985.
- These two viruses are related and have a similar overall structure.
1987—59000 cases of AIDS were reported, and 40,000 were in the USA.
1989—85000 cases were in the USA, and 5 million cases were in the world.
1996—at the end of 1996, estimates were 10 million HIV-infected people in the world.
1999—one of the sources estimated 30 million cases in the world.
1983—Prof. Luc Montagnier (Pasteur Institute) discovered HIV and traced it back to 1970 pooled sera.
Epidemiology
- HIV-II is endemic in West Africa and appears to less pathogenic as compare to HIV-I.
- 70% of the reported cases of HIV are in the USA.
- It is estimated that 1.2 million Americans are involved with HIV infection currently. 1 out of 7 of them doesn’t know that they have HIV infection.
- Untreated end-stage cases of HIV will die in three years.
Worldwide reports of HIV are in more than 100 countries.
The incidence of HIV infection in 1994 North America, Europe, and sub-Saharan Africa is shown in the following table.
| Location | Male Incidence | Female Incidence | Total Number Infected |
| North America | 1/75 | 1/700 | 10,00,000 |
| Sub-Saharan Africa | 1/40 | 1/40 | 6,000,000 |
| Western Europe | 1/200 | 1/1400 | 500,000 |
Table XXIX – Incidence of AIDS
1996—There was an estimate of 10 million HIV infected people.
- A dramatic reduction in North America’s documented rates is 10% down to 0.5% per year. At the same prevalence of HIV infection in I/V drug abusers, Bangkok rose from less than 5% to over 40%.
- Two% of the cases occur in the pediatric age group, where more than 90% occur from mother to newborn. The remaining 10% are hemophiliacs.
India—There are 4 million HIV cases, and this is second to Africa.
China—This country will have 10 million carriers by 2010.
International statistic by CDC December 2001 and Joint United Nations Programme.
Today 40 million people living with HIV/AIDS.
37.1 million Adults.
18.5 million Women.
3.0 million Children (< 15 years).
In 2001: AID caused roughly 3 million people were 1.1 million females and 58000 children.
The majority of HIV people, approximately 95% of total global cases, live in the developing world.
Some of these HIV viruses are listed in the following table according to their history and origin:
| Types of AIDS Viruses | Old Name | Source |
| 1. HIV I (cytopathic) |
HTLV III LAV(Lymphadenopathy virus) |
AIDS-victims (1983) |
| 2. HTLV I |
HTLV (Human T-L Leukemia virus) |
Leukemia Patients (1978) |
| 3. HTLV II | HTLV II |
Hairy cell Leukemia (1982) |
|
4. STLV III (MAC) (Simian T-L Leukemia Virus Macqua) |
– | – |
|
5. STLV III (AFG) (Simian T-L Leukemia Virus African Green) |
– | 1985 |
| 6. HIV II (cytopathic) | LAV II |
AIDS patients (1986) |
Table XXXII – Types of HIV viruses
- >80% of the cases are seen in the developing countries, and the spread is 80% through sexual contacts (70% vaginal and 10% anal).
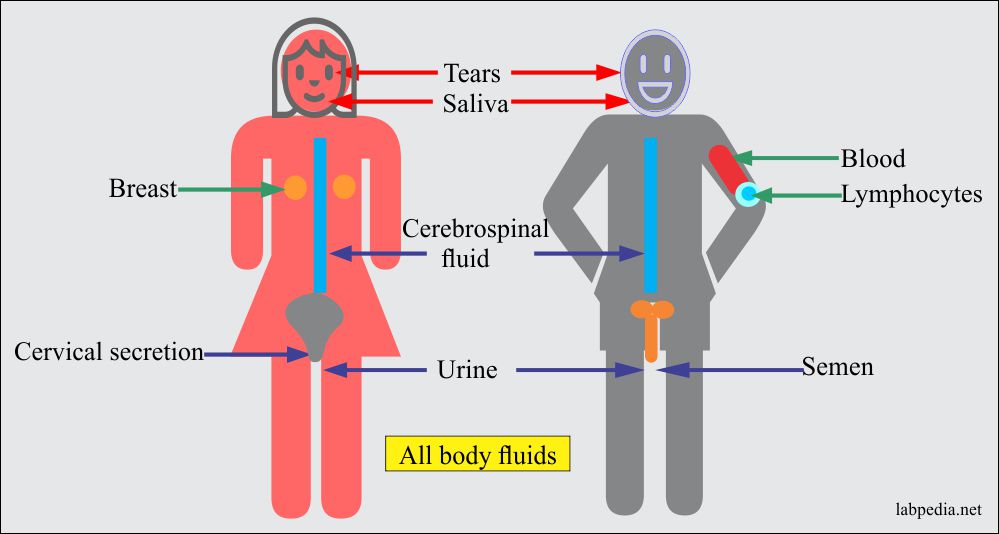
- HIV has been isolated virtually from all body fluids. It is present in the blood, semen, cervical secretion, saliva, tears, breast milk, CSF, plasma, urine, and lymphocytes.
- STD: This is a sexually transmitted disease. There is a greater concentration of HIV in semen than vaginal secretions.
- Infected blood and blood products are the sources, reaching 90%.
- It can spread through contaminated needles and syringes.
- Children of infected mothers rate are 20-70%.
- 8% mode of transmission is unidentified in the USA.
- 50% = Homosexual/Bisexual.
- 20% = I/V drug abuser.
- 20% = Blood transfusion before 1985.
- 10% = Heterosexual.
- It is present in the Bone marrow.
- Lymphoid cells (CD4+) are also a carrier of this virus.
- It can spread through Monocytes and macrophages bearing low-level CD4+ molecule, e.g., alveolar macrophages, microglial cells, Langerhan’s cells in skins, myelomonocytic in B.M precursors, dendritic cells, and thymocyte precursor cells.
Transmission of the virus in various contacts:
| Route | Risk of Transmission |
| Receptive and intercourse with an infected partner | 1/100 – 1/150 contacts |
| Heterosexual intercourse with an infected male partner | 1/500 –1/1000 contacts |
| Heterosexual intercourse with an infected female partner | 1/1000 – 1/2000 contacts |
| Needle prick injury | Approximately 1/250 contacts |
| Child delivered of infected Mother | 1/3 – 1/8 |
Table XXX – Rate of Transmission
HIV is a fragile virus and cannot survive for a larger period outside the body, so:
- No risk to normal social contacts.
- No transmission through coughing, sneezing, and sharing of toilets and swimming pools.
- No transmission from insects.
HIV STRUCTURE
HIV-Human Immune Deficiency Virus Structure:
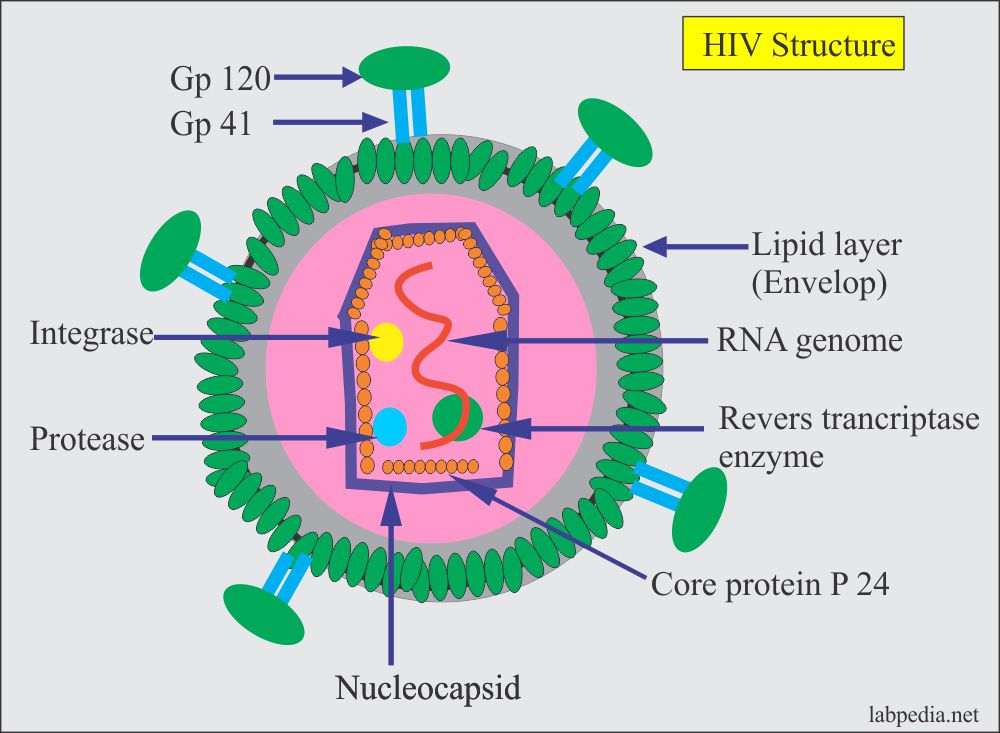
- This virus is a member of the retrovirus family, a small enveloped virus containing a single-stranded RNA genome.
- HIV is a single-stranded diploid RNA virus measuring 100 to 120 nm in diameter.
- Viral nucleic acid and replication enzymes are contained within a core surrounded by capsid proteins. It consists of an outer lipid layer with protruding glycoproteins (gp) molecules. The core has RNA-genome, reverse transcriptase enzyme, and proteins.
- gp 120 is anchored to gp41, which is part of the lipid outer layer.
- The core contains proteins called p24 and p25.
- Reverse transcriptase enzyme is present in the core, and it helps to convert viral RNA to DNA. Later on, this process reverses again into RNA, the so-called retrovirus.
Viral genes are:
- Gag
- Codes for p24.
- Codes for proteins p17, p9, and p7.
- Env
- Codes for two glycoproteins:
- gp 41.
- gp 120.
- Codes for two glycoproteins:
- Pol
- Produce DNA polymerase.
- Produce endonuclease.
Gag forms group-specific proteins (Ag). These are core proteins (p) named as p24 and p18.
Pol forms polymerase, reverse transcriptase enzyme, and other enzymes like protease and integrase.
Env forms envelop proteins, which are necessary for the interaction and penetration of target cells. These are gp120 and gp41.
Other genes, e.g., ZaZ, γeγ, and nef, have been identified as having a regulatory effect on viral assembly and drugs that modulate their function.
Location of the HIV proteins and gene:
| Type of HIV | Type of the protein | Location site and gene |
| HIV-I | gp 41 | Envelope (transmembrane protein), env gene |
| gp 120/160 | Envelope (external protein), env gene | |
| p 24 | Core (major protein), gag gene | |
| HIV-II | gp 34 | Envelope (transmembrane protein), env gene |
| gp 140 | Envelope (external protein), env gene | |
| p 26 | Core (major protein), gag gene |
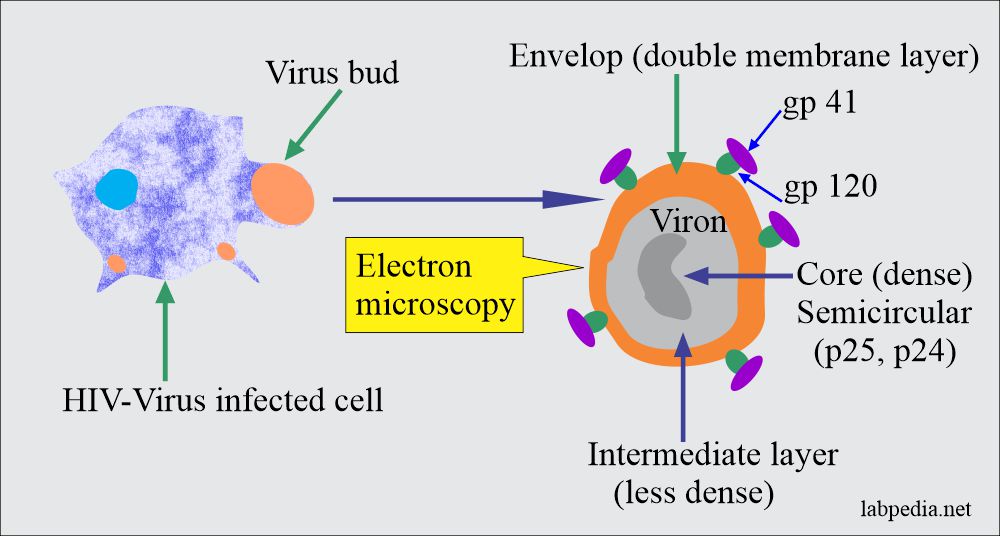
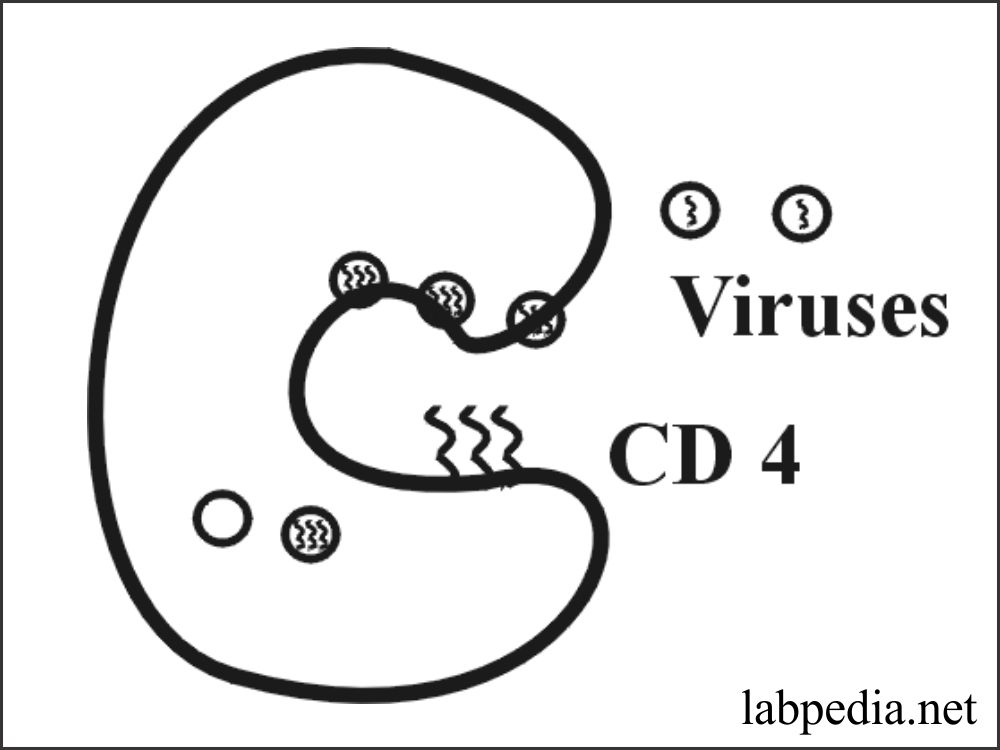
HIV infecting other cells on E/M:
Virus buds out of the cells and on electron microscopy show virus bud. This has a double layer envelops, a dense core, and a less dense intermediate layer.
Two main HIV viruses are causing AIDS, and their brief differences:
| Property | HIV I | HIV II |
| 1. Envelop proteins | Gp41, gp120 | gp36, gp105 |
| 2. Core proteins | P24, P18 | P34, P68 |
| 3. Prevalence | Worldwide pandemic | Endemic in West Africa and now spreading in India |
Lifecycle of HIV
HIV life cycle can be summarized:
- HIV has a CD4+ receptor present on CD4+ T-helper cells and macrophages.
- The virus attaches through gp120 to the CD4+ molecule on the cells.
- Then it is internalized, and with the help of Reverse Transcriptase Enzyme, it changes RNA to DNA and integrates with target cell DNA with the help of viral integrase.
- These are known as Provirus. Double-stranded DNA is then internalized and inserted into the host cell genome.
- What follows, latency or viral replication, is dependant upon the state of activation of the cell. When the virus is assembled and leaves the cells, it does so by budding out, incorporating the host cell membrane into its coat.
The life cycle of the Human immune deficiency virus (HIV):
The dose of HIV Infection
Exactly not known but estimated as 10-100 viruses may cause infection.
Clinical Features of the HIV Infection
The incubation period is variable from 3 weeks to 6 months and, in some cases, even up to many years.
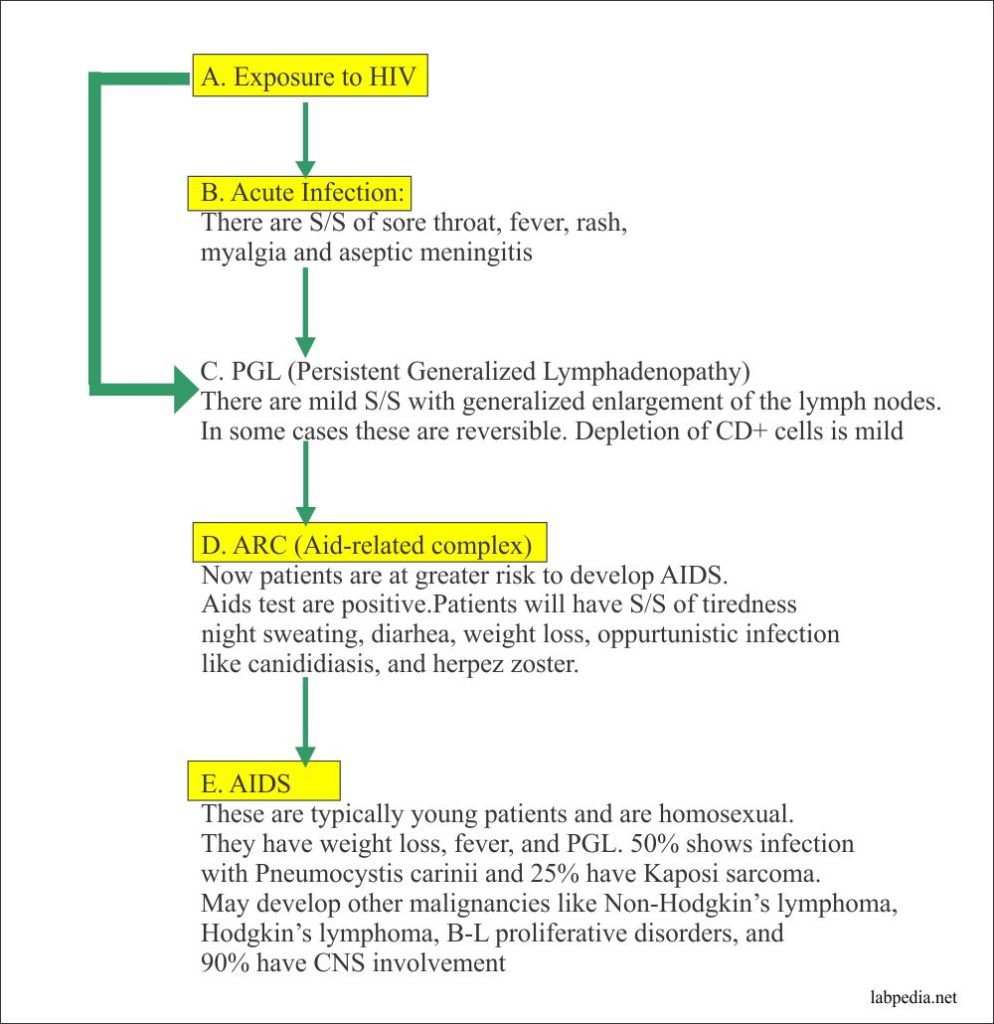
These patients may develop other malignancies like Non-Hodgkin’s lymphoma, Hodgkin’s lymphoma, B-L proliferative disorders, and 90% show CNS involvement.
CDC classification of AIDs patient:
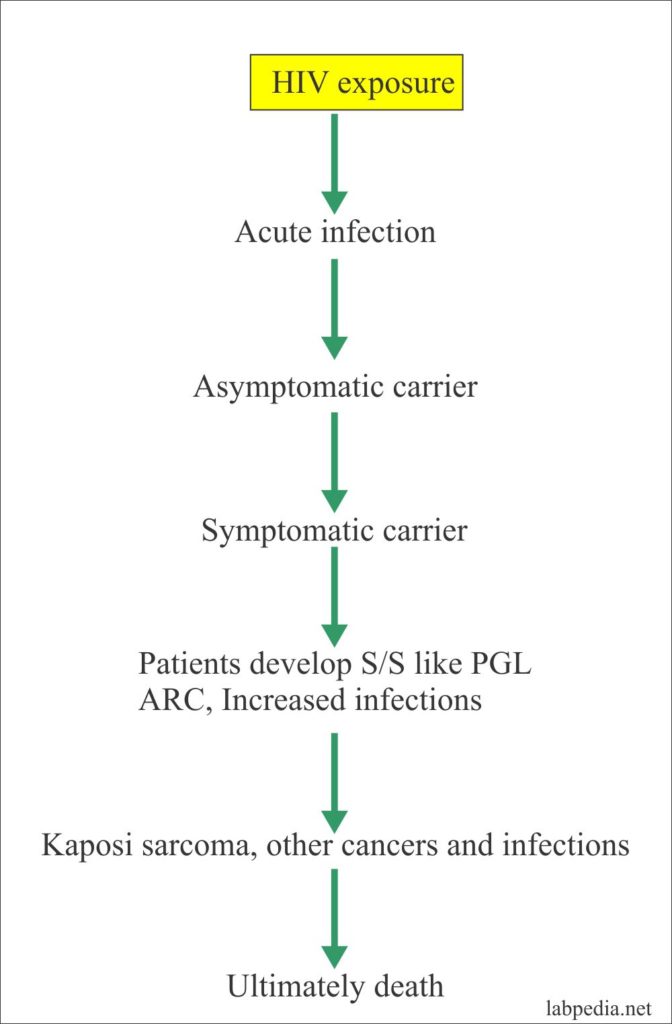
- The spectrum of the disease can be summarized as follows.
Classification and Staging of HIV-Infection:
CDC Classification: This divides these patients into different groups.
| Group | Clinical stage |
| 1 | Acute infection |
| II | Asymptomatic, HIV, fully positive for serological test |
| III | PGL and relatively asymptomatic |
| IV | The patient will have other diseases |
| A. ARC | |
| B. Neurological involvement | |
| C1. Opputunistic infections (P.carinii) | |
| C2. Milder secondary infections like candidiasis and H.zoster | |
| D. Secondary cancers like Kaposi’s sarcoma, Nonhodgkin’s lymphoma, and cervical neoplasm | |
| E. Other complications like interstitial pneumonitis and chronic lymphoid neoplasm |
- CDC revised classification was based on the number of CD4+ Lymphocytes. With a decreasing number of CD4+ cells, the patient will end up with AIDS.
| CD4+ Cells | CD4+ Percentage | Clinical Categories | ||
|
A Asymptomatic Acute HIV or PGL |
B Symptomatic Not A or C Condition like ARC |
C AIDS-indicator conditions |
||
| 1. ³ 500/ml | >29% | A1 | B1 | C1 |
| 2. 200-400/ml | 14-28% | A2 | B2 | C2 |
|
3. < 200/ml (AIDS indicator) |
> 14% | A3 | B3 | C3 |
Table XXXI – CDC Revised Classification in 1993
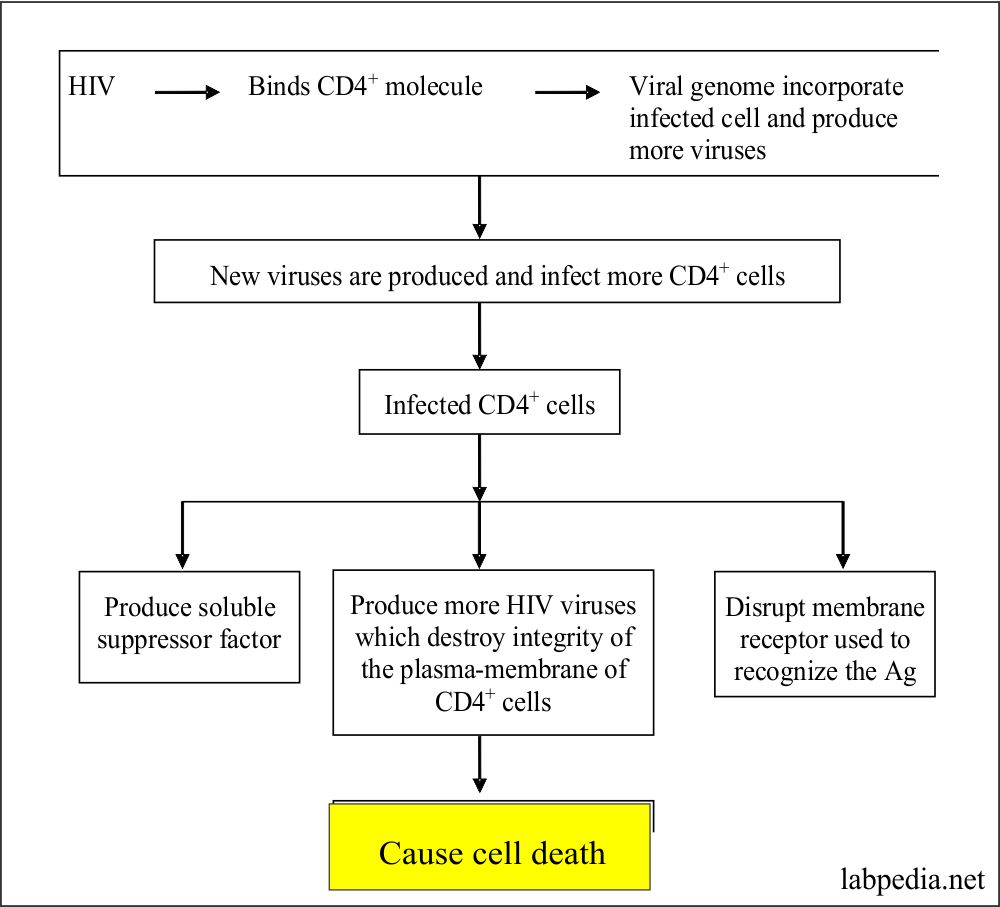
Destruction of the Immune System
- HIV leads to the destruction of the host immune system, which can be summarized as follows:
HIV Infected Cell:
- Can produce lymphotoxin and kill other CD4+
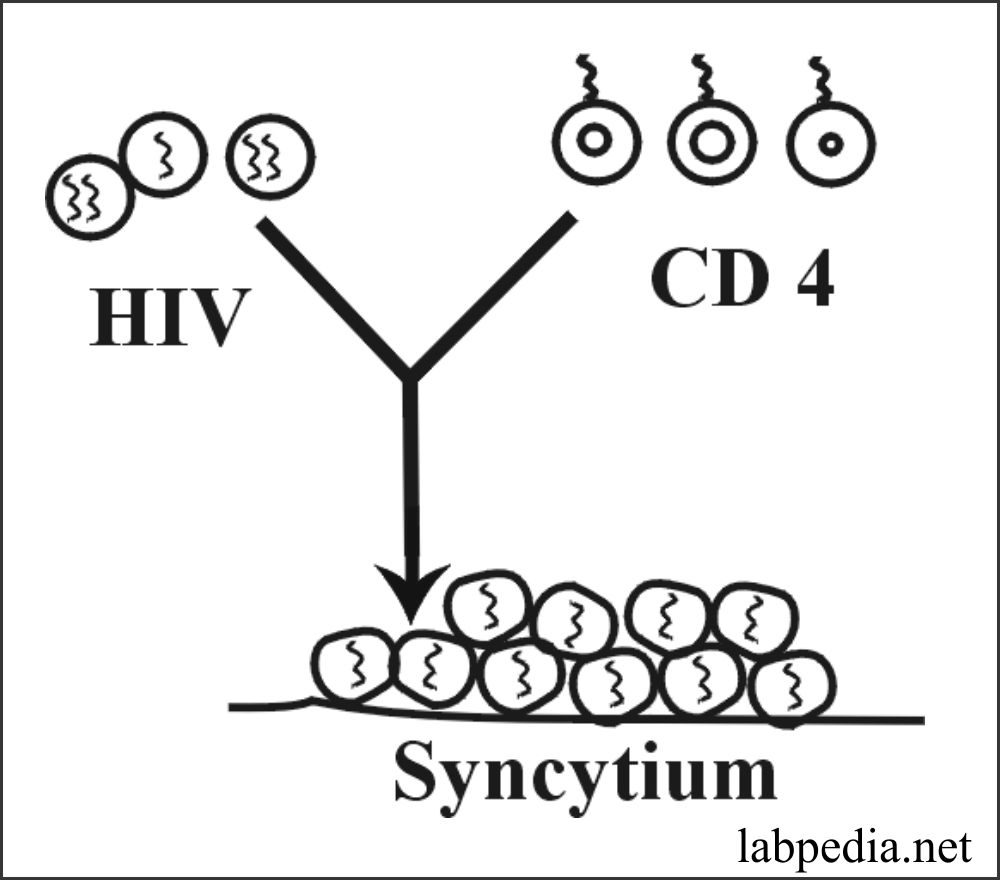
- It can fuse with other cells and make syncytium, which may be up to 100 non-infected cells. Then there is the death of the entire unit.
- There may be direct cell-to-cell contact and transmission.
HIV-as a Cytopathic Virus:
It is believed that the HIV-infection of CD4+ T-lymphocytes cell lines can lead to cell death. There are two mechanisms for this cell death.
- Several viral particles budding simultaneously can fuse with CD4+ molecules on the same cell surface, destroying membrane integrity in “auto-fusion.”
- This is based on observation in vitro-where infected cells fuse to form large, multinucleated giant cell syncytia that have markedly reduced half-life compared to intact cells.
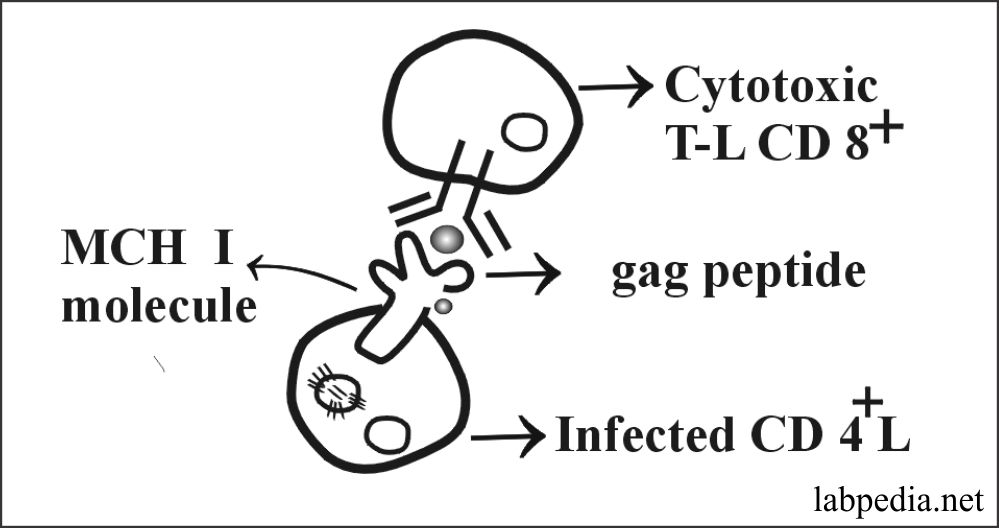
Cytotoxic Responses to HIV-Infected Cells:
CD8+ T-lymphocytes can destroy target cells expressing autologous class-I MHC molecules presenting antigen P24, gag peptide, and env-and pol-derived peptides.
These cells are important in protection against HIV-infection.
Major Immunologic Features:
- There is lymphopenia, which is selective of CD4+ T-lymphocytes. In the terminal phase, there is a total loss of CD4+.
- CD8+ cells are not affected.
- The cytopathic effect is more on CD4+ T-lymphocytes and monocytes relatively refractory.
- CD4+: CD8+ = Normal 2:1 is changed to 0.5:1.
Laboratory Diagnosis:
Two or more findings are needed to suspect HIV. If sign and symptoms persist for more than 3 months like:
- Pyrexia more than 38oC.
- History of chronic diarrhea.
- Weight loss of more than 10%.
- Malaise and lethargy.
- PGL.
- Night sweating.
- Oral candidiasis.
- Hairy leukoplakia.
- Herpes zoster infection.
HIV diagnosis has to be confirmed by laboratory findings.
- ELIZA: Confirmatory tests like HIV-virus or antibodies. Elisa may detect in patient serum specific viral antigen.
- The Western blot technique may further confirm this for the HIV antibody. Western blot, the method that can be used to detect HIV-antigen.
- In the case of acute infection-HIV-1 RNA, quantitation (By PCR) may be helpful.
- Quantitation of lymphocytes (CD4+ T-L), This can be done by flow cytometry.
Other supportive tests are:
- There is leucopenia.
- There is anemia.
- There may be thrombocytopenia.
- There is an immunological abnormality.
- There is raised ESR.
- There is cutaneous anergy.
Direct evidence of HIV infection
- Direct isolation of virus by PCR.
- Indirect detection of the antibody against HIV-antigen.
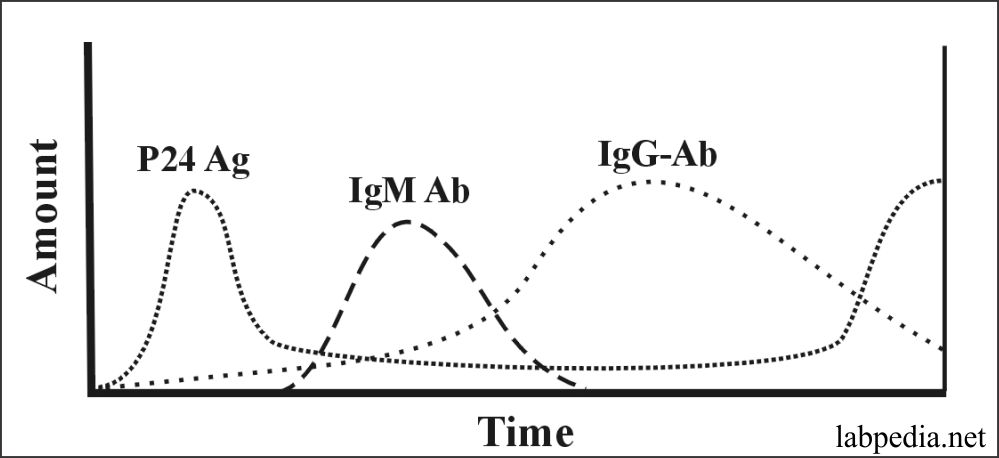
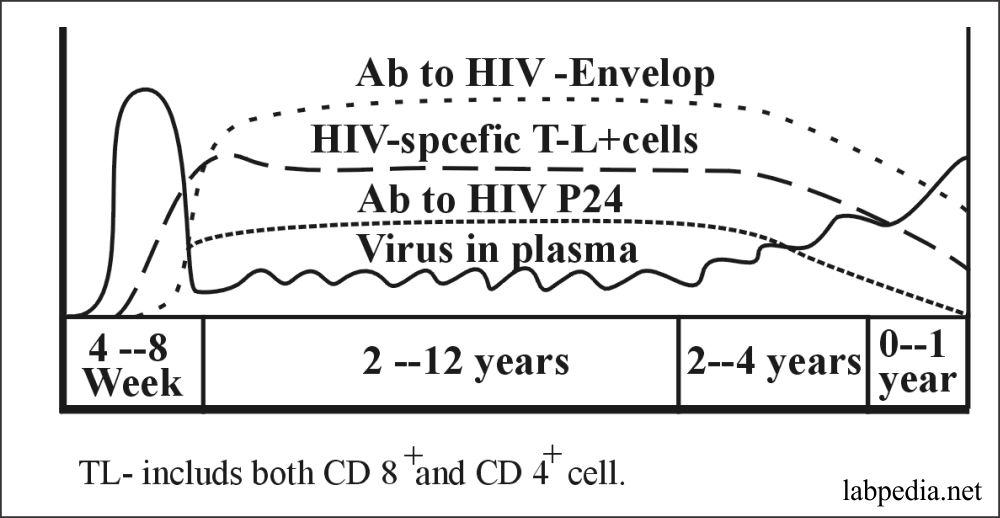
Fig 162: Typical Serological Profile of HIV
The following diagram shows the situation of the level of virus and antibody against the virus antigen. It also shows the state of CD8+ cytotoxic cells.
Summary of the HIV infection:
- ELISA for the anti-HIV I/II.
- Sensitivity is 99%.
- Antibodies to HIV are detected within 6 to 8 weeks of infection.
- p24 protein is detected by 2 to 3 weeks of infection.
- Western blot is the confirmatory test.
- CDC has defined a positive HIV-Western blot test in the presence of any of the following two bands:
- Band for p24.
- Band for gp41.
- Band for gp120/160
- If no bands, then this test is negative.
- In case of a doubtful test, repeat the test within 6 months.
- CDC has defined a positive HIV-Western blot test in the presence of any of the following two bands:
- CD4+ cell count by flow cytometry.
- This is the earliest index of disease progression.
- This count is monitored at 6 months when the disease is stable.
- CD4+ cell count is done to decide the line of treatment.
- Detection of the proviral DNA is used to confirm the diagnosis.
- This has a sensitivity of 955 and a specificity of 98%.
- Quantitation of the HIV RNA viral load is advised.
- This gives a better prognosis for 10 years than the CD4+ cells count.
- The sensitivity of HIV RNA in acute infection is 100%, but specificity is not 100%.
- PCR for proviral DNA is recommended for neonatal infection.
- Umbilical blood should not be tested.
After acute infection, CD4+ T-lymphocytes start gradually declining. Although in the beginning, CD8+ T-lymphocytes and antibody against viral antigen remains at a high level.
Eventually, the antibody and CD8+ T-lymphocytes also fall, and progressively more HIV-appears in the peripheral blood.
AIDS IN PAKISTAN
UNICEF estimates are HIV positive cases in Pakistan are 24,000- to 150,000 in 2003. There is a 0.1% prevalence rate of HIV in Pakistan among adults between 15 and 49.
Other sources say that there are 2464 reported HIV positive cases and 286 AIDS patients.
AIDS in Multan
- 2 male workers in Dubai gave a history of sex with Indian prostitutes and were HIV-positive.
- One male landlord positive, and he was a frequent visitor to Bangkok.
- Screening of T.B. patients was done, and all were negative.
- Screening of blood donors was done, and all were negative.
HIV-is not destroying because of:
- The outer envelope is detachable, which makes adherence to antibodies difficult.
- There is the potential of change in envelope gp120, so a previously formed antibody is not helpful. Because of the above reason, there is difficulty with the formation of the vaccine.
Treatment
- Drugs-like Zidovudine, Azidothymidine, interfere with reverse transcriptase activity and Dideoxyinosine (DDI) has the same mechanism.
- α-interferon has also been tried with the above drugs.
- Drugs that mimic CD4+ molecule-Recombinant CD4+ molecule have been shown to inhibit HIV-replication in vitro.
- Antimicrobial agents. These are of value in the management of opportunistic infection.
AIDS Outcome
85% mortality for 5 years and may reach 100%.



wonderful insights. nicely explained. Thanks
Thanks for the comments.
Good for learning
Thanks.