Chapter 10: Human Leucocyte Antigen (HLA), Major Histocompatibility complex (MHC)
HUMAN LEUKOCYTES ANTIGEN (HLA)
Introduction and History (Historic Back Ground)
Long time back it was considered that successful blood transfusion is dependant upon the blood grouping of donor and recipient.
Landsteiner in 1931 suggested that these groups are important and involved in a successful transplant acceptance.
later on, the histocompatibility antigens were discovered and it leads to more successful transplantation of the organs.
These are isoantigens called histocompatibility antigens. These are found on the surface of white blood cells, platelets, and most of the fixed tissue of the body. These got importance since these got the importance of tissue transplantation.
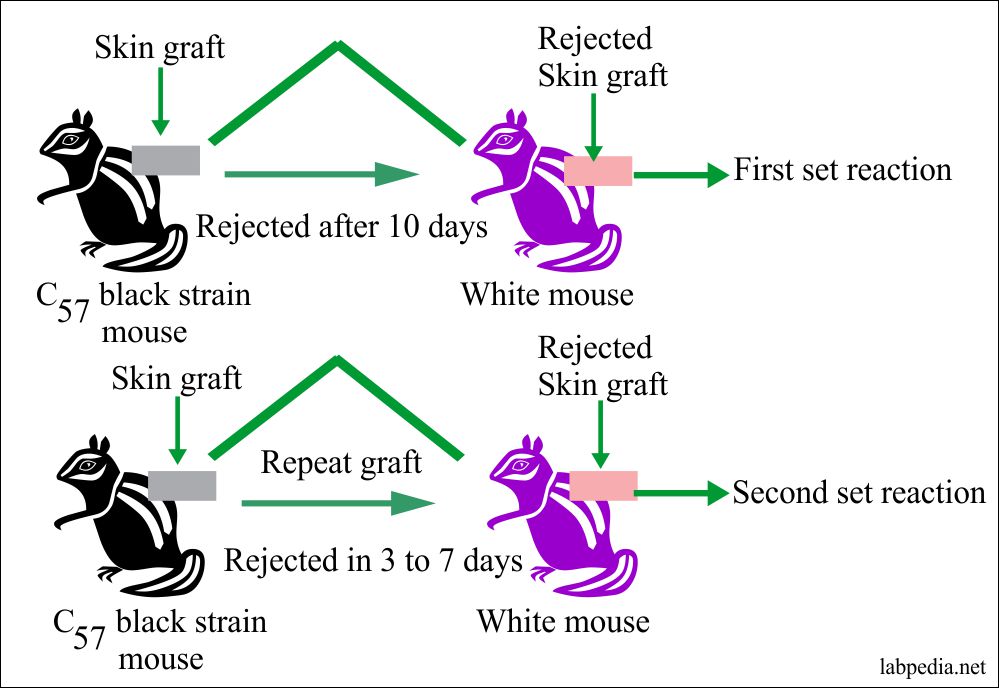
Medawar was attempting to transplant skin graft in world war II in the case of burn soldiers. He noticed that the skin graft of the patient to his own body was successful but when grafted to another person was rejected. On this basis, the experiment was done on mice.
If the mice are already sensitized by the transplantation of tissue from the black strain mice, then in that case skin will have accelerated rejection of the skin graft or any other tissue.
In 1954 the discovery by Dausset, Van Rood, and Payne that the antisera of the multigravida women contain antibodies that agglutinate human leucocytes in spite of ABO compatibility.
The production of the antibodies in these mothers had occurred as a consequence of isoimmunization of pregnancy, during which white cells has entered the mother circulation and stimulated the production of antibodies to the parental antigen on the fetal white cells in a manner analogous to RBCs isoimmunization. Although the disease in the newborn was rare.
Finally, in 1965, Dusset provided a unifying concept and postulated that the genetic basis for the control of 10histocompatibility antigens known at that time was under the control of a single genetic locus.
Gorer gave the idea and identified a group of antigens in mice when matched with the donor and the recipient, markedly improved the survival of the graft.
Major Histocompatibility Complex (MHC) is largely used to show a collection of genes that include those responsible for determining the rejection of transplanted tissue by the immune system.
These antigens are more potent to provoke an immune response, that is why these are called major histocompatibility complex (MHC).
Human Leucocytes Antigen (HLA) is used for MHC gene products involved in antigen recognition by the T-lymphocytes. MHC genes are present on the short arm of chromosome NO: 6.
In human MHC is referred to as human leukocyte antigen (HLA).
Sera of multiple blood transfusion patients and multi-parous females show leuko-agglutinin antibodies, which gives agglutination with white cells and particularly Lymphocytes.
1933 Haldane noticed a reaction to donor cells antigen.
1948 George Snell gave the concept of HLA.
1974 Zinkerangel and Doherty published a series of their classic experiments which helped in understanding the physiological role of the MHC gene in the immune response. They were given Noble Prize in 1966.
MHC or HLA is the most complex immunogenetic system, controlled humans by MHC gene or supergene, which include several loci closely linked on the short arm of chromosome no: 6.
Each of these loci involves numerous alleles, with at least 10 to 40 alleles per locus that control the production of their corresponding antigens.
In the normal person one maternal and one paternal chromosome no: 6 is inherited.
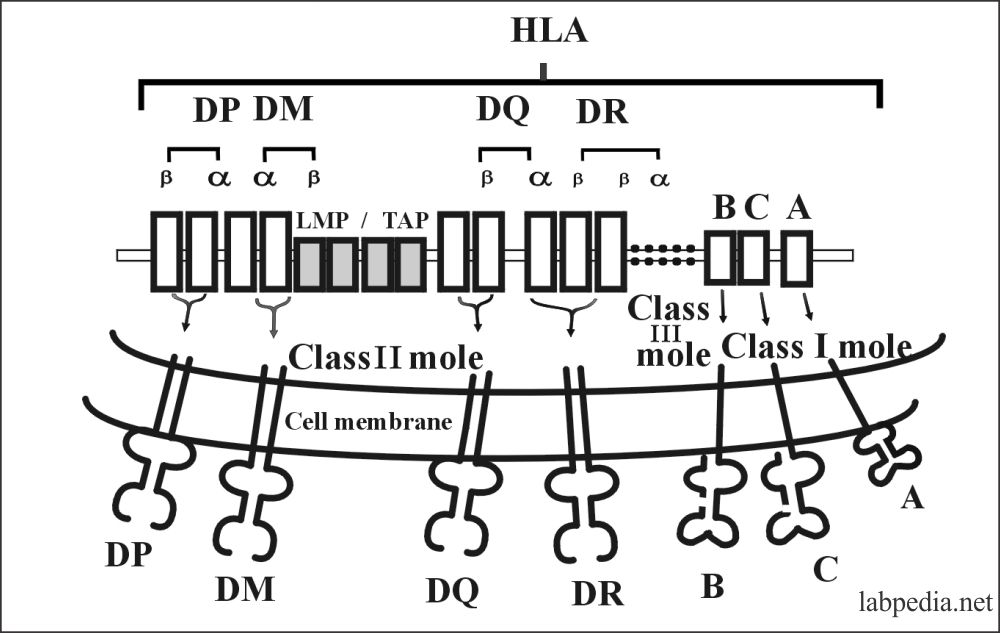
The MHC is divided into 4 major regions:
- HLA – D
- HLA – B
- HLA – C
- HLA – A
- The HLA – A, B, C = Class I molecule = HLA – A, B, and C antigens.
- The HLA – D = Class II molecule = HLA – D antigen.
- HLA – D region divided into HLA-DR, HLA-DC (DQ), HLA-SB (DP).
- Class I and class II molecules are surface membrane protein.
The role of MHC (HLA):
- HLA was originally recognized in the tissue transplantation success.
- Now, this HLA has an important role in our immune system. T-lymphocytes do not recognize directly the antigen but do so when the antigen is presented on the surface of the antigen-presenting cells (APC).
- T-lymphocytes are able to interact with the histocompatibility molecules only if they are genetically identical called MHC restriction.
Organs and tissue transplanted are:
Rejection of tissue transplantation is dependant upon genetic dissimilarity.
- Bone marrow
- Bone matrix
- Liver
- Kidneys
- Skin
- Hairs
- Cardiac valves
- Heart
- Pancreas
- Lungs
- Cornea
Types of tissue transplantation:Type of the graft Tissue types Genetic configuration Definition of the graft tissue Autograft Autologous (from the same individual, from one position to another site) Total identical This is graft in the same individual from his own tissue e.g skin, hairs, and bone. Isograft Isologus (from the genetically similar individual Syngeneic (genetically similar and immunologically compatible) This is a graft from the genetically identical or near-identical individual Allograft (homograft) Homologous (same species but genetically different) Allogeneic (genetically dissimilar but from the same species) This is a graft from genetically different but from the same species Xenograft Heterologous (from the different species) Xenogeneic (genetically different and also the different species) This is a graft from the different species
Comparison of HLA system and Blood group antigens:
| Characteristics | HLA antigens | ABO blood group | Rh blood group |
| Locus Location of genes) | MHC, Linked genes | Single | Complex |
| Polymorphism (multiple forms | Extensive | moderate | Extensive |
| Distribution in the body | WBCs and other tissue | RBCs and other tissue | Only RBCs |
| Clinical significance |
|
|
|
| Lab diagnosis |
|
Serology (ABO blood grouping) | Serology (Rh- blood typing) |
| Treatment (immuno-suppression) |
|
No treatment | Can give specific anti-Rh antibody (Rhogam) |
The degree of immunogenicity in the transplanted tissue:
| Degree of immunogenicity | Organs for transplantation |
| Most immunogenic organs |
|
| Least immunogenic tissue |
|
MHC CLASS I MOLECULE (HLA- antigen)
MHC I molecule is coded by three closely linked loci.
MHC molecules are designated by the capital letter A, B, and C and can be written as:
- HLA- A
- HLA – B
- HLA – C
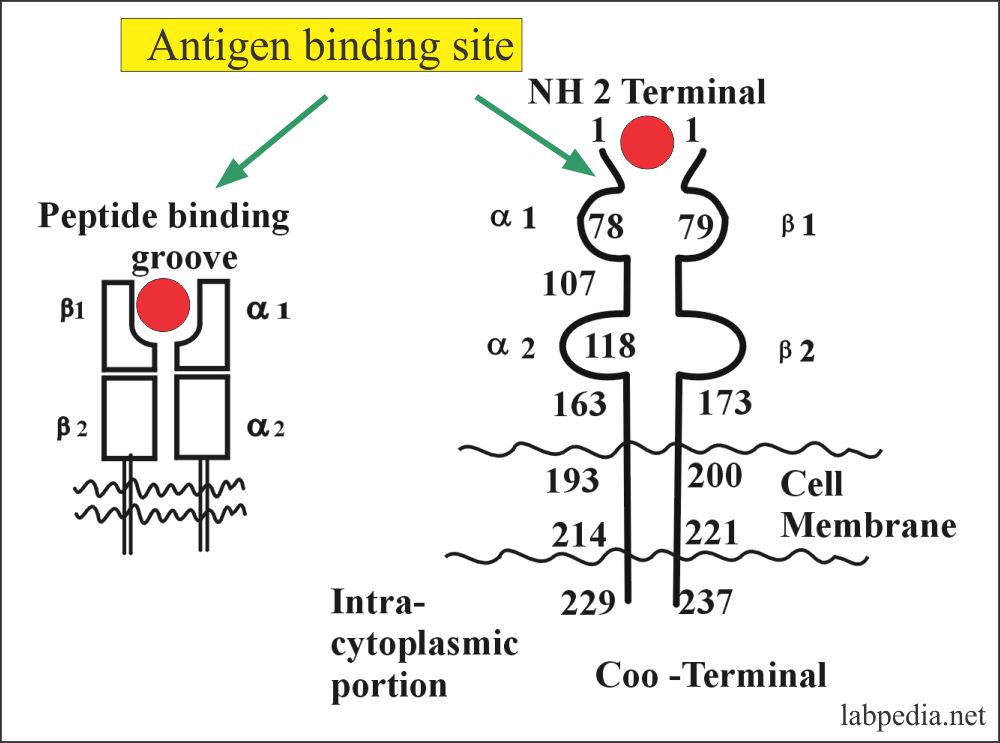
Structure
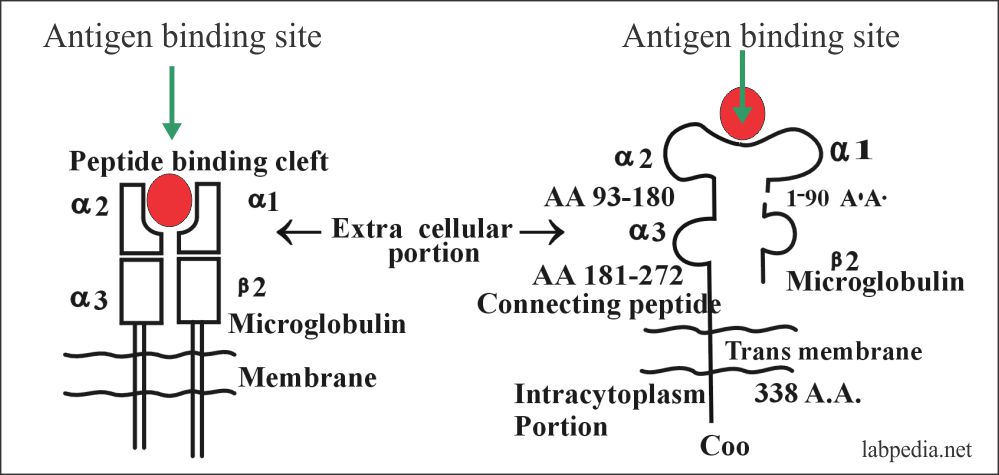
It is a transmembrane glycoprotein (glycosylated heavy chain) and consists of three α- chains with a molecular weight of 45000 and 338 amino acids. The α-chain is linked to β-microglobulin (12 kD). These chains are linked by a disulfide bond and it has four portions as:
- Trans-membrane portion. It consists of 25 amino acids and it crosses the lipid layers of the cells. This is predominantly hydrophobic.
- Extracellular domain consists of 3 α-chains, α1 (N-terminal), α2, and α3. These three extracellular domain compromises 90 amino acid and can be cleaved from the surface with proteolytic enzyme papain.
- α2 and α3 both have intrachain disulfide bonds enclosing loops of 63 and 86 amino acids respectively.
- α3 domain is structurally homologous to the immunoglobulins C domain and contains a site that interacts with CD8+ on cytotoxic T-lymphocytes.
- Connecting peptide.
- Intracytoplasmic portion. This is a hydrophilic domain consist of 30 to 40 amino acids.
- β-microglobulin is non-polymorphic in humans. It has the structure of the immunoglobulin constant region domain.
- β-microglobulin is essential for the expression of all class I molecule at the cell surface.
- The extracellular portion of the α-chain has a groove or cleft where foreign peptide binds to the MHC molecule for the presentation to CD8+ T-lymphocytes.
- In summary MHC class I molecule binds to peptide-like viral antigen.
Distribution of MHC-I molecule
The class-I molecule is virtually present on all nucleated cells including platelet and spermatozoa and body fluids. The following table shows the subclasses (Haplotypes) of HLA.
| HLA Type | Subclass (Haplotype) |
| HLA-A | 24 |
| HLA-B | 50 |
| HLA-C | 8 |
Table XV – HLA subclasses (Haplotypes)
Importance of HLA Class-I Molecule (MHC I molecule)
- It is 1% of the total membrane proteins.
- It is a strong antigen for transplantation rejection.
- It has an important role in CMI (Cell-mediated immunity).
- The function of class I molecule is to present antigens that have originated inside the cell, like viral peptides.
- It has MHC class I restriction for activation of CD8+ cells.
- MHC class I molecule regulate the interaction between cytolytic T-L and target cells.
- Peptide grove holds an antigen for presentation to T-cells (CD8+ cells) TCR.
- Cytotoxic T- L directed against class I antigens are inhibited by CD8+ cells.
- Cytotoxic T- L directed against class II antigens are inhibited by CD4+ cells.
MHC CLASS-II MOLECULE (HLA-antigen)
- MHC II class molecules are coded in the HLA-D region, where there are three subregions DP, DQ, and DR.
- These are different in many respects from the MHC I molecule.
- These are also membrane glycoproteins.
Structure
It is bimolecular protein consists of a heavy (α) and light (β) glycoprotein chain.
- α-chain: Molecular weight is 34000 and consists of 229 amino acids.
- β-chain: Molecular weight is 29000 and consists of 237 amino acids.
- There is evidence that the structure of (α) and (β) chains have the overall same structure.
It has four parts like the class I molecule:
- The extracellular portion consists of two domains of 2 (α) and 2 (β). These are similar to the class I (α3) domains, possessing the structural characteristics of the immunoglobulins constant domain.
- α1, α2, and β1 domains are N-glycosylated, while β2 is not.
- The β2 domain contains a binding site for CD4+ and class II molecule on antigen-presenting cells (APC).
- α2 and β2 domains are similar to class I α3 domain, possessing the structural characteristics of immunoglobulin constant domains.
- β1 domain contains a disulfide bond generating 64 amino acids loop.
- Connecting peptide
- Trans-membrane
- Intracytoplasmic portion.
MHC Class-II Molecule location on the cells
- It is present on the antigen-presenting cell (APC), Monocytes, B-lymphocytes. Spermatozoa, some epithelial cells, and some activated T-lymphocytes.
- MHC class II molecule has a more open groove than the class I molecule.
Importance of MHC class II molecule:
- Class II molecules restrict the activity of the regulatory T-L (helper, suppressor).
- Class II molecules regulate the interaction between helper cells and the antigen-presenting cells (APC).
- Peptide grove of the Class II molecules binds antigen and presents to TCR of T-lymphocytes (CD4+) and this is called MHC II restriction.
Subclasses (Haplotypes) of Class-II Molecules are:
| HLA Class-II Type | Subclass (Haplotypes) |
| HLA-D | 10 |
| HLA-DQ | 9 |
| HLA-DP | 6 |
| HLA-DR | 20 |
Table XVI – HLA Class-II subclasses (Haplotypes)
HLA system expression on the different cells and tissue:
| Degree of expression | HLA class 1 molecule |
| Not expressed on the surface of: |
|
| Weakly expressed on the surface of: |
|
| The variable expression on the surface of: |
|
| Expressed on the surface of: |
|
| HLA II molecule | |
| Not expressed on the surface of: |
|
| Expressed on the surface of: |
|
| HLA-DR | |
| Expressed on the surface of: |
|
| HLA-DQ | |
| Weakly expressed or absent |
Mixed Lymphocytes Reaction (MLR)
Definition:
The MLR is an assay as a vitro procedure in which leukocytes, from two genetically distinct individuals, are mixed of the same species, are cultured where these are resulting in cell blast transformation, DNA synthesis, and proliferation.
Generation of the MLR occurs as a consequence of the incompatibility of the allogenic determinants which are expressed on the surface of the cell population and which are encoded by the major histocompatibility complex (MHC).
Procedure:
- In this procedure, donor cells and recipient cells are mixed in a culture medium where Class-II molecule was identified as a class D by mixed lymphocytic reaction (MLR).
- T-lymphocytes from one individual are mixed and cultured with lymphocytes from the other individual.
- Donor Lymphocytes and Recipient Lymphocytes in culture medium will show:-
- Cell proliferation and division = If Ags are different (when individuals find different MHC molecules).
- No proliferation = If Ags are identical (when MHC molecules are identical to each other).
- This test is done in two ways:
- Two- way test when both individuals cells can proliferate.
- One-way test when only one individual cell can proliferate while the other individual cells are inactivated by irradiation.
Use of MLR:
- To detect the alloreactive T -lymphocytes and histocompatibility.
- Used for selection of donors for the bone marrow transplant.
- For typing of the HLA-D antigens.
- For the selection of donor for the living-related renal allotransplantation.
- With mixed lymphocytic reaction Hyperacute rejection can be prevented.
- Used for diagnosis of immune deficiency diseases.
Class-III Molecule
- Class III molecules bear no clear relation to class I and Class II molecule aside from their genetic linkage.
- These are present in soluble form and are not immunogenic. So these are not important in tissue transplantation.
- Class III molecules are involved in immunologic reactions because they represent the complement components that are involved in the complement pathway.
SIGNIFICANCE OF HLA SYSTEM
- Tissue transplantation
HLA system has a major role in the success of tissue transplantation. There is a humoral and cell-mediated response. When there is a close similarity in class I and II of donor and recipient Ag typing that will lead to a successful transplant.
- Paternity problems
HLA typing of parents and the disputed child may be helpful to confirm the real parentage.
- Association with diseases
There are so many diseases which are common in the same HLA group e.g.
- B-27: Acute anterior uveitis, Ankylosing spondylitis, Postgonococcal arthritis.
- BR3: AIDS, Sjogren syndrome, and Chronic Active hepatitis.
- DR4: Rheumatoid arthritis and insulin-dependent diabetes mellitus.
HLA antigen associated with diseases:
| Disease | Possible HLA antigen in the patient |
| Reiter’s syndrome | B27 |
| Ankylosing spondylitis | B27 |
| Behcet’s disease | B5 |
| Type 1 diabetes mellitus | DR3 |
| Rheumatoid arthritis | DR4 |
| Chronic lymphatic leukemia | DR5 |
| kaposi’s sarcoma | DR5 |
| Celiac disease | B8 |
| Sjogren’s syndrome | B8 |
| Pemphigus | DR4 |
| Myasthenia gravis | B8 |
| Chronic active hepatitis | B8 |
HLA antigen and its association with diseases:
| Presence of the HLA antigen in the patient |
possible Diseases | Increased risk developing the disease over a lifetime |
| B27 |
|
|
| B8 |
|
|
| DR2 |
|
|
| DR3 |
|
|
| DR4 |
|
|
| DR5 |
|
|
The role of MHC class I molecule and MHC restriction:
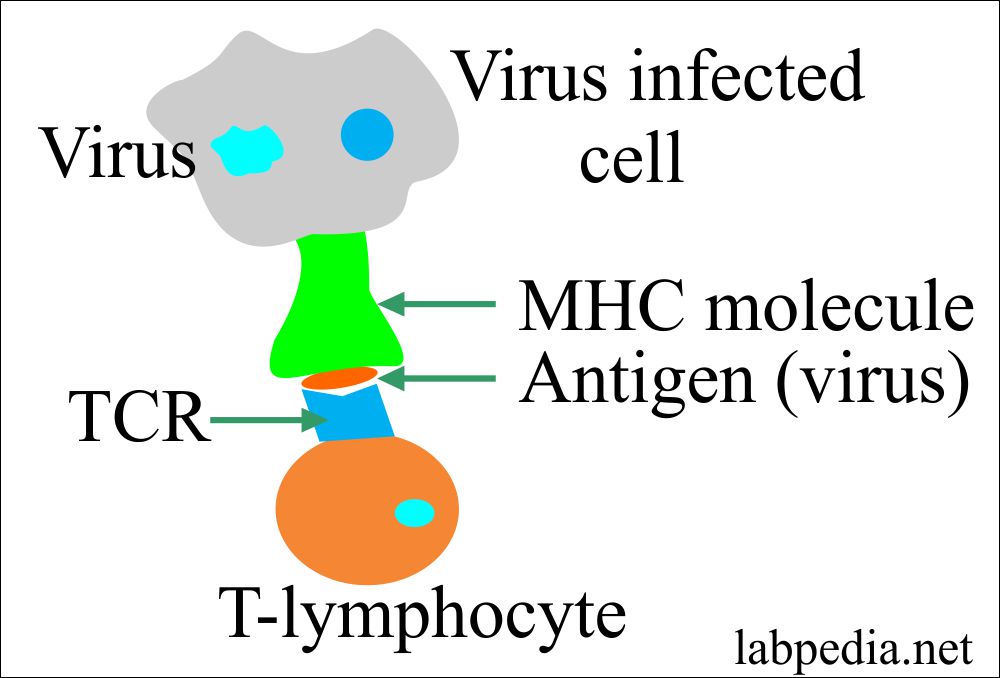
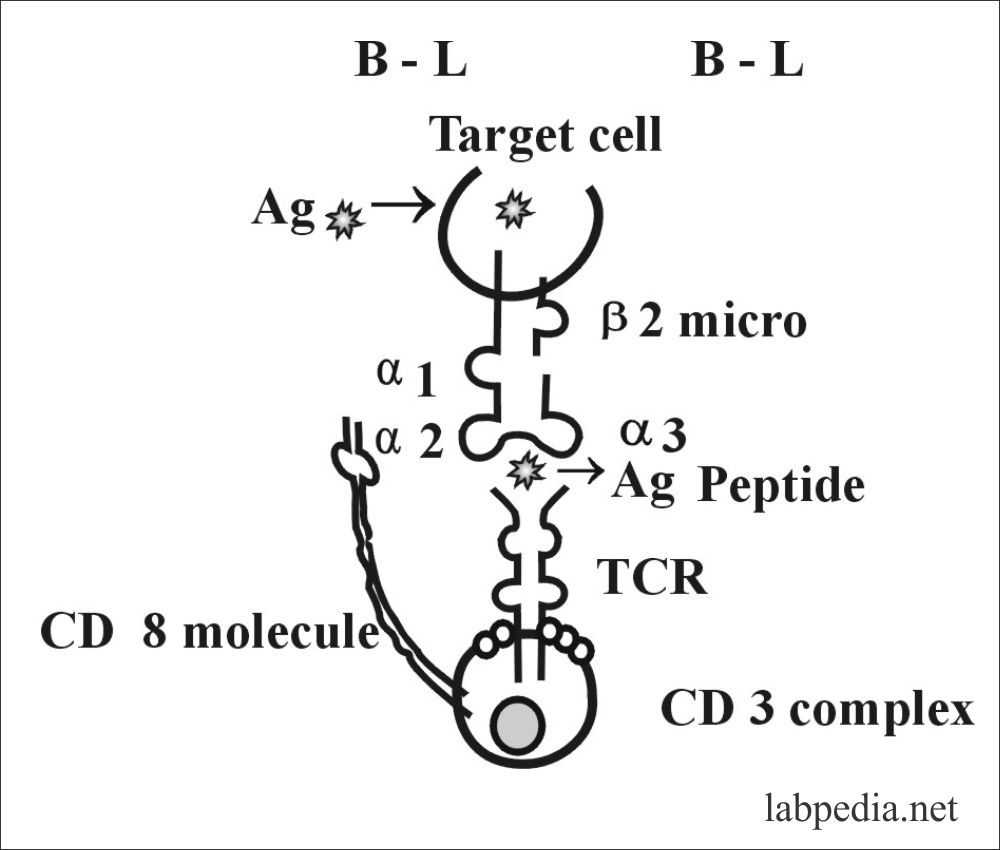
MHC class 1 molecule presents Ag to TCR of CD8+ cells. So CD8+ cell TCR recognizes (Ag + MHC-I).
MHC-I presents peptide form pathogens in the cytosol to CD8+ cells. Mostly these are viruses that cytotoxic CD8+ cells will kill (virus-infected cells).
RBC lake MHC-I molecule. Viruses cannot replicate in RBC because of a lake of MHC I molecule while malarial parasites (Plasmodium) species can live in RBC.
Proteins are broken down by antigen-presenting cells and associates with MHC molecules to activate T-cells.
So CD8+ TCR only recognizes Ag along with MHC-I molecule (Ag + MHC-I).
The Ag is processed in the APC and binds to MHC class-I molecule and presented at the surface to CD8+ cells.
Tc (CD8+) sends lytic signals and cause the death of the target cells. There is the following explanation for cell lysis.
- There may be pore formation due to perforin and cytolysin.
- There may be a release of lymphotoxin (TNF-β).
- There may be a release of proteolytic enzymes like serine Esterase.
So, in this case, TCR of CD8+ recognizes = Ag along with – MHC class I molecule OR
TCR + CD8 = Ag + MHC I molecule
Role of CD 8+ cells:
CD8+ cell activation restricted to MHC-I molecule and these CD8+ Tc cells kill the target cells particularly virus-infected cells and other cells like cancer cells.
CD8+ Tc cells are activated by endogenously derived peptides presented by class-I molecule.
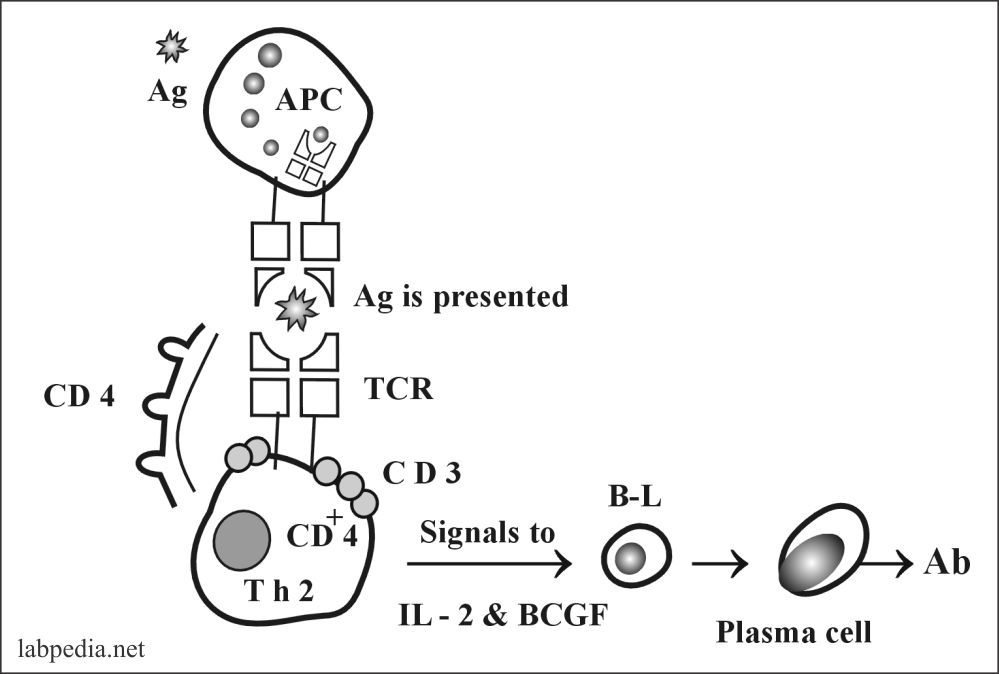
Role of HLA Class-II Molecule and MHC restriction:
Any antigen when after processing by APC and is presented on the surface along with MHC-II molecule is recognized by TCR of CD4+ cells.
CD4+ TCR = Antigen + MHC II
TCR of CD4+ cell is a recognition unit for antigen along with MHC Class-II molecule. So the response to a given antigen is restricted to MHC class-II molecule.
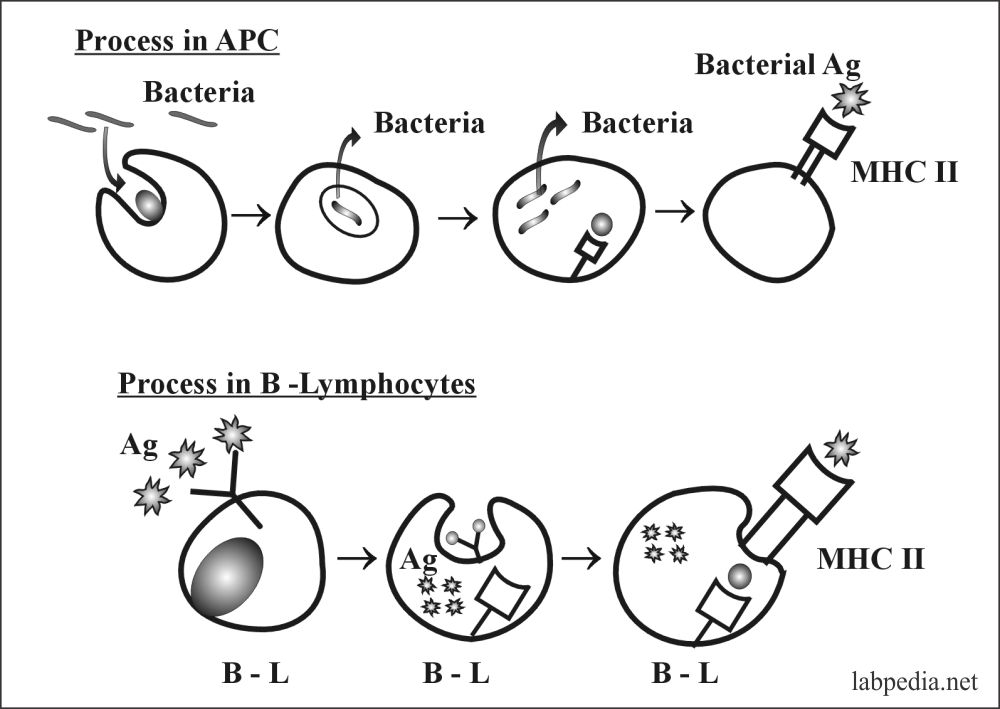
CD4+T cells are activated by peptides that are derived from exogenous proteins which are internalized and processed in APC and presented bound to MHC class II molecule on the surface of APC.
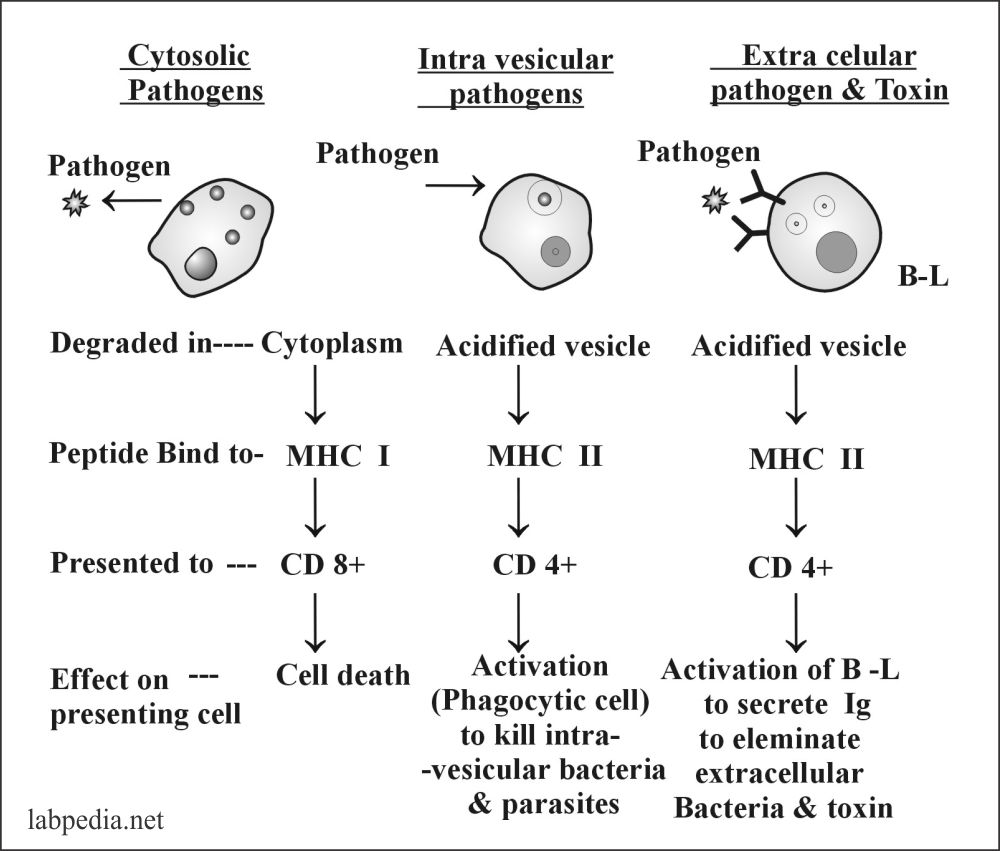
The role of MHC Class-II molecules can be further clarified by the following diagram.
The process in APC showed as follows where Ag is internalized and after processing, presented along with MHC-II molecule.
TCR + CD4+ = Ag + MHC-II
So the response to given Ag is restricted by MHC-II molecule.
Distribution of MHC molecules on various cells:
Type of Cell |
MHC-I | MHC-II |
| T-L | +++ | – |
| B-L | +++ | +++ |
| Macrophagic cells | +++ | ++ |
| Other APC (Langerhan’s cell) | +++ | +++ |
| Epithelial cells of the thymus | + | +++ |
| Neutrophil | +++ | – |
| Hepatocytes | + | – |
| Kidney | + | – |
| Brain | + | – |
| RBC | – | – |
Self Education
MHC system also helps in self-education of self-antigen so self reacting clones of lymphocytes are deleted or made anergic. During the developmental stages of lymphoid cells in the fetus.
The following figure shows the role of Lymphocytes for different types of pathogens and the function of MHC molecules.
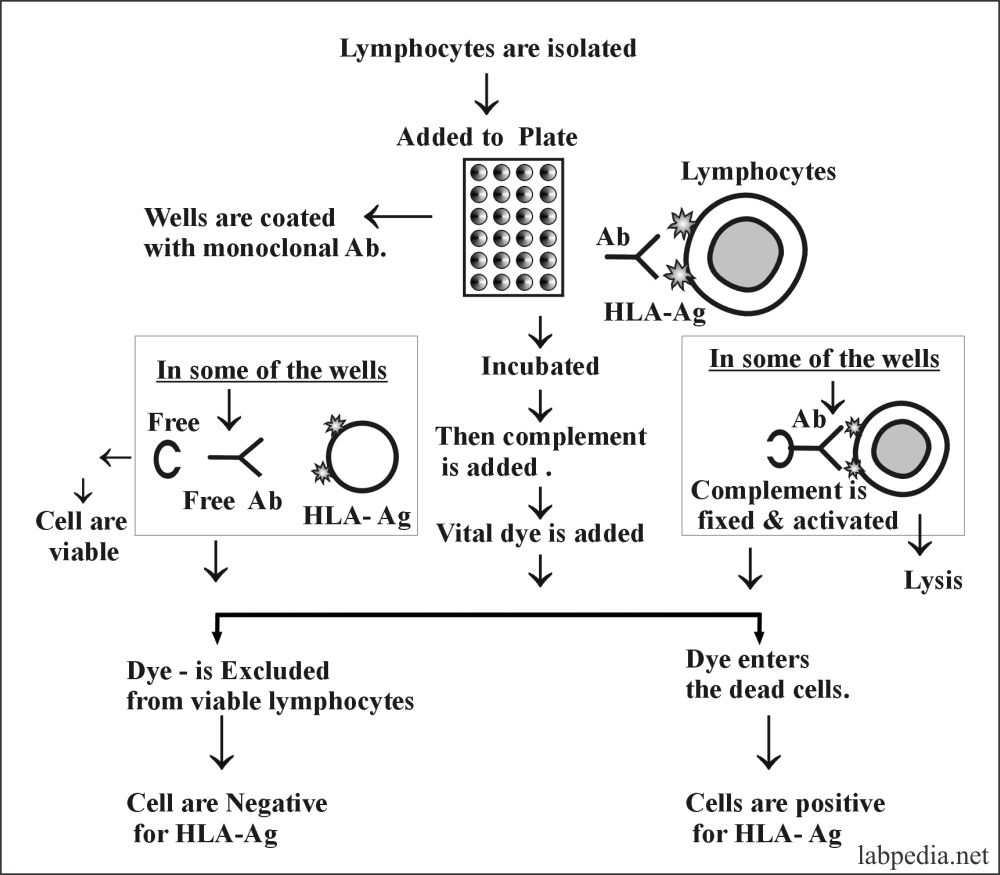
Typing of HLA
The tying of the HLA molecule is based on microcytotoxicity. Now a days monoclonal Ab coated plates are available in the market, which has antibody-coated wells and this is cheap and easy to perform.
The following are the steps to perform HLA typing shown diagrammatically.
Using the commercially available kits HLA, typing of the Donor and Recipient blood can be performed easily.
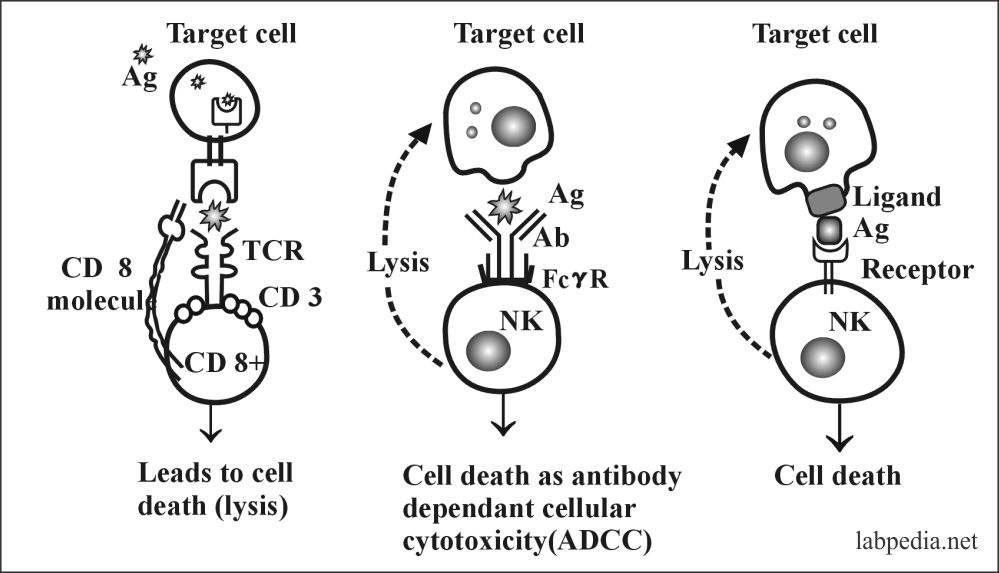
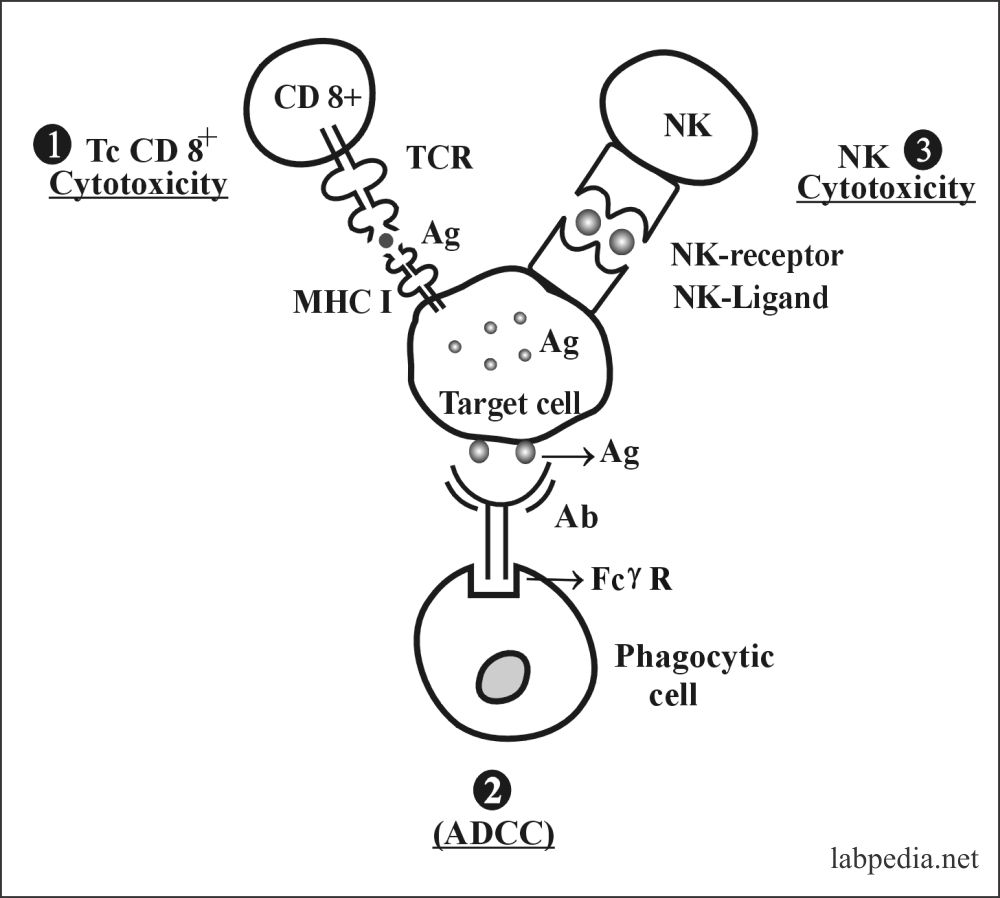
Summary of Process of Lysis of Target Cells
The cells lysis can take place by:
- CD8+ Tc
- Natural killer cells (ADCC)
- Natural killer cells (by ligand)
The following diagram shows that the infected target cell can be destroyed in three different ways as follows.