Dubin-Johnson Syndrome, Diagnosis
Dubin-Johnson Syndrome
What sample is needed for Dubin-Johnson Syndrome?
- Blood is needed to get the serum.
- A random sample can be taken.
How will you define Dubin-Johnson syndrome?
- Dubin-Johnson syndrome (DJ) is a benign condition and looks like mild viral hepatitis.
- This is an autosomal recessive disorder.
- It is characterized by mild recurrent jaundice with hepatomegaly.
How will you discuss the pathophysiology of Dubin-Johnson syndrome?
- This is a rare genetic autosomal recessive disorder (chromosome 10q24).
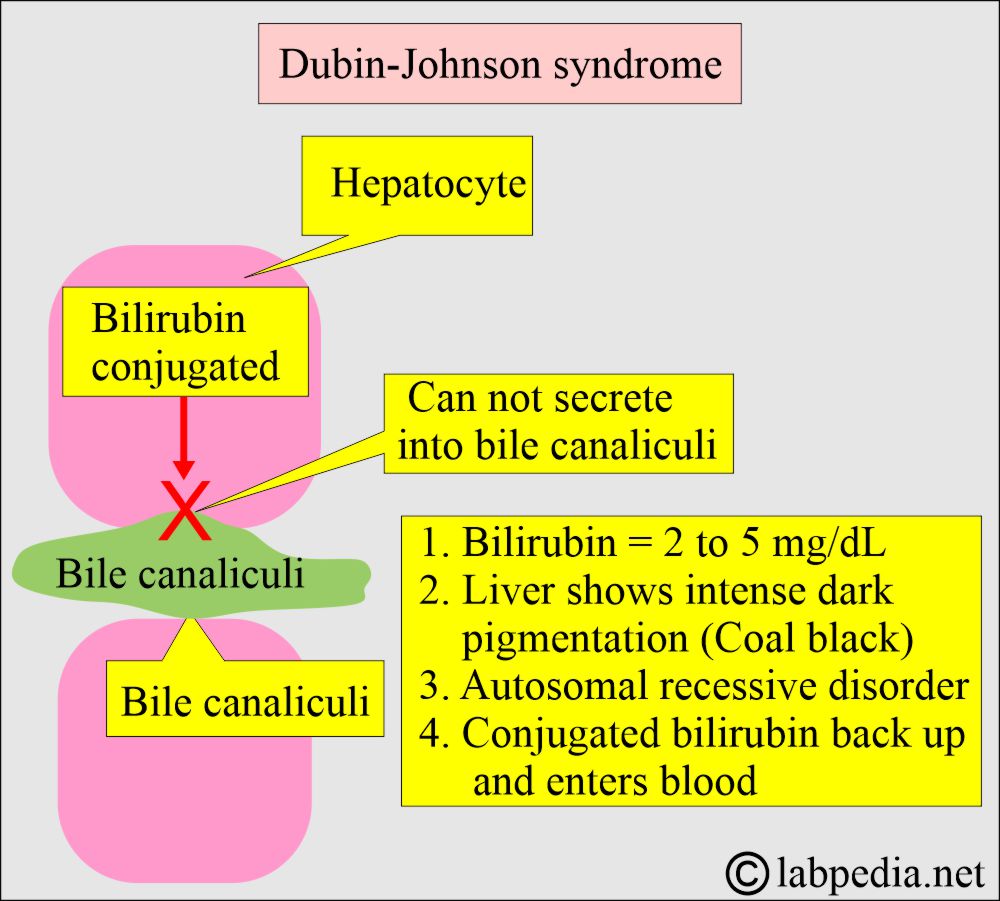
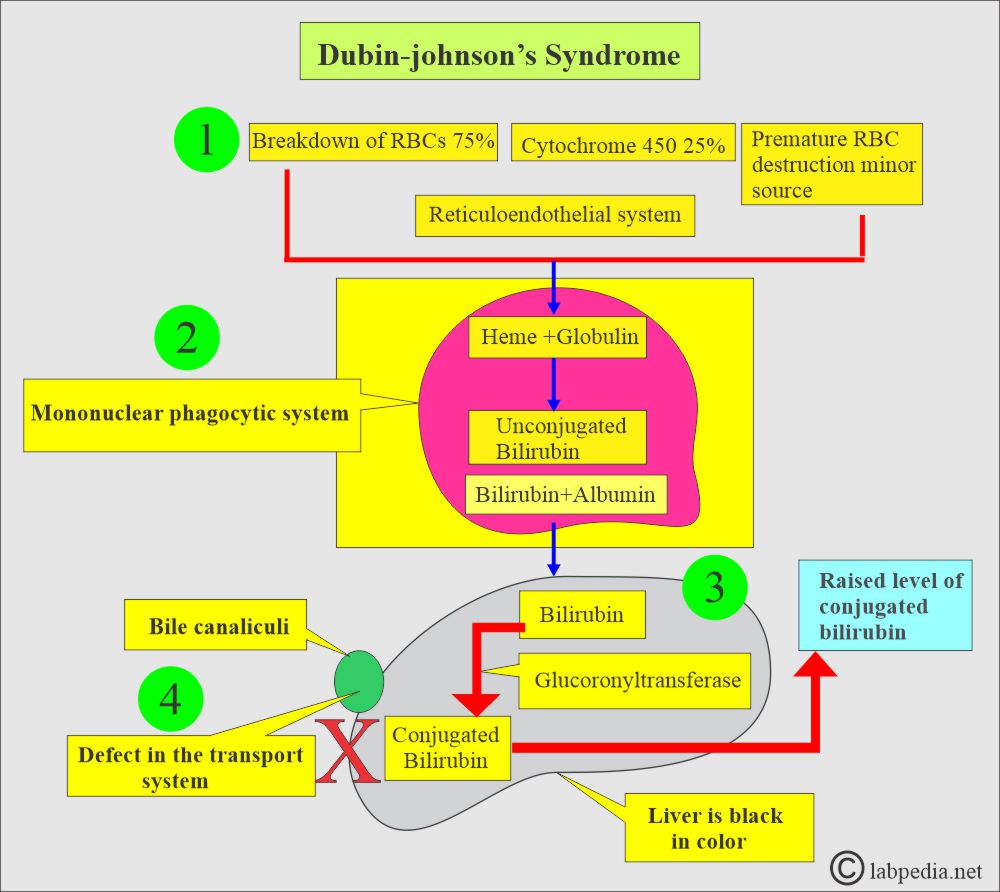
- This is due to the inability to transport bilirubin diglucuronide across the parenchymal hepatic cells into the bile canaliculi.
- This is a defect in canalicular multispecific organic anion transport, associated with increased plasma conjugated bilirubin.
- There is mild jaundice with a total bilirubin of 2 to 5 mg/dL.
- The liver shows intense dark pigmentation due to lipofuscin accumulation (Liver is coal black).
- While the conjugation of bilirubin is regular.
What are the Signs and symptoms of Dubin-Johnson Syndrome?
- There is a yellowness of the eyes and skin due to hyperbilirubinemia.
- Mild jaundice, which may not appear until puberty or adulthood, is the only symptom of Dubin-Johnson syndrome.
- The jaundice is nonpruritic.
- Mild jaundice and may fluctuate.
- Most of the patients are asymptomatic.
- It may become worse in:
- Pregnancy.
- Viral diseases.
- Alcohol intake.
- Stress.
- Oral contraceptives.
- There is no itching and pruritus because the bile level is normal.
What are the Risk factors that increase jaundice?
- Infection.
- Pregnancy.
- Birth control pills.
- Use of alcohol.
- Environmental factors that may affect the liver.
How will you diagnose Dubin-Johnson Syndrome?
- Serum bilirubin is raised (maybe 3 to 10 mg/100 ml). Approximately 50% is indirect bilirubin.
- Mostly, it is conjugated bilirubin (direct bilirubin) that is raised.
- Serum SGOT and SGPT (ALT, AST) are normal.
- Urine contains bile and urobilinogen.
- A liver biopsy shows plenty of yellow or black pigments in the hepatocytes and gives the liver a black appearance.
- Most of the time, a liver biopsy is not needed.
- Cholecystography shows the absence of the gallbladder.
- Urinary coproporphyrin confirms the diagnosis.
Summary of Dubin-Johnson syndrome
| Clinical features | Dubin-Johnson syndrome features |
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
How will you treat Dubin-Johnson Syndrome?
- This is a benign disease and does not need any specific treatment.
- This patient should be given a warning for follow-up in case of pregnancy, oral contraceptives, and any illness that leads to an increase in the bilirubin level.
- Phenobarbitone was used but is not now recommended.
What is the outcome of Dubin-Johnson syndrome?
- The picture is not gloomy and does not shorten the patient’s lifespan.
How will you differentiate from Rotor’s syndrome?
- Both have direct hyperbilirubinemia.
- No liver pigmentation in Rotor’s syndrome.
How will you summarize different types of inherited jaundice?
| Clinical parameters | Unconjugated Hyperbilirubinemia | Conjugated Hyperbilirubinemia | |||
| Gilbert’s disease | Type 1 Criggler-Najjar | Type II Criggler-Najjar syndrome | Rotor’s syndrome | Dubon-Jhonson syndrome | |
| Inherited mode | Autosomal dominant | Autosomal recessive | Autosomal dominant | Autosomal recessive | Autosomal recessive |
| Incidence | <7% of the population | Very rare | Uncommon | Rare | Uncommon |
| Age at onset | In adolescence | In infancy |
|
Early adulthood |
|
| Pathogenesis | Glucoronyl transferase enzyme deficiency (GTE) | GTE decreased | Markedly decrease | Impaired conjugated bilirubin excretion | Impaired conjugated bilirubin excretion |
| Bilirubin level |
|
Mainly indirect | Mainly indirect |
|
|
| Clinical signs/symptoms |
|
|
|
|
|
| Effect of phenobarbitone | Decreased to normal | There is no effect | Marked decrease | —– | —– |
| BSP (Dye excretion) test | May be mildly impaired in <40% of cases | It is absent | _____ | Positive, Initial rapid fall and then rise in 40 to 90 minutes | Positive, Slow clearance, and no rise |
| Oral cholecyctography | Normal | Normal | Normal | Normal | GB is usually not visualized |
| Liver biopsy | Normal | —- | —- | No pigments | Characteristic pigments (Coal black) |
| Treatment | Not needed | There is no treatment | Not needed | ||
Questions and answers:
Question 1: What is the mechanism of Dubin-Johnson Syndrome?
Question 2: What is the color of the liver in Dubin-Johnson Syndrome?

hello,
Im vinoth kambli,
doctor was confirmed for me . i have a dubin johnson syndrome.
problems a matter is im not able to clear medical test for foreighn jobs in any country.
so,please reply….any solutions?
Please read my article.
Hello,
I am Muha,
I have liver function test. I have elevated direct bilirubin (5.9 umol/l) and ALP (311 U/l). All other parameters (ALT, AST, GGT, TP, Albumin and total bilirubin) are normal. Abdominal (liver) ultrasound reveals no abnormalities. I have mild intermittent colic. I am not sure what is going on. My doctor said nothing to worry about. I appreciate if you could help me. Thank you
Have you checked the viral profile (HBV, HCV)? If there is only raised direct bilirubin, then the possibilities are hereditary hyperbilirubinemia. Mostly these are benign conditions. You can try the tab. Phenobarbitone or consult a physician about this drug. It will lower the bilirubin level.
Thank you for your reply. Yes, I have checked for HCV in 2017 and it was negative. I have experienced an elevated ALP since I was 11 (16-year-old now). What is the tab?