Cholesterol (Serum Cholesterol)
Serum Cholesterol
Sample for Serum Cholesterol
- The best sample is after 12 hours of fasting, and that is the morning sample.
- The best sample is serum separated within 2 hours of the collection.
- This test may be done on Serum or Plasma (EDTA) but not oxalate, citrate, or fluoride.
- The serum is stable at 4 °C for 5 to 7 days and 3 months at -20 °C.
- Avoid freezing and thawing.
- The result with EDTA plasma is 3% lower than serum.
- Sample with Cholesterol above 500 mg/dL should be diluted.
Precautions for serum cholesterol
- Try to separate serum or plasma from the cells within 2 hours.
- The best sample is after 12 to 14 hours of fasting.
- Pregnancy may give a high level.
- Drugs that may increase the level are anabolic steroids, corticosteroids, oral contraceptives, vitamin D, phenytoin, thiazide diuretics, and cyclosporin.
- Drugs that may decrease the level are captopril, colchicine, erythromycin, isoniazid (INH), lovastatin, neomycin, bile salt binding agents, androgens, niacin, and nitrates.
Purpose of the test (Indications) for serum cholesterol
- Cholesterol level is estimated to determine the coronary artery disease risk.
- This test may be needed to rule out hyperlipidemia.
Pathophysiology of serum cholesterol
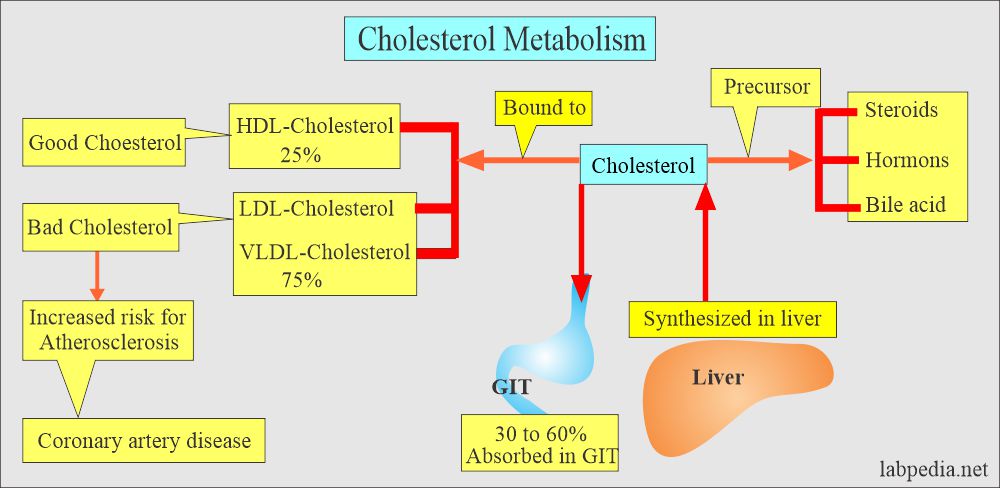
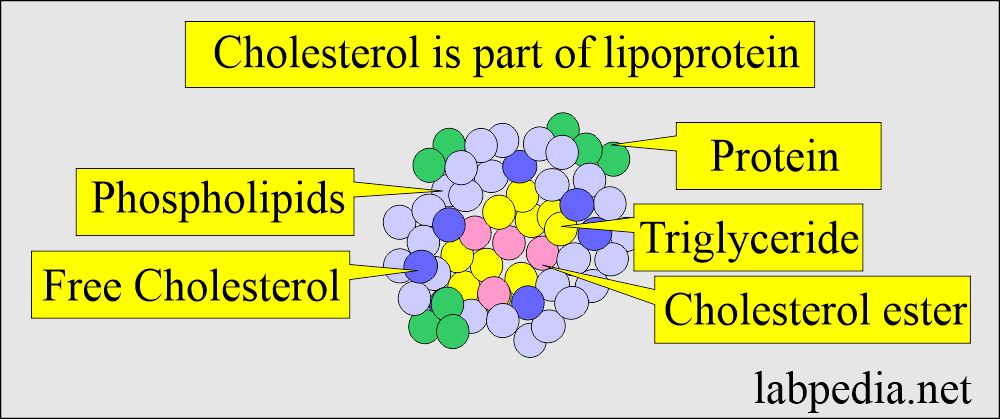
- Total serum cholesterol comprises all of the Cholesterol found in the various lipoproteins.
- Cholesterol is an organic molecule, is a sterol or modified steroid, a type of lipid.
- This is an essential part of all cell membranes.
- Cholesterol is the major component of LDL and a minority part of VLDL and HDL.
- Cholesterol is the best-known steroid because of its association with atherosclerosis.
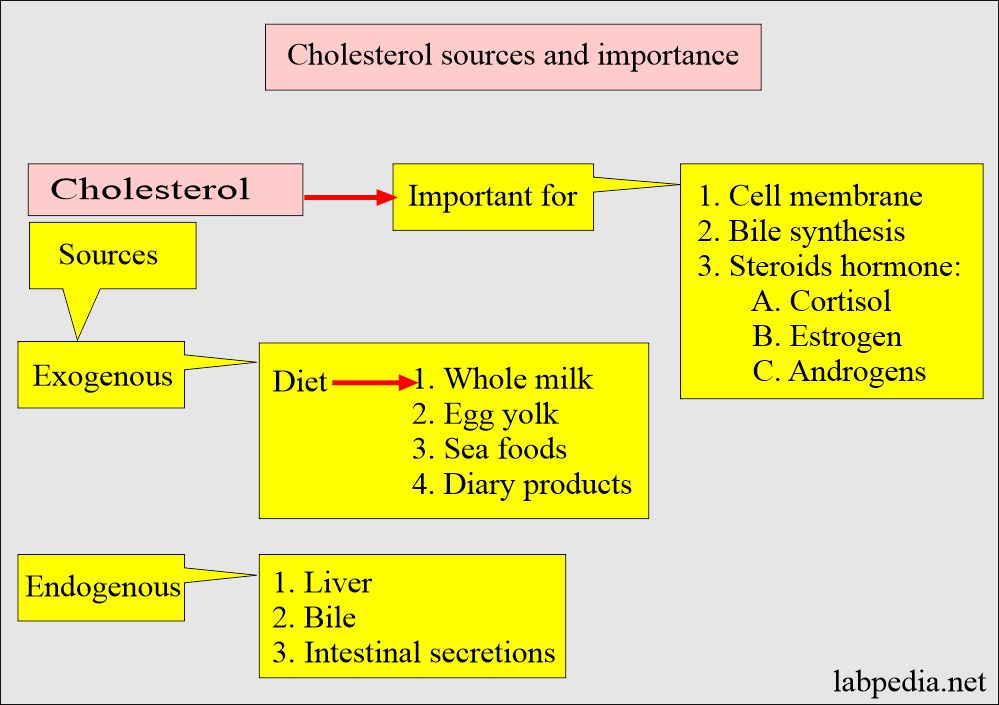
- Cholesterol has biochemical significance because it is the precursor for important steroids like bile acids, adrenocortical hormones, sex hormones, Vitamin D, cardiac glycosides, sitosterol of the plant kingdom, and some alkaloids.
- Cholesterol is steroid alcohol with 27 carbon atoms.
- Cholesterol is present virtually in all cells and body fluids.
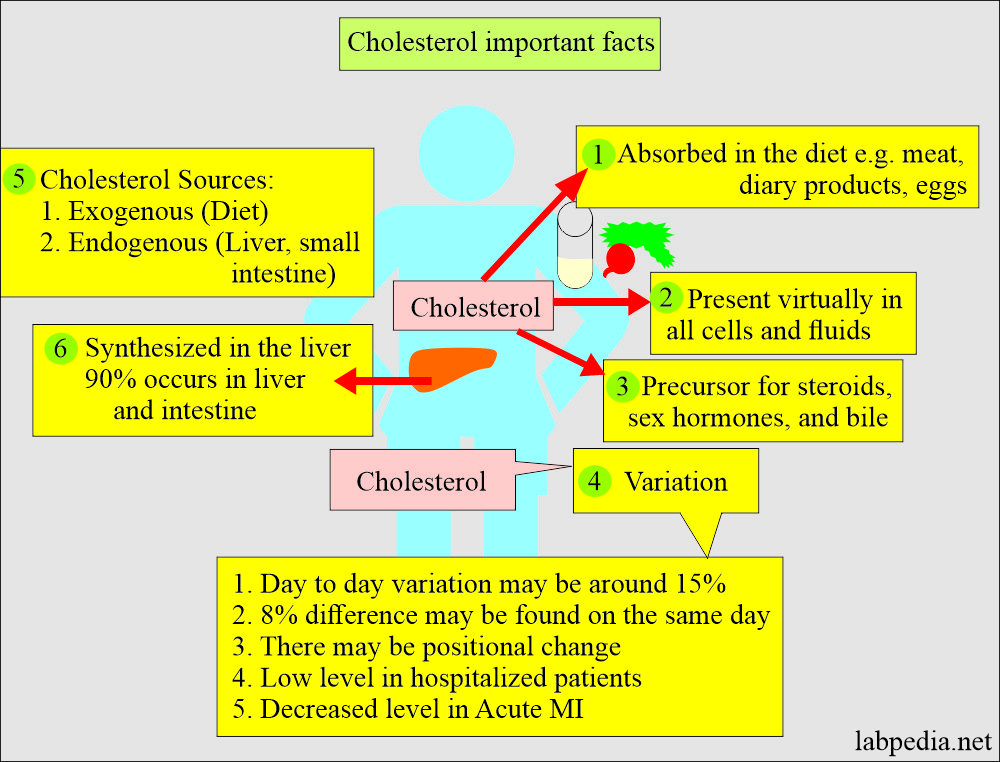
- Cholesterol is absorbed in the diet and synthesized in the liver and gut.
- It is a precursor of steroid hormones, bile acids, sex hormones, and cellular membranes.
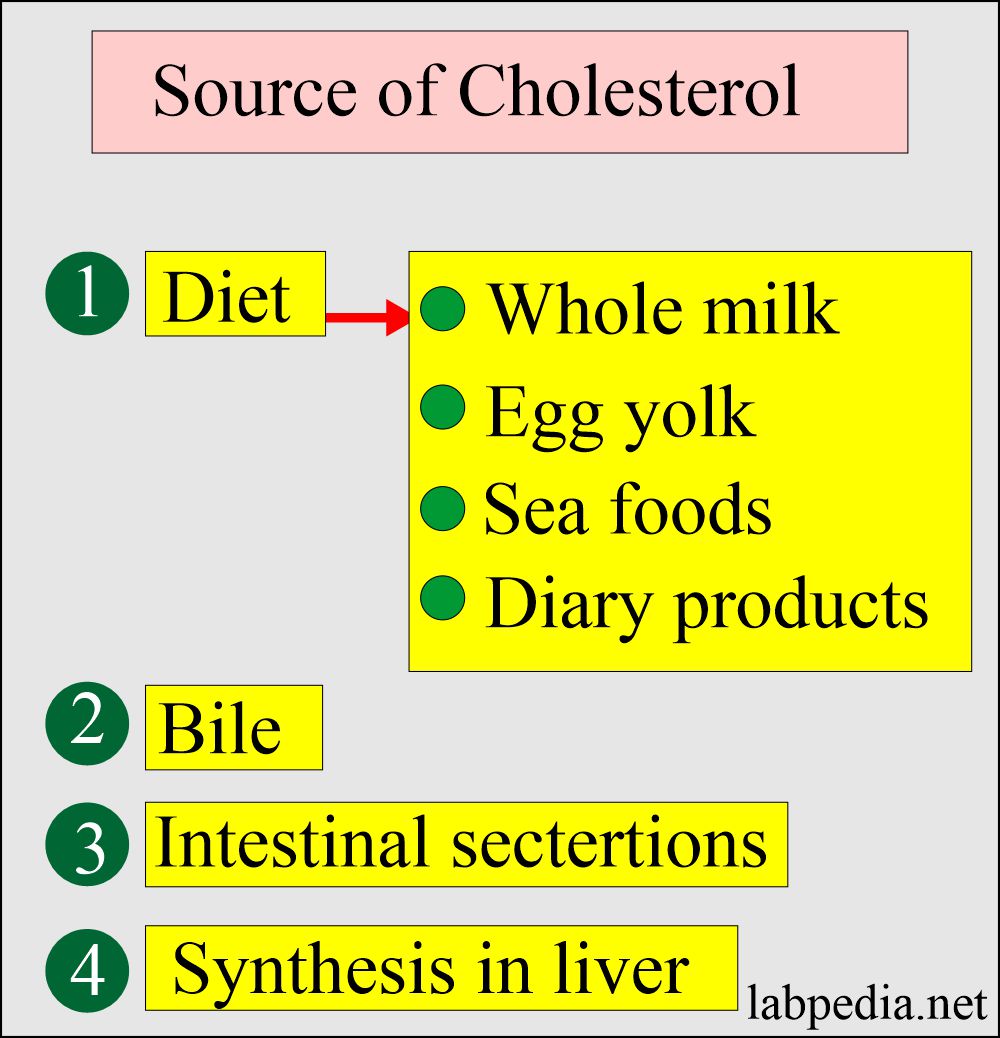
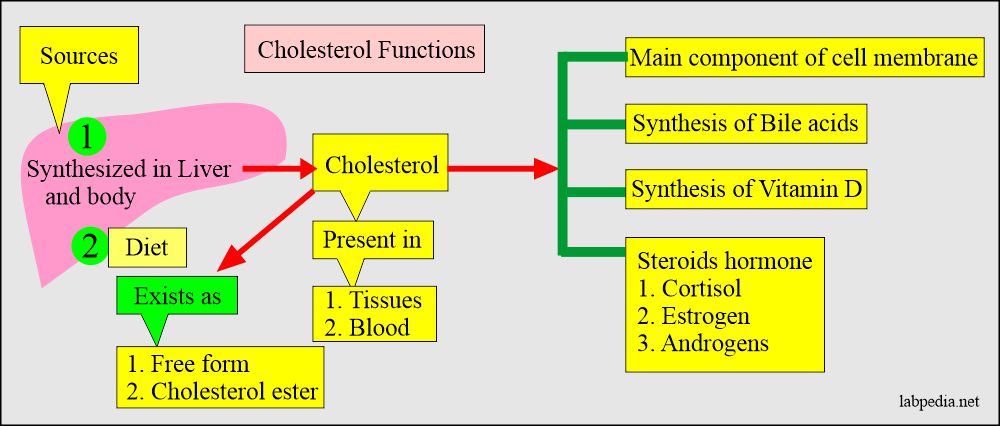
Sources of Cholesterol:
- Cholesterol sources:
- Exogenous sources are present in the diet, mainly from animal sources, and absorbed by the gastrointestinal tract.
- Endogenous sources are like the liver and other tissues.
- All the cells have the ability to synthesize Cholesterol, and 90% occurs in the liver and intestines.
- Malnutrition will give low cholesterol formation.
Cholesterol in the body and their calculation from LDL-cholesterol formula:
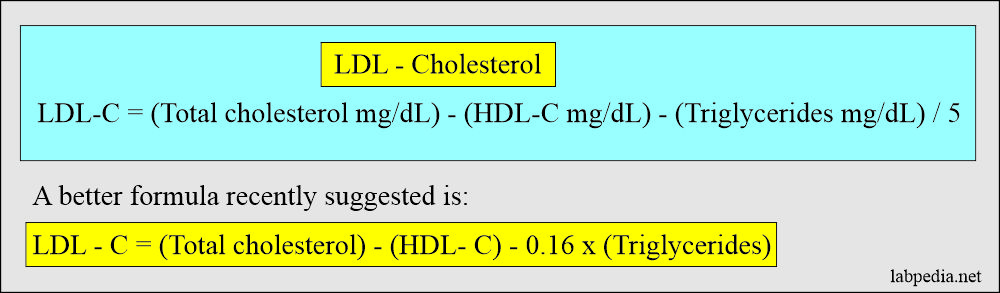
- Three different lipoproteins carry Cholesterol in the fasting serum. So, the total cholesterol sum equals the sum of these three components.
- Total cholesterol = HDL-cholesterol + VLDL-cholesterol + LDL-cholesterol
- The amount of Cholesterol in the HDL fraction can be found by precipitating from the serum.
- The level of Cholesterol in VLDL = Triglycerides/5
- This formula works in the fasting sample and when:
- The triglycerides are <400 mg/dL.
- No chylomicrons are seen.
- Does not work in type III dyslipidemia (β-VLDL).
- This formula works in the fasting sample and when:
- LDL – Cholesterol = The separation of LDL from the lipoproteins is very difficult, so the Friedewald equation is used, which is:
-
-
-
- LDL-cholesterol = (Total cholesterol mg/dL) – (HDL-cholesterol mg/dL) – (triglycerides mg/dl)/5.
-
-
-
Cholesterol level changes in the body and its distribution along with other lipoproteins:
- There is day-to-day variation in the cholesterol level.
- This day-to-day variation may be seen in persons around 15%.
- An 8% difference can be found on the same day.
- There is a positional change in the level.
- The level may be decreased by as much as 15% in the recumbent position.
- There is a low level in the hospitalized patient.
- Because of these variations, two samples must be tested for heart disease risk.
- There is a decreased Cholesterol level in acute MI, as much as 50% for 6 to 8 weeks.
Cholesterol distribution in the lipoproteins:
| Type of lipoprotein | Cholesterol | Triglycerides | Phospholipids | Proteins |
| Chylomicron | 3% to 5% | 85% to 95% | 5% to 10% | 1% to 2% |
| HDL (High-density lipoprotein) | 20% | Very small amount | 30% | 50% |
| LDL (Low-density lipoprotein) | 45% | 5% to 10% | 20% to 30% | 15% to 25% |
| VLDL (Very-low-density lipoprotein) | 10% to 15% | 60% to 70% | 10% to 15% | 10% |
Cholesterol absorption:
- The primary source of Cholesterol is diet. Another source is endogenous.
- Cholesterol is an important constituent in the assembly of the cell membrane.
- Cholesterol is the basic part of synthesizing bile acids and steroid hormones (cortisol, estrogen, androgen).
- In the normal biological process, Cholesterol undergoes changes like synthesis, recycling, and degradation.
- Cholesterol enters the intestine from the following sources:
- For food like egg yolk, meat, fat-diary products, and seafood, the average amount is 400 to 700 mg/day.
- Plant sterols (200 to 300 mg) are ingested daily. These are poorly absorbed.
- Bile provides another fraction of Cholesterol.
- Intestinal secretions and turnover of the intestinal mucosal cells are other sources.
- For food like egg yolk, meat, fat-diary products, and seafood, the average amount is 400 to 700 mg/day.
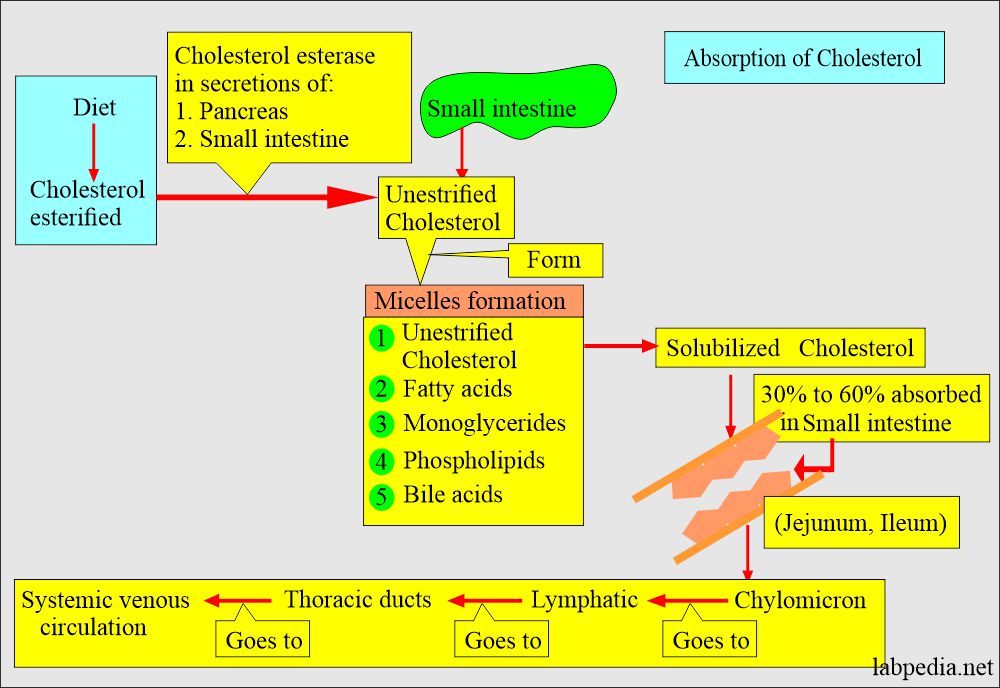
- Bile acids are detergents and are the most critical factor affecting micelles formation.
- Without bile acids, digestion and absorption of Cholesterol and triglyceride are severely affected.
- Most absorption of Cholesterol takes place in the jejunum and ileum.
- When Cholesterol enters the intestinal cells, it is packaged with triglycerides, phospholipids, and apolipoproteins into large lipoproteins called chylomicrons.
- An increased amount of fat in the diet, particularly triglycerides 98%, will result in more micelles formation, allowing more Cholesterol to be solubilized and absorbed.
- Approximately 60% of the total Cholesterol in the male plasma is carried by LDL 22%, HDL 13%, and Chylomicrons 5%.
Cholesterol esterification:
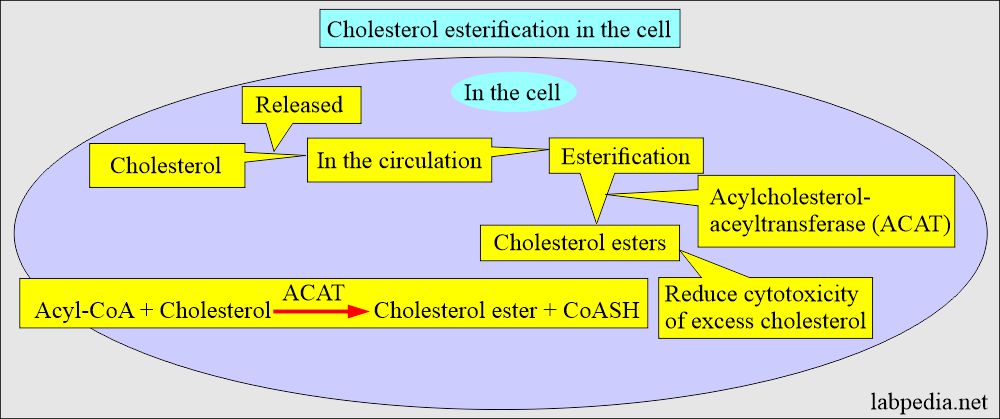
- Cholesterol is esterified to fatty acids to form a cholesterol ester by two enzymes:
- In the cells, excess cholesterol is esterified by acyl-cholesterol acyltransferase (ACAT), forming cholesteryl ester.
- This process will help to prevent the toxicity of the excess cholesterol.
- Cholesteryl esters are stored in the cells as lipid drops.
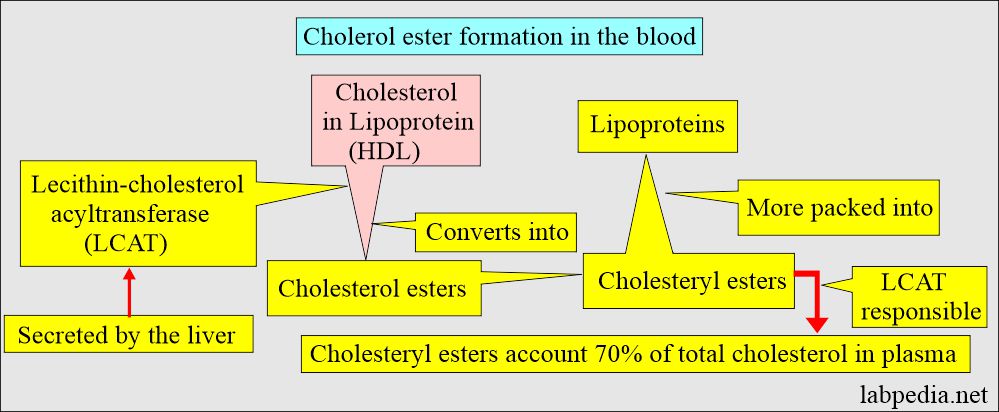
- In blood circulation, Cholesteryl esters also form by the action of lecithin cholesterol acyltransferase (LCAT) on cholesterol in lipoproteins, particularly High-density lipoprotein (HDL).
- LCAT is responsible for the conversion of cholesterol into ester.
- LCAT is secreted by the liver into the blood circulation, activated by the apolipoprotein A-1, the main component protein of HDL.
- Cholesteryl ester accounts for about 70% of the total cholesterol in the blood.
- Cholesterol, once formed, enters the blood circulation.
- Cholesterol is esterified and combined with apoprotein and apolipoprotein and ultimately carried as a lipoprotein.
- Cholesterol esterification helps in the packing of Cholesterol into lipoproteins.
- Both dietary and synthesized Cholesterol are converted to cholesteryl esters, easily packed into lipoproteins.
- Esterification increases the lipid-carrying capacity of the lipoproteins in plasma and prevents the toxicity effect of Cholesterol.
- 75% bound to LDL.
- 25% bound to HDL.
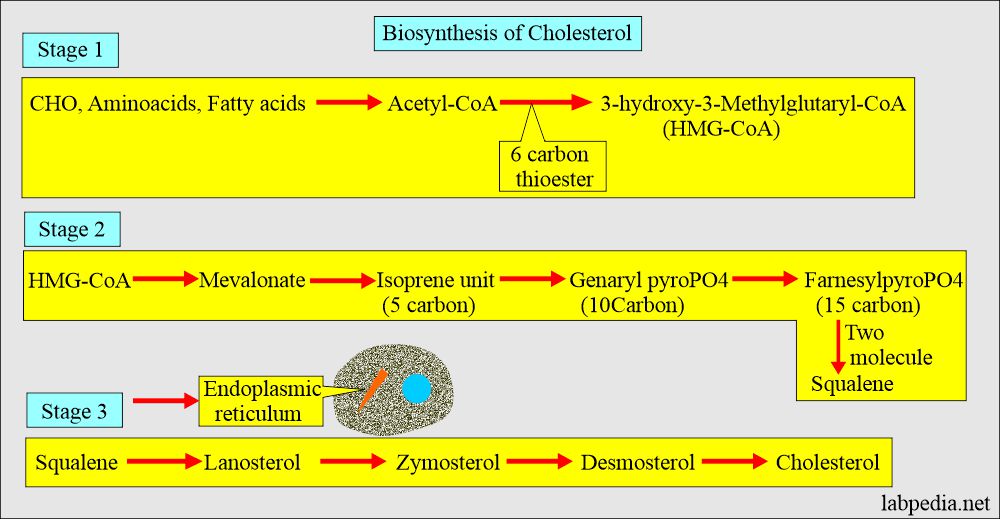
Biosynthesis of Cholesterol
- 90% of cholesterol synthesis takes place in the liver and gut.
- Cholesterol synthesis takes place in three stages.
- The starting molecule is acetate.
- All body cells have the ability to synthesize Cholesterol from acetyl-CoA.
- Knowing the endogenous synthesis of Cholesterol, drugs are developed that lower the cholesterol level, like mevastatin, lovastatin, simvastatin, pravastatin, and atorvastatin, which will suppress the HMG-CoA reductase.
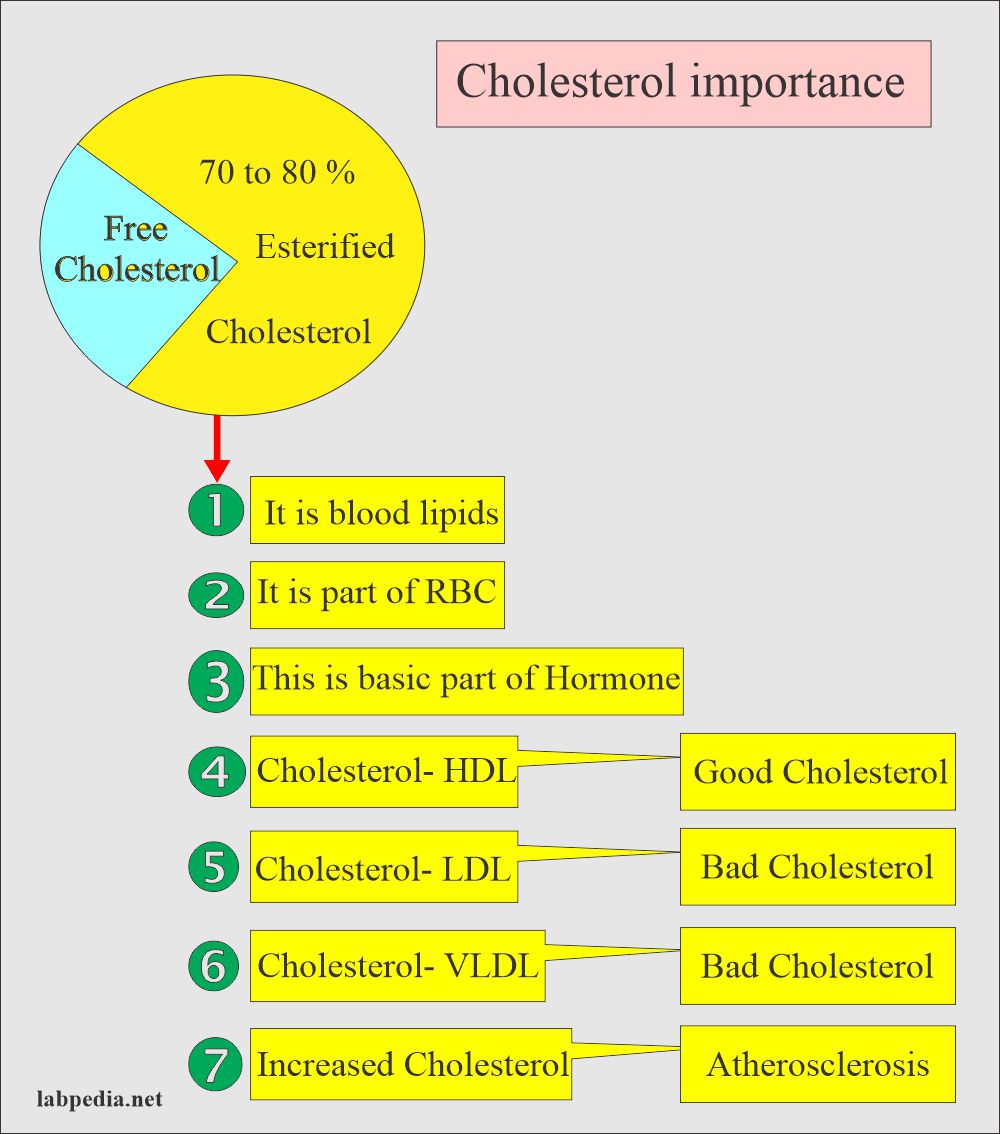
Cholesterol exists in two forms:
- Free Cholesterol.
- Esterified Cholesterol.
- 75% to 85% of the total Cholesterol is in the form of esterified Cholesterol.
- Cholesterol can be derived from dietary sources like meat, eggs, butter, and plants.
- 30 to 60% of dietary Cholesterol is absorbed.
- Once Cholesterol is absorbed into the mucosal cells, it becomes part of the large micelle called Chylomicron.
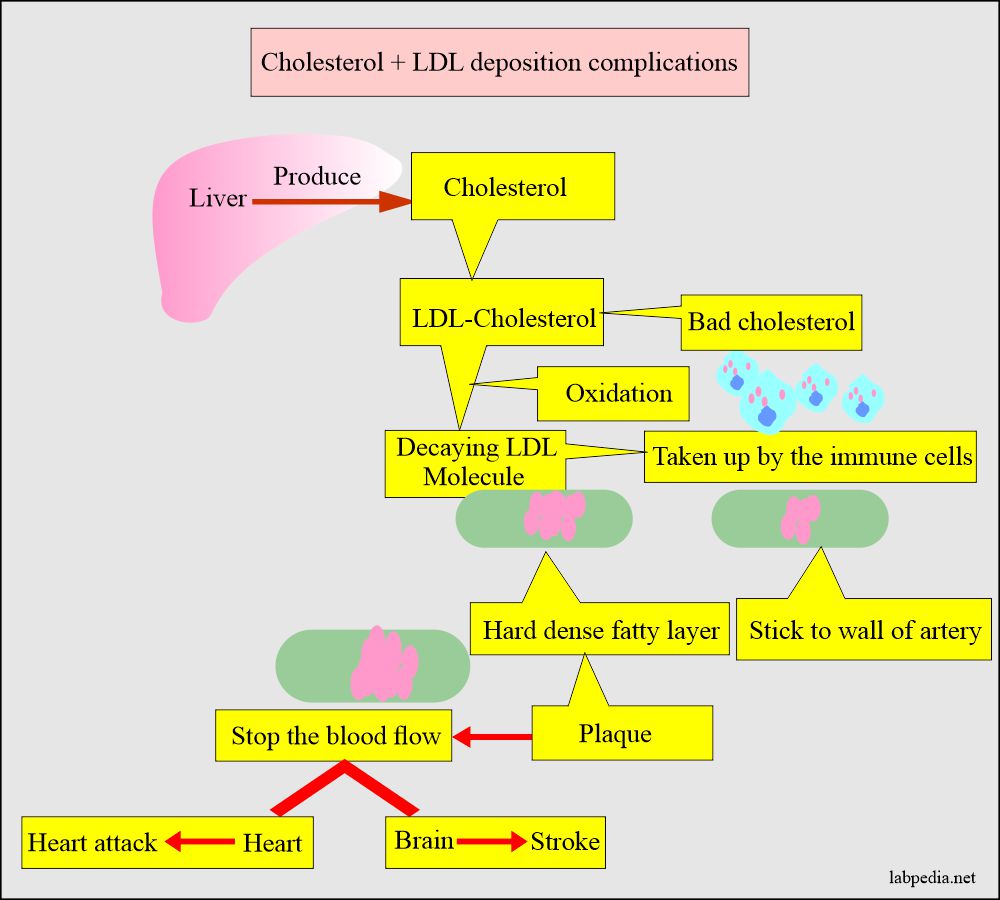
Cholesterol complications:
- Cholesterol’s main complication is atherosclerosis, which leads to heart disease and stroke.
Cholesterol distribution in other lipids:
| Cholesterol found in: | Cholesterol % in other lipids |
| Chylomicron |
|
| VLDL |
|
| LDL |
|
| HDL |
|
Cholesterol functions:
- Cholesterol is a blood lipid (fat).
- Cholesterol is a normal part of RBC.
- Cholesterol, when increased, leads to atherosclerosis and is the main lipid.
- A total raised level of Cholesterol is associated with an increased risk of cardiovascular disease. Its subtypes LDL-C and HDL-C are more important than the total Cholesterol.
- Cholesterol is the basic unit of hormone produced by adrenal glands, ovaries, and testes.
- Cholesterol is needed for bile acids and cellular membranes.
- Cholesterol is transported in circulation by carrier proteins.
- Cholesterol bound to high-density lipoprotein (HDL- cholesterol) is known as good Cholesterol. HDL will prevent atherosclerosis.
- Cholesterol bound to low-density protein (LDL-cholesterol) is known as bad Cholesterol and increases atherosclerosis chances.
- Also, the same is Cholesterol bound to very low-density lipoprotein (VLDL) is bad Cholesterol.
- Increased Cholesterol level is associated with atherosclerosis and coronary vessel disease.
- It is needed to form steroids, sex hormones, and bile acids.
- This is the part of cellular membranes.
- It gives the risk of heart disease.
Normal Cholesterol level
Source 1
Adult
- The desired level to prevent coronary disease is < 200 mg/dl
- Moderate risk is 200-239 mg/dl
- High risk is > 240 mg/dl
- CSF <0.5 mg/dl
Source 2
| Sample | Male mg /dL | Female mg /dL |
| Cord blood | 44 to 103 | 50 to 108 |
| 0 to 4 years | 114 to 203 | 112 to 200 |
| 5 to 9 years | 121 to 203 | 126 to 205 |
| 10 to 14 years | 119 to 202 | 124 to 201 |
| 20 to 24 years | 124 to 218 | 122 to 216 |
| 30 to 34 years | 138 to 254 | 130 to 230 |
| 40 to 44 years | 151 to 268 | 147 to 252 |
| 50 to 54 years | 158 to 277 | 162 to 285 |
| 60 to 64 years | 159 to 276 | 172 to 297 |
| >70 years | 144 to 265 | 173 to 280 |
- To convert into SI unit x 0.0259 = mmol/L
Cholesterol and its relation to heart disease:
- Desirable level is = < 170 mg/dl
- Moderate risk is = 170-199 mg/dl
- High risk is = > 200 mg/dl
- Above 240 mg/dL = needs treatment.
- Nowadays, the Cardiology Association recommends the level to be around 160 mg/dl.
| Cholesterol mg/dL | Risk |
| <160 | Very low |
| 160 to 199 | low risk |
| 200 to 239 | moderate risk |
| 240 to 279 | high risk |
| >280 | very high risk |
- According to the latest NHS research study, there is no relation between total cholesterol and heart disease risk.
ATP III (Adult treatment panel) recommendations for blood lipids are:
| Chemical substance (Lipid) | Clinical effects on the people |
| Cholesterol |
|
| HDL |
|
| LDL |
|
ATP III (Adult treatment panel) LDL target level for coronary vascular disease:
| Risk factors | Details of risk factors | The target LDL level required ( This level is mandatory) |
|
CHD heart disease risk factors are:
|
|
|
Major risk factors including are:
|
<130 mg/dL |
| <2 major risk factors | <160 mg/dL |
Framingham formula calculations (Risk score counting):
| Risk factors | Points for the calculation for women | Points for the calculation for men |
|
|
|
|
|
|
|
|
|
| All non-smokers | 0 point | 0 point |
|
|
|
|
|
|
10 years risk for cardiovascular diseases according to Framingham risks in %:
| Total points | % Framingham score (risk) |
| 0 point | <1% |
| 1 to 4 points | 1% |
| 2 points | 5% to 6% |
| 7 points | 3% |
| 8 points | 4% |
| 9 points | 5% |
| 10 points | 6% |
| 11 points | 8% |
| 12 points | 10% |
| 13 points | 12% |
| 14 points | 16% |
| 15 points | 20% |
| 16 points | 25% |
| 17 points | >30% |
Total Cholesterol relation to coronary artery disease:
- Another source:
- Desirable level = <200 mg/dL
- Borderline level = 200 to 239 mg/dL
- High Risk level = >240 mg/dL
Cholesterol and triglycerides risk factors for coronary artery disease (NCEP expert panel and ATP III guideline):
| Risk factors grades | Total cholesterol | Total triglycerides | Total cholesterol/HDL-C ratio | LDL/HDL ratio |
| Normal or low-risk | <200 mg/dL | <150 mg/dL | 3.3 to 4.4 |
0.5 to 3.0
|
| Average risk (>optical risk) | 150 to 190 mg/dL | 4.4 to 7.1 | ||
| Moderate or borderline risk | 200 to 239 mg/dL | 200 to 499 mg/dL | 7.1 to 11.0 | 3.0 to 6.0 |
| High-risk group | >240 mg/dL | >500 mg/dL | >11.0 | >6.0 |
Optimal values of lipids (ATP III guidelines):
| Risk level | LDL cholesterol | Total cholesterol | Triglycerides | HDL cholesterol |
| Optimal fasting values | <1000 mg/L | <2000 mg/L | <150o mg/L | >400 mg/L |
| Near-optimal fasting level | 1000 to 1290 mg/L | |||
| Borderline high fasting level | 1300 to 1590 mg/L | |||
| High fasting level | 1600 to 1890 mg/L | |||
| Very high fasting level | >1900 mg/L |
Increased Cholesterol (Hypercholesterolemia):
- Familial combined hyperlipidemia.
- Hyperlipoproteinemia type, 1V, V.
- Intra- and extrahepatic cholestasis.
- Glomerulonephritis.
- Nephrotic syndrome and chronic renal failure.
- Malignant neoplasm of pancreas and prostate.
- Hypothyroidism.
- Gout.
- Diabetes mellitus.
- Alcoholism.
- Glycogen storage disease type 1 (Von Gierke disease).
- Stress.
- Biliary cirrhosis.
Decrease Cholesterol (Hypocholesterolemia):
- alpha-Lipoprotein deficiency.
- Hepatocellular necrosis.
- Malignant neoplasm of the liver.
- Hyperthyroidism.
- Malabsorption and malnutrition (starvation).
- Severe acute illness.
- Extensive burns.
- Rheumatoid arthritis.
- Cholesterol-lowering medications.
Prevention, recommendations, and treatment for the cholesterol level:
| Total cholesterol <200 mg/dL |
|
| Total cholesterol 200 to 239 mg/dL |
|
| Total cholesterol >240 mg/dL |
|
Risk factors leading to heart disease are:
- Cigarette smoking.
- Cerebrovascular disease.
- Diabetes mellitus.
- Hypertension.
- The family history of coronary heart disease.
- Sex is male.
- Overweight >30%
- peripheral occlusive vascular disease.
Important:
-
- There is variation in the level of Cholesterol, so take at least two samples.
- Critical value = >500 mg/dL.
Chemical substance Panic value (critical value) Cholesterol >240 mg/dL (>500 mg/dL) HDL-cholesterol <40 mg/dL LDL- cholesterol >160 mg/dL Triglycerides >500 mg/dL
Questions and answers:
Question 1: What is ATP and its significance?
Question 2: What is the cholesterol level risk for coronary heart disease?

I agree with you
Thanks
[…] the liver, cholesterol, and triglycerides are packed into another type of lipoprotein called Very low-density […]