Chapter 24: Autoimmune diseases, Diabetes Mellitus Type 1, Insulin-Dependent Diabetes Mellitus, Juvenile-Onset Diabetes (IDDM)
November 18, 2020Elementary Immunology
TYPE I (INSULIN DEPENDANT) DIABETES MELLITUS (IDDM), Juvenile Diabetes
Definition
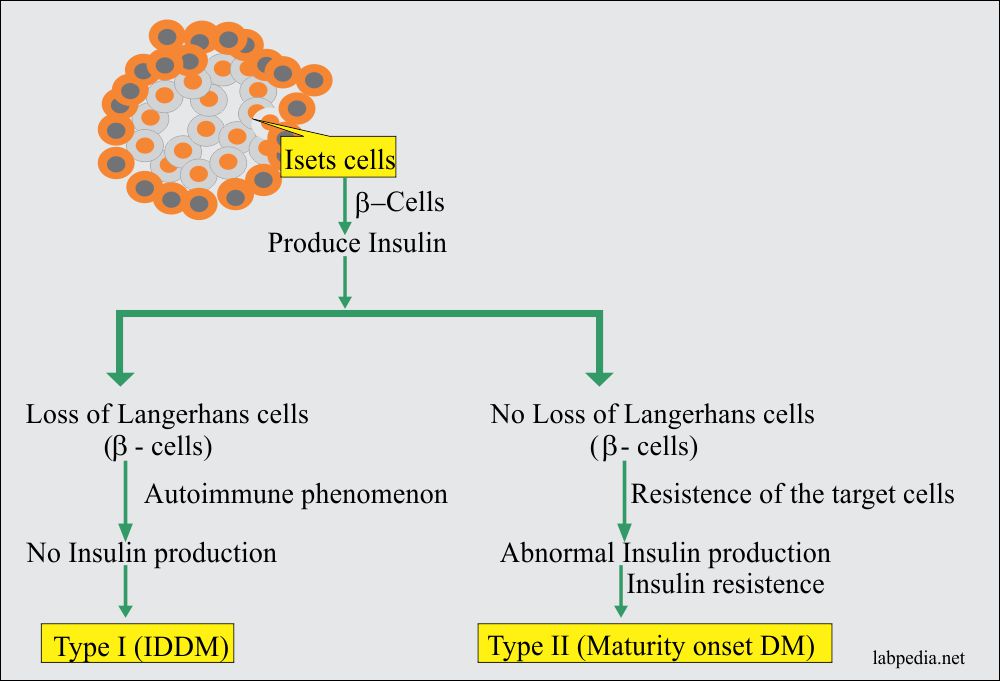
Type I or insulin-dependent diabetes mellitus (IDDM) is a state of hyperglycemia because of a lack of insulin secretion from the β-cells in islets of Langerhan’s of the pancreas. These patients need exogenous insulin to sustain life.
Age
- Most patients develop IDDM in early childhood or early adolescence but may be seen at any age.
- It has a peak onset around puberty. It is 5 to 43/100,000 population per year in Europe, while in the USA 16 cases/100,000 per year.
- 95% of the patients developing diabetes mellitus before the age of 30 years are IDDM.
Sex
Both sexes are equally affected.
Epidemiology
- 10% of the people with diabetes are IDDM, and most common in childhood.
- Roughly 10,000 new cases per year are diagnosed every year in the USA.
- This may be associated with other autoimmune diseases.
- It is found 30% to 50% in identical twins.
Clinical Features (Signs and Symptoms)
- Glucose may be present in urine at the time of diagnosis (glycosuria).
- The patient may have prodromal symptoms of:
- Weight loss.
- Thirst.
- Polydipsia.
- Polyuria.
- Sometimes patients may come with severe metabolic disturbance known as ketoacidosis coma.
Pathogenesis and Immunological Features
There is immune-mediated destruction of the insulin-producing cells of the pancreas, which are β-cells of Langerhans.
There are several hypotheses for the death of β-cell. The following two are more accepted.
- The presence of T-lymphocytes and selective loss of β-cells (insulin-producing) suggests targeting by T-cell receptor for β-cell-specific autoantigen. There is a predominance of CD8+ cells that suggests a cell-mediated cytotoxic reaction to damage β-cells.
- CD4+ T-lymphocytes also may play a central role in the immune process that leads to the development of diabetes Mellitus.
- This hypothesis says that inflammatory cells infiltrate is not specifically against β-cell. The insulitis may be initiated by a viral infection, resulting in cytokine production, e.g., IL-1 is cytotoxic to β-cells. Macrophagic cells may produce IL-I. So if the macrophagic function is inhibited by treatment with silica, diabetes does not develop in the experimental model.
- There is autoantibody against β-cells, and these are present for several years before hyperglycemia appears.
- Many patients have autoantibody, which binds the cytoplasm of the β-cells.
- The autoantibodies are:
- Autoantibodies against islet cells.
- Autoantibodies against insulin.
- Autoantibodies against glutamic acid decarboxylase.
- Insulinoma associated proteins (IA2, ICA512)
- Using the human pancreas, an autoantibody binding to the islet cell cytoplasm (islet cell antibody = ICA) is detectable in some 75% of the patients at the time of diagnosis.
- Insulin autoantibody (IAA) appears before the start of treatment with insulin.
- Islet cell-surface antibodies are detected, but their role in the disease is not clear.
- Congenital rubella is also found as an environmental factor.
- The presence of Coxsackievirus B and several other viruses suggests the possibility of different triggering mechanisms for this disease.
- A viral infection of the β-cells occurs, and there is immune-mediated destruction of the β-cells.
- There is genetic susceptibility, and this disease is found more in HLA-DR3 and HLA-DR4 antigens.
The relative risk for IDDM:
| HLA Typing | Relative Risk |
| HLA DR3 | 5 |
| HLA DR4 | 6.8 |
| HLA DR2 | 0.1 |
| HLA-DQw8 | 2 to 6 |
| HLA-Identical siblings of diabetic | 44.0 |
| Identical Twin of Diabetics | 230.0 |
Diagnosis
Following is the criteria to label diabetic:
- Fasting glucose level = ≥126 mg/dL.
- Nonfasting plasma glucose = ≥200 mg/dL.
- 2 hours of plasma glucose (on 75 grams of glucose tolerance test)= ≥200 mg/dL.
- Urine glucose is positive (Glycosuria).
- HbA1c is not used for the diagnosis of diabetes.
- An annual test for urine microalbumin should be done.
Treatment
- Insulin at the physiologic level is needed. This is insulin-dependent.
- For maturity-onset diabetes mellitus, there are no free receptors for insulin or decreased due to autoantibody, which binds to these receptors. So in these cases, increase the amount of insulin is needed because it has to compete for available receptors.
Complications
Complications include:
- Vascular diseases.
- Neurological dysfunctions.
- Renal diseases.
- Involvement of the eye.