D-Dimer test, Fragment D-dimer, Diagnosis of Disseminated Intravascular Coagulopathy (DIC)
D-dimer test
Which sample is needed for the D-dimer test?
- Citrate plasma is needed.
- It is stable for 8 hours at room temperature. It can be kept at -20 °C for 6 months.
What are the indications for the D-Dimer test?
- This test is done to diagnose DIC (disseminated intravascular coagulopathy).
- It monitors the DIC or hypercoagulable states.
- It can diagnose other thromboembolic disorders (venous thrombosis).
- It can diagnose Pulmonary embolism.
- For the diagnosis of acute myocardial infarction.
- D-dimer may be increased by atrial fibrillation, congestive heart failure, and cirrhosis.
- It monitors anticoagulant therapy.
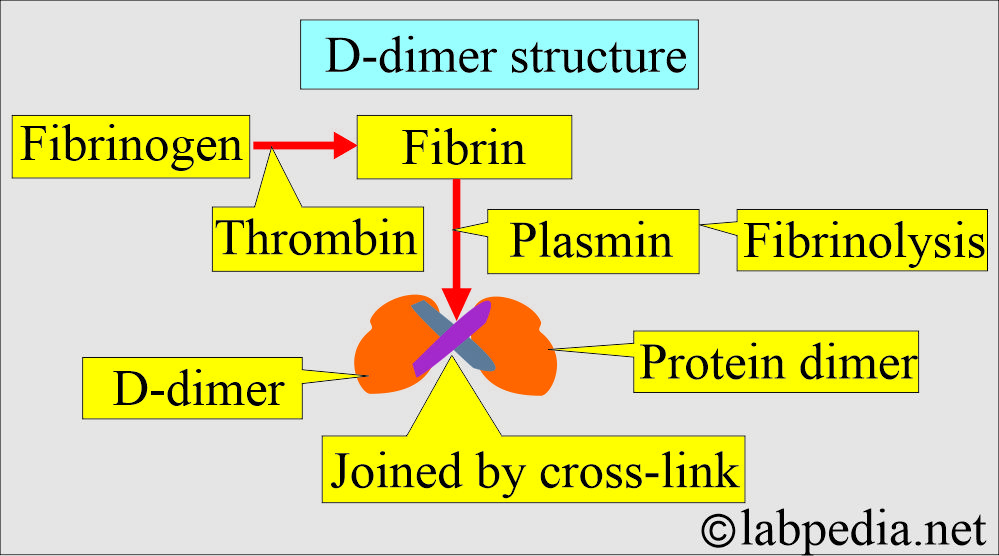
What is the definition of D-dimer?
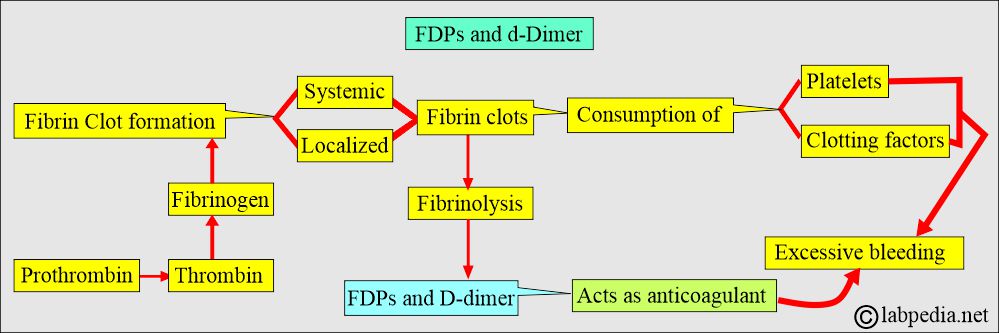
- D-dimer is a fibrin degradation product (FDP) by fibrinolysis.
- Plasmin action on cross-linked fibrin clots produces d-dimers.
- The presence of D-dimer confirms that both thrombin and plasmin have been generated.
- Factor XIII generates a D-dimer by covalently linking the D regions of the fibrin molecule.
- D-dimer assesses both thrombin and plasmin activity.
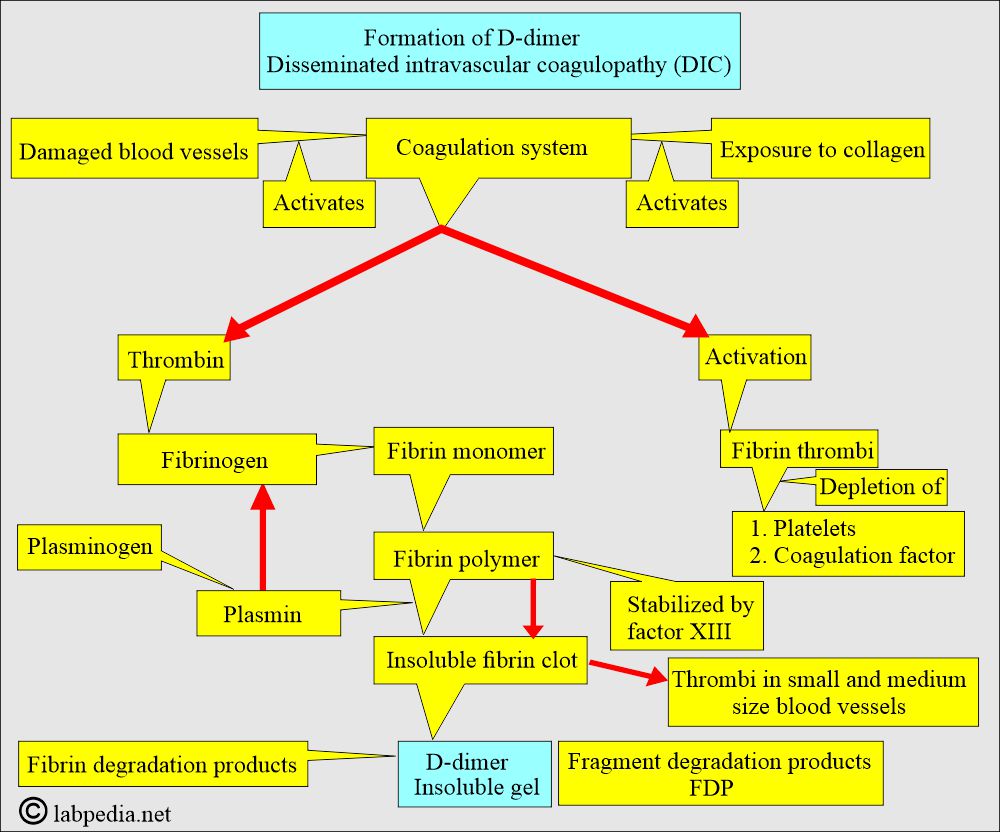
- Damaged blood vessels and exposure to collagen activate both the intrinsic and extrinsic coagulation cascades.
- SO D-dimer is a fibrin degradation product (fragment).
- It is found in the blood as a small protein fragment after fibrin clot degradation (fibrinolysis).
- It consists of 2 D-fragments of the fibrin protein, joined by a cross-link, forming a protein dimer.
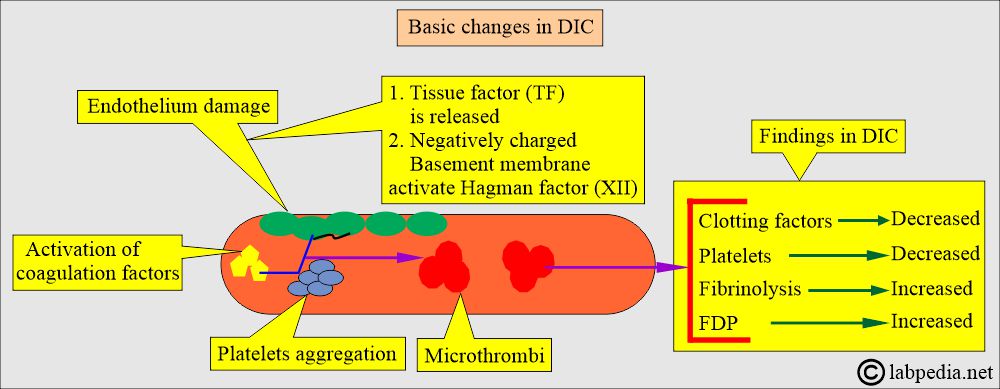
Disseminated intravascular coagulopathy (DIC):
What is the definition of Disseminated Intravascular Coagulopathy (DIC)?
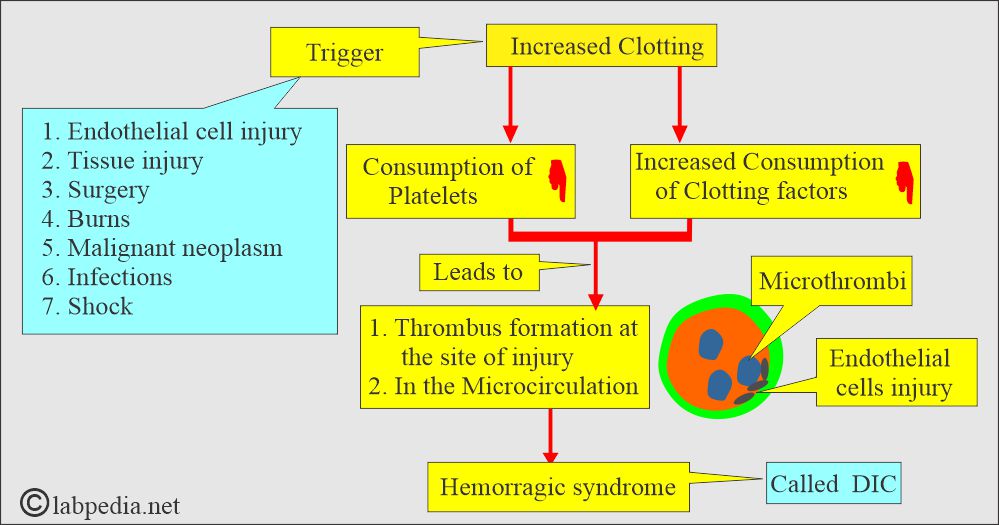
- Briefly, it is a widespread activation of the coagulation system that occurs throughout the blood circulation.
- This is the most serious complication of fibrinolysis in DIC.
- This is also called consumption coagulopathy.
- DIC is an acquired coagulation disorder characterized by excessive systemic activation of the coagulation system, widespread fibrin thrombi in the microcirculation, rapid depletion of platelets and coagulation factors, leading to bleeding.
- There is the activation of thrombin, leading to thrombosis of small and mid-sized vessels.
- Usually, more than one mechanism is at work.
- This is an inappropriate intravascular deposition of fibrin, with consumption of coagulation factors and platelets, which occurs due to many diseases that release procoagulants into circulation, or it may cause widespread endothelial damage and platelet aggregation.
- There is the deposition of microclots in the blood vessels and depletion of the plasma fibrinogen, leading to hemorrhagic syndrome.
What is the pathogenesis of Disseminated Intravascular Coagulopathy (DIC)?
- This is an acquired clinical syndrome caused by increased protease activity in the blood.
- It is the unregulated release of thrombin with the formation of fibrin and increased fibrinolysis.
- This is mainly due to the activity of the coagulation cascade (procoagulants).
- The possible factors that will increase the procoagulant’s activity are:
- Arterial hypotension is accompanied mainly by shock.
- Hypoxemia.
- Acidosis (acidemia).
- Stasis of the capillary blood flow.
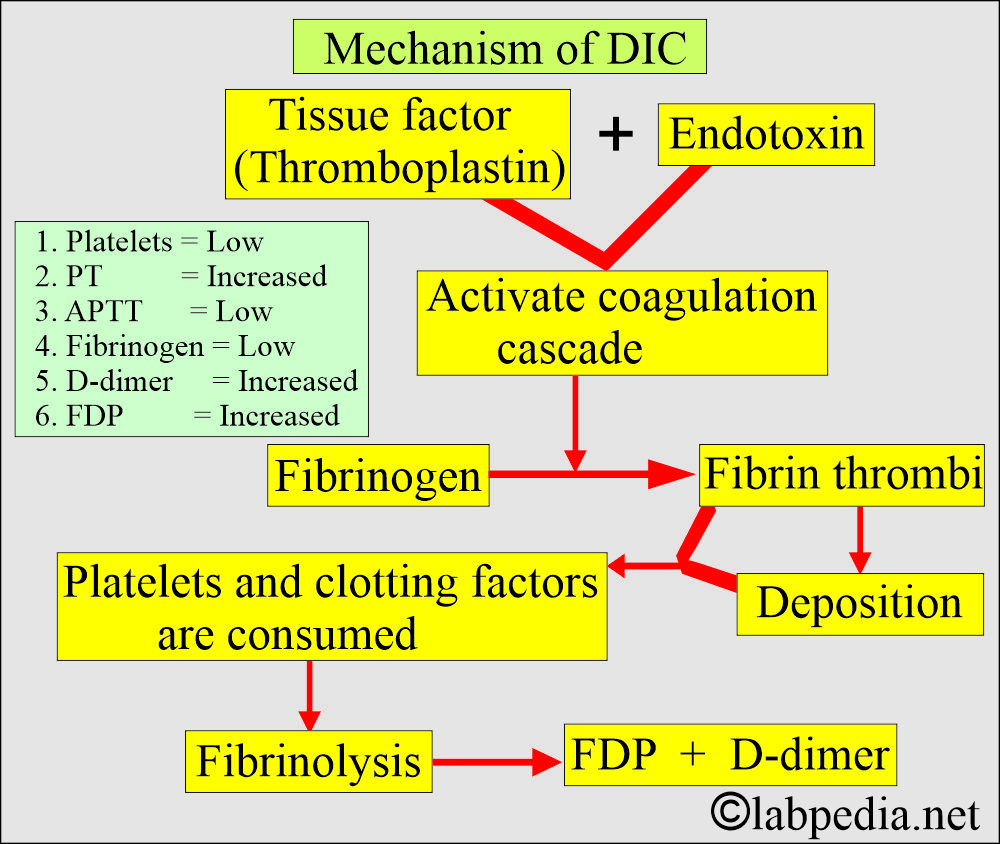
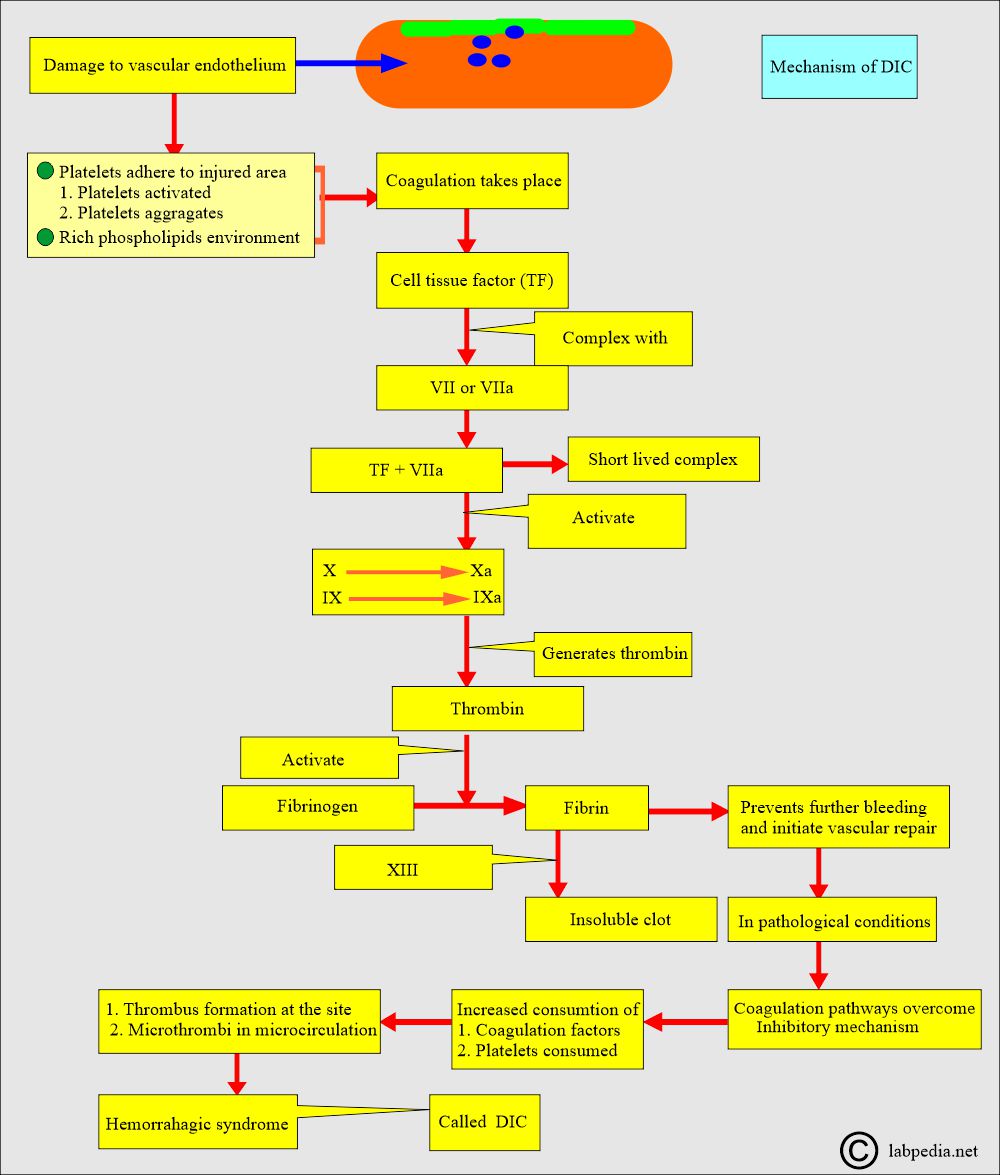
- The DIC is initiated by the release of tissue factor (TF) from endothelial cells, either due to direct endothelial injury or endothelial activation.
- Tissue factor (TF) is also released directly into the blood:
- From the white blood cells (monocytes).
- Immune complexes.
- Malignant cells.
- Tissue factor (TF) is present in endothelial cells. It is released when endothelial cells are damaged.
- Cell-damaging agents are:
- Endotoxin.
- Cytokines (Interleukin-1, 6, and 8).
- Tumor necrosis factor-α.
- Platelet-activating factor.
- Summary of DIC pathogenesis:
- Initiated by the endothelial cell damage and release of tissue factor (TF).
- The tissue factor (TF) stimulates the coagulation factors.
- Activation of plasmin and thrombin.
- Accelerated consumption of coagulation factors.
- Clotting and hemorrhage will take place.
- Snake venom can activate factor X to Xa.
- Damaged endothelium and inhibited the anticoagulant activity, there is uninhibited thrombin activity, and unrestricted formation of clots.
How will you classify Disseminated Intravascular Coagulopathy (DIC)?
- DIC is divided into two types:
- Acute DIC.
- Chronic DIC.
What are the causes of Disseminated Intravascular Coagulopathy (DIC)?
- DIC is not a primary disease; it is secondary to other causes, such as:
- Severe infection (sepsis).
- Snake bite.
- Heat stroke.
- Blood transfusion reaction.
- Burns.
- Severe trauma.
- Advanced malignancies.
- Obstetric complications like amniotic fluid embolism and abruptio placentae.
- Hypersensitivity reactions.
- Vascular abnormalities.
- Widespread tissue damage.
- Other causes include liver failure, pancreatitis, snake venom, heatstroke, and acute hypoxia.
- Other causes include liver failure, pancreatitis, snake venom, heatstroke, and acute hypoxia.
What are the clinical features of acute Disseminated Intravascular Coagulopathy (DIC)?
- It is uncompensated DIC.
- Coagulation factors are consumed faster than they are replaced.
- What are the causes of Acute DIC?
- Trauma.
- Sepsis.
- Shock.
- Burns.
- Eclampsia.
- Amniotic fluid embolism.
- Acute promyelocytic leukemia, FAB M3.
What are the Lab findings in acute DIC?
- There is thrombocytopenia.
- Fibrinogen is decreased.
- Factor VIII is decreased.
- There is microangiopathic hemolytic anemia.
- Increased PT, APTT, and positive protamine sulfate test.
| Lab tests | Result |
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
What are the clinical features of chronic Disseminated Intravascular Coagulopathy (DIC)?
- This is a compensated form of DIC.
- The coagulation factors that are consumed are compensated for or replaced.
- What are the causes of chronic DIC?
- In various malignancies of the Pancreas, lungs, stomach, and breast.
- It is also seen in leukemias.
- Myeloproliferative disorders.
- Obstetric disorders.
- Paroxysmal nocturnal hemoglobinuria.
What are the Lab findings in acute and chronic DIC?
- Normal platelet count.
- Normal PT, APTT, and fibrinogen.
- Positive protamine sulfate test.
| Advised test | Acute DIC | Chronic DIC |
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
What is the mechanism of Disseminated Intravascular Coagulopathy (DIC)?
- In DIC, there is increased consumption of coagulation factors, leading to their depletion.
- Also, due to microclots, platelets are depleted.
- Plasmin increases fibrinolysis and leads to fibrinogen degradation products (FDP) and D-dimer formation.
- There is a trigger for increased clot formation; then fibrinolysis leads to the formation of FDP and d-dimer.
- Plasmin acts on Fibrin polymer clots and gives rise to FDP and D-dimer.
- FDPs and Plasmin act on the fibrin clot and give rise to D-dimer products.
What are the S/S of disseminated intravascular coagulopathy (DIC)?
- The patient may have weakness and malaise.
- The main feature is bleeding, especially from the venipuncture site or a recent injury.
- There may be bleeding in the gastrointestinal tract. Oropharynx, into the lungs, and in the urogenital tract.
- During delivery, vaginal bleeding may be very severe.
- Acrocyanosis is characterized by irregularly shaped cyanotic patches.
- Microthrombi may cause skin lesions.
- There may be gangrene of the finger or toes.
- There may be occult bleeding to massive GIT bleeding.
- There is abdominal distension.
- Patients may develop renal failure.
- There may be hematuria.
- There is oliguria.
- Patients may have cerebral ischemia.
- There may be subarachnoid hemorrhage.
- There is a slight confusion about convulsions and coma.
- These patients have respiratory symptoms like:
- Cyanosis.
- Hypoxemia.
- Adult respiratory distress syndrome (ARDS).
- Tachypnea.
- Pulmonary infarction.
- Some patients with mucin-producing adenocarcinoma may develop subacute or chronic DIC.
What are the complications of Disseminated Intravascular Coagulopathy (DIC)?
- Thrombotic conditions such as deep vein thrombosis, sickle cell anemia, pulmonary embolism, and malignancy-related thrombosis are associated with elevated D-dimer levels.
- FDP and D-dimer form as a complication of disseminated intravascular coagulopathy (DIC).
How do you determine the Diagnosis of Disseminated Intravascular Coagulopathy (DIC)?
- Fibrinogen concentration is low.
- Platelets are low.
- Thrombin time is prolonged.
- Fibrinogen degradation products (FDP) and D-dimer are elevated and detected in urine and serum.
- PT and APTT are prolonged in the acute phase.
- The D-dimer test detects the cross-linked fibrin degradation products.
- The D-dimer assay is more specific than the FDP assay.
- D-dimer is a highly specific marker of fibrin degradation products.
- Combining the positive FDP and D-dimer tests is highly specific and sensitive for diagnosing DIC.
- A positive D-dimer result is evidence of DIC or other causes of intravascular thrombosis.
- D-dimer can be used as a screening test for deep vein thrombosis (DVT).
- The concentration of fibrin breakdown products will increase when fresh venous thrombosis occurs.
- A negative result is useful in the emergency department for excluding DVT in clinically suspected patients.
What is the advantage of D-dimer?
- There is no interference from fibrinogen, so the test can be performed on plasma without the need to collect it in a special tube.
What are the disadvantages of D-dimer?
- It has limited usefulness because it is used in fibrinolysis and will not detect fibrinogen breakdown products.
- Elevated D-dimer levels have limited value in cancer, post-surgical inflammation, or trauma, limiting their usefulness.
How will you classify Disseminated Intravascular Coagulopathy (DIC) on various factors?
| The groups of Disseminated Intravascular Coagulopathy (DIC) | Main lab criteria |
|
|
|
|
|
|
|
|
What are the Normal values of D-dimer?
Source 1
- Negative
- <0.25 mg/L
Source 2
- Normal = negative ( no D-dimer fragments are seen).
- <250 ng/mL (<250 µg/L).
Source 4
- Normally, plasma D-dimer levels are negative.
- Qualitative: It is negative
- Quantitative : < 250 ng/mL or < 250 µg/L ( SI unit)
- Critical value >40 mg/L (40 µg/mL).
Source 6
- <0.4 mcg/mL
What factors will lead to a False-positive test?
- This is seen in heparin therapy.
- The Rheumatoid factor can yield falsely elevated FDP values.
- This test is positive in patients after surgery or trauma.
- The false-positive test is seen in estrogen therapy and pregnancy.
What are the causes of increased levels of D-dimer?
- Primary and secondary fibrinolysis.
- DIC
- Thrombolytic therapy.
- Deep vein thrombosis.
- Pulmonary embolism.
- Arterial thromboembolism.
- Vaso-occlusive crises of sickle cell anemia.
- Pregnancy (Especially the postpartum period).
- Malignancy.
- Surgery.
Questions and answers:
Question 1: What are the complications of DIC?
Question 2: What is the lab diagnosis of Disseminated Intravascular Coagulopathy (DIC) ?
- Please see more details in the fibrinogen degradation products FDP.

very informative. Do visit our website https://medintu.in/d-dimer-test/vizag/
Your website looks very good. My website is my hobby and charity.
Really very nice article. thanks for sharing. check this also- https://www.deepnursingbureau.com/
Thanks.
This is very useful guidance. I will definitely apply it during my D-Dimer Test. I have checked it at mrinagpur.com and I am thankful for this help
This is very useful guidance. I will definitely apply it during my D-Dimer Test. I have checked it at https://mrinagpur.com and I am thankful for this help
You are most welcome.