Disseminated Intravascular Coagulopathy (DIC), Diagnosis and Treatment
Disseminated Intravascular Coagulopathy (DIC)
What sample is needed for Disseminated Intravascular Coagulopathy (DIC)?
- Collect the blood for PT and PTT.
- Blood samples were collected in sodium citrate as an anticoagulant.
- Immediately do an assay for clotting factors ( coagulation profiles).
- Perform the bleeding time.
- Collect blood for a complete blood examination, particularly for the platelet count.
What are the Indications for Disseminated Intravascular Coagulopathy (DIC)?
- To exclude septicemia.
- Amniotic fluid embolism.
- Retention of the dead fetus.
- Malignant neoplasia.
- In liver cirrhosis.
- Extensive surgery, especially on the liver.
- Severe burn.
- Extensive trauma.
- After the blood transfusion reaction.
How will you define Disseminated Intravascular Coagulopathy (DIC)?
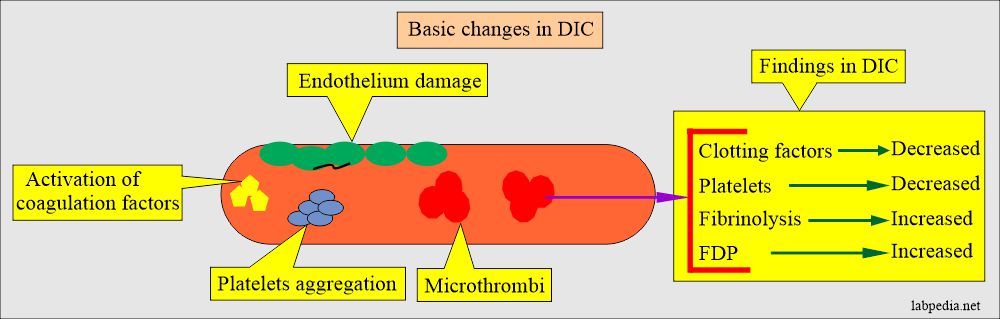
- DIC is an acquired coagulation abnormality where excessive activation of the coagulation factors will show widespread fibrin thrombi in the microcirculation. This process will lead to the following:
- Depletion of the coagulation factors.
- Decreased count of platelets.
- It will cause bleeding and activation of thrombin.
- Thrombosis of small and midsized-sized blood vessels.
Another definition of Disseminated Intravascular Coagulopathy (DIC):
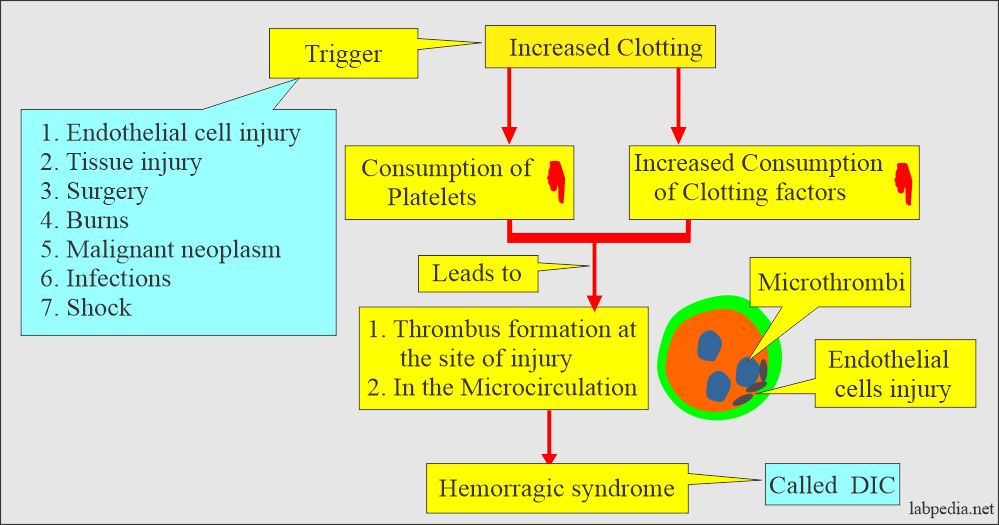
- DIC is uncontrolled activation of the clotting mechanism (factors) that will lead to:
- Widespread thrombi formation.
- Depletion of coagulation factors.
- Decreased platelet count.
- Massive hemorrhage.
- More than one mechanism is often present.
Pathophysiology of Disseminated Intravascular Coagulopathy (DIC)
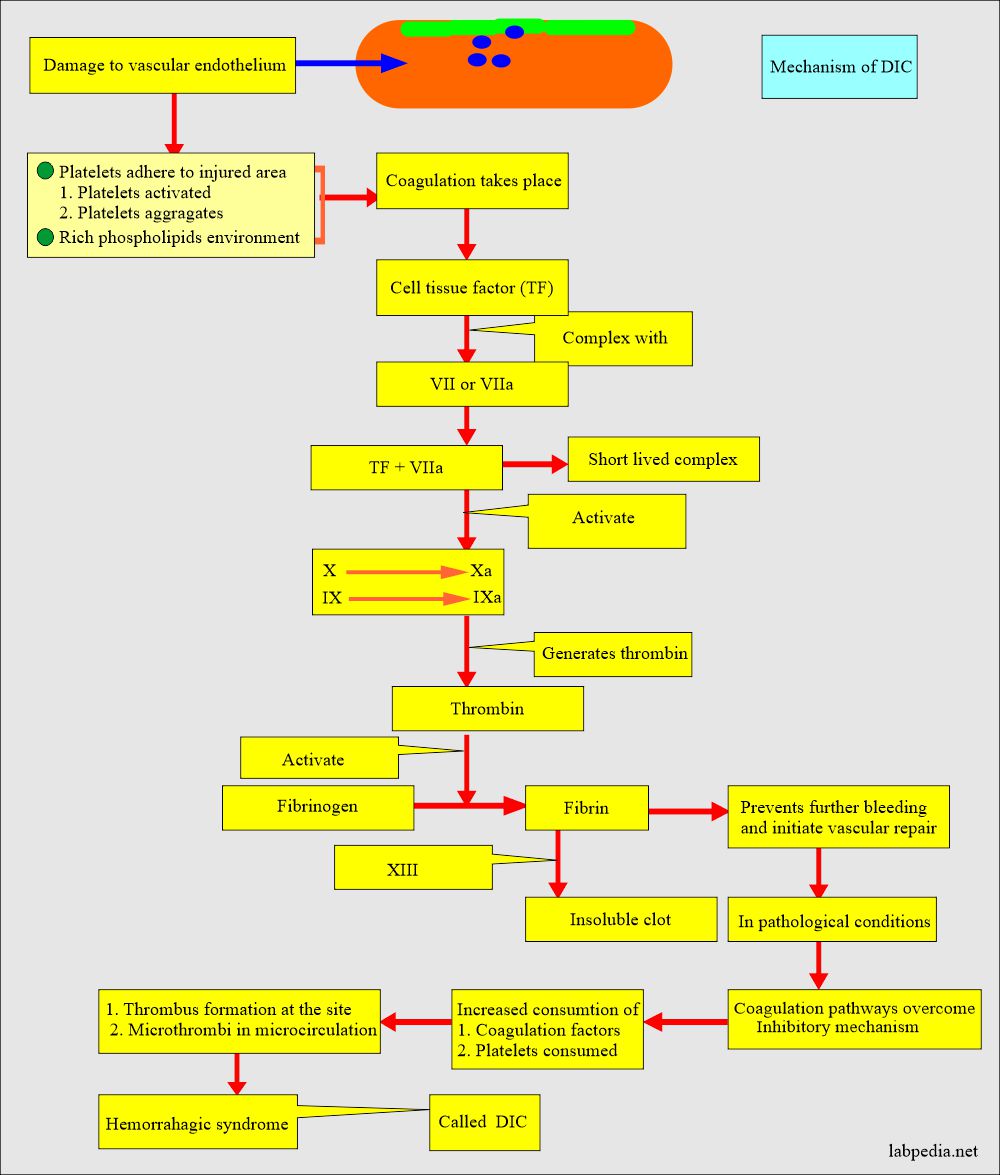
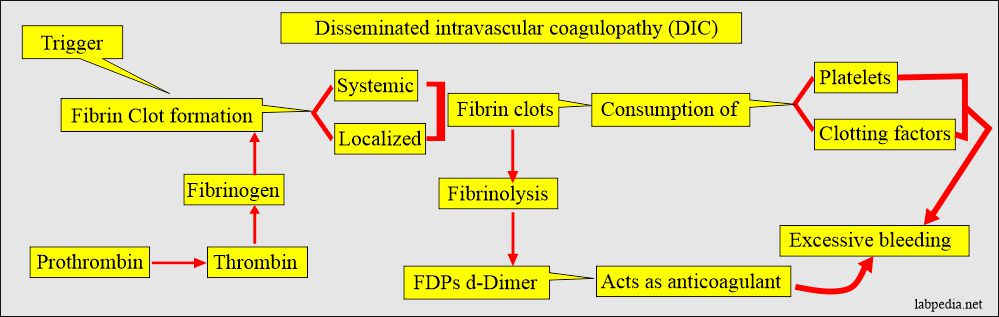
- In DIC, there is inappropriate activation of the clotting system.
- This will lead to systemic or localized fibrin clot formation.
- Due to increased clotting, there is sludging and excessive bleeding because of the consumption of platelets + clotting factors.
- There is increased coagulation, which overcomes the inhibitory mechanism.
- This will lead to thrombus formation at the site and microcirculation, leading to hemorrhagic syndrome.
- This hemorrhagic syndrome is called DIC, defibrination syndrome, or consumptive coagulopathy.
- The fibrinolytic system is activated and breaks the clots + fibrin.
- Fibrinolysis leads to FDP (Fibrin degradation products).
- FDPs increase bleeding tendency.
What is Fibrinogenolysis?
- This may be primary or secondary.
- Primary fibrinogenolysis is rare, and the target is only fibrinogen.
- Secondary fibrinogenolysis is common. It attacks fibrin but also attacks fibrinogen.
How will you diagnose Fibrinogenolysis?
- The platelet count is usually normal.
- Fibrinogen level is decreased.
- The potassium sulfate test is negative, which is positive in DIC.
- Latex test for fibrinogen degradation products (FDP) titer. FDP very markedly increased.
- Euglobulin clot lysis time (minutes) is decreased.
- Factor V is decreased.
- Factor VIII is normal to decrease moderately.
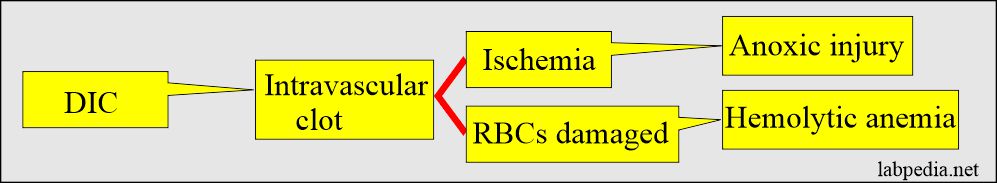
- Intravascular clots lead to microvascular occlusion leads to injury to the organs.
- There may be hemolysis of RBCs by passing through these vessels.
How will you differentiate between Disseminated intravascular coagulation (DIC) and fibrinogenolysis?
| Lab test | Fibrinogenolysis | Acute disseminated intravascular coagulation (DIC) |
|
|
|
How will you classify Disseminated Intravascular Coagulopathy (DIC)?
- Acute DIC (Acute hemorrhagic DIC).
- Chronic DIC (Subacute chronic DIC).
Table: The difference between acute and Chronic DIC:
Lab Tests |
Acute DIC |
Chronic DIC |
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
how will you diagnose Disseminated Intravascular Coagulopathy (DIC)?
- The lab. findings of the DIC reflect direct or indirect excess of thrombin and plasmin generation.
- No single test is diagnostic.
- Indirect tests are the lake for thrombin action, including PT, APTT, and thrombin/reptilase clotting tests.
- The confirmatory test is the demonstration of the fibrin deposition in the biopsy of blood vessels that are involved.
- The following tests are advised to diagnose DIC:
- Platelet count. There is thrombocytopenia.
- There is an increased plasma level of platelets-specific protein (β-thromboglobulin).
- Platelet factor 4.
- Prothrombin time (PT).
- Partial thromboplastin time (PTT).
- Coagulation factor assay.
- Fibrinogen degradation products (FDP).
- Fibrinogen.
- D-dimer.
- Prothrombin fragments.
- The peripheral blood smear shows schistocytes.
- Platelet count. There is thrombocytopenia.
- Immediately perform the following test that will diagnose the DIC.
- PT.
- PTT.
- Platelet count.
- Bleeding time.
What are the causes of Disseminated Intravascular Coagulopathy (DIC)?
- These can be summarized into various groups:
- Infections.
- Trauma with extensive tissue damage.
- Vascular abnormalities.
- Connective tissue diseases.
- Due to toxins like snake bites, etc.
- Pregnancy and obstetrical complications.
- Damage to platelets or RBCs.
- Metastatic neoplasm.
- Broadly, DIC can be caused by:
- Bacterial Septicemia.
- Retention of a dead fetus.
- Amniotic fluid embolism.
- Liver diseases.
- Malignant diseases.
- Extensive surgery on the liver or prostate.
- Heart bypass surgery.
- Extensive trauma.
- Severe burns.
- Transfusion reaction.
What clinical conditions are associated with Disseminated Intravascular Coagulopathy (DIC)?
- Due to Thromboplastin release – Factor VII activation:
- Placental abruption.
- Sepsis.
- Promyelocytic leukemia.
- Retained dead fetus syndrome.
- Amniotic fluid embolus.
- Cardiopulmonary bypass surgery.
- Acute intravascular hemolysis.
- Adenocarcinoma (mucin-producing).
- Trauma.
- Due to Factor X/II activation:
- Acute pancreatitis.
- Snake venom.
- Fat emboli syndrome.
- Liver diseases.
- Due to endothelial cell damage – Factor XII activation:
- Liver diseases.
- Intravascular hemolysis.
- Immune complex diseases.
- Vasculitis.
- Burns.
- Anoxia.
- Acidosis.
- Heatstroke.
Table: Shows the findings of the various tests in Disseminated Intravascular Coagulopathy (DIC):
Tests |
Outcome |
|---|---|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
Laboratory diagnosis of Acute Disseminated Intravascular Coagulopathy (DIC):
| Lab Test | DIC |
|
|
|
|
|
|
| Confirmatory test | |
|
|
|
|
How will you treat Disseminated Intravascular Coagulopathy (DIC)?
- Treatment is two folds:
- Removal of the underlying pathologic cause.
- Maintain the blood volume and hemostatic function.
- There is a transfusion of the packed red blood cells.
- Give fresh frozen plasma.
- Give platelets concentrate.
- Replace missing blood coagulation factors (components).
- The main aim of the DIC treatment is the balancing function to restore the body’s ability to coagulate normally.
Questions and answers:
Question 1: What is the definition of DIC?
Question 2: How will you diagnose acute DIC?