Cardiac marker:- Part 1 – Diagnosis of Acute Myocardial Infarction (AMI)
Diagnosis of Acute Myocardial Infarction (AMI)
Sample for diagnosis of Acute Myocardial Infarction (AMI)
- The best sample is Venous blood to get a clear serum.
- Heparinized plasma can be used.
- Rapid Troponin-T can be done on whole blood (some available methods).
- Current recommendation on admission with the possibility of acute MI, a blood sample should be taken at intervals of:
- Blood sample at admission.
- Second sample at 2 to 4 hours.
- Third sample at 6 to 8 hours.
- Fourth sample at 12 hours.
- The serum can be stored at room temperature for 4 to 8 hours.
- At 4 °C, the serum is stable for 1 to 2 days.
- The serum is stable for 24 hours for troponin-T at 2 to 8 °C.
Precautions for diagnosis of Acute Myocardial Infarction (AMI)
- I/M injection may raise the level of CPK.
- Strenuous exercise and recent surgery may raise the CPK level.
- Early pregnancy may decrease the CPK level.
Definition of Acute Myocardial Infarction (AMI)
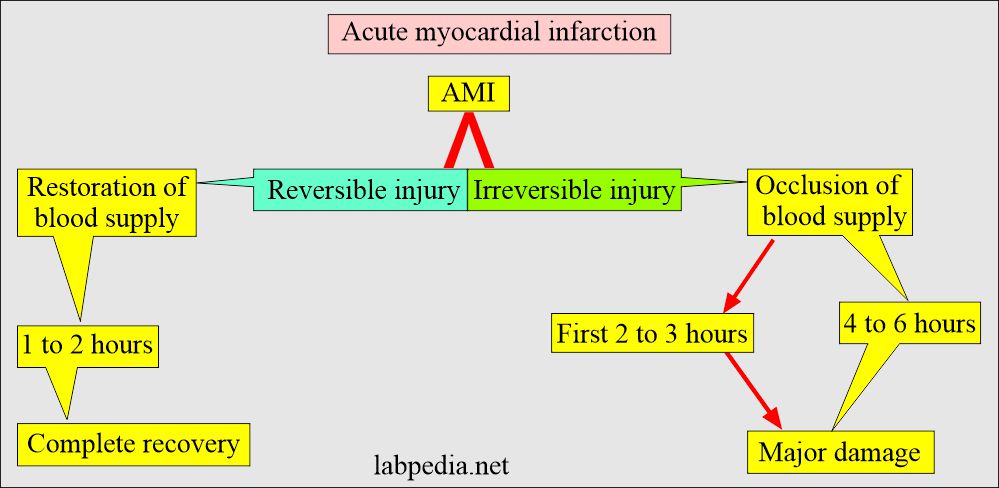
- This is characterized by the ischemia of the myocardial muscles. Also, this myocardial ischemia results in irreversible myocardial cell damage or death (necrosis).
- Or when there is obstruction of the blood supply to any part of the heart and necrosis of the muscles, or massive cell death occurs.
- It is almost always caused by atherosclerosis of the coronary arteries, followed by thrombosis.
- Clinical S/S is very important in both suspicious and diagnosed cases of AMI.
- Diagnosis depends upon the type of pain, its distribution, and its response to nitroglycerine.
- The pain characteristics are typical, and pain will respond to nitroglycerine.
- 20% to 30% of Acute Myocardial Infarctions (AMI) are painless.
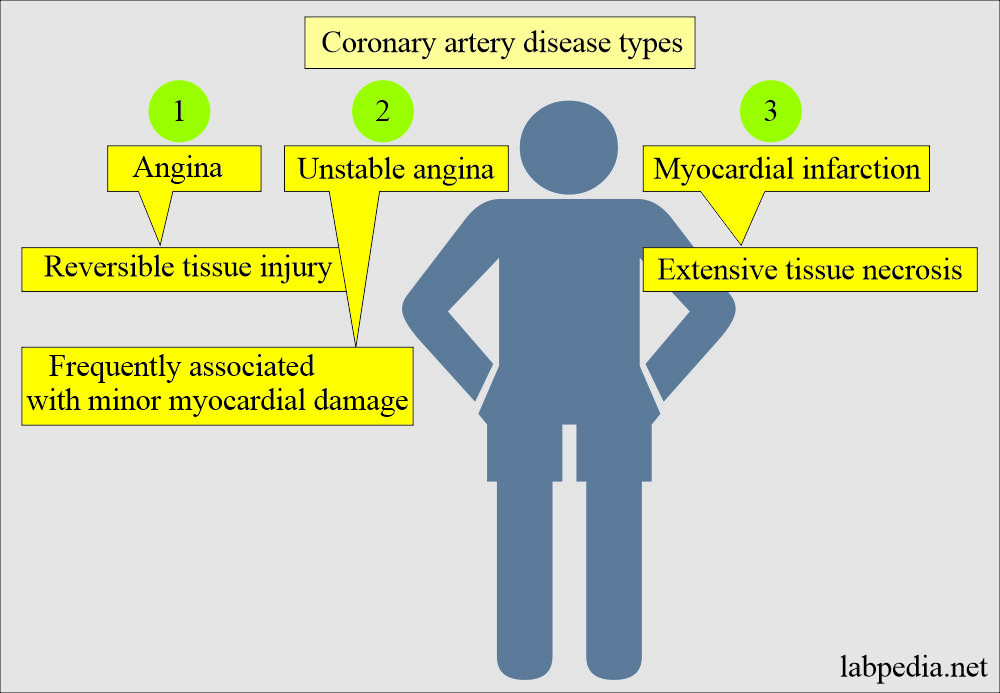
- Acute Coronary syndrome includes:
- Silent ischemia.
- Stable angina.
- Unstable angina.
- Non-ST wave elevation.
- Non-Q wave.
- Infarction to typical acute myocardial infarction (AMI).
Types of acute myocardial infarction (AMI):
- Silent myocardial infarction, where 40% to 50% of patients do not notice the typical signs and symptoms of acute myocardial infarction.
- These are diagnosed on the ECG.
- This is usually seen in diabetic patients and hypertension.
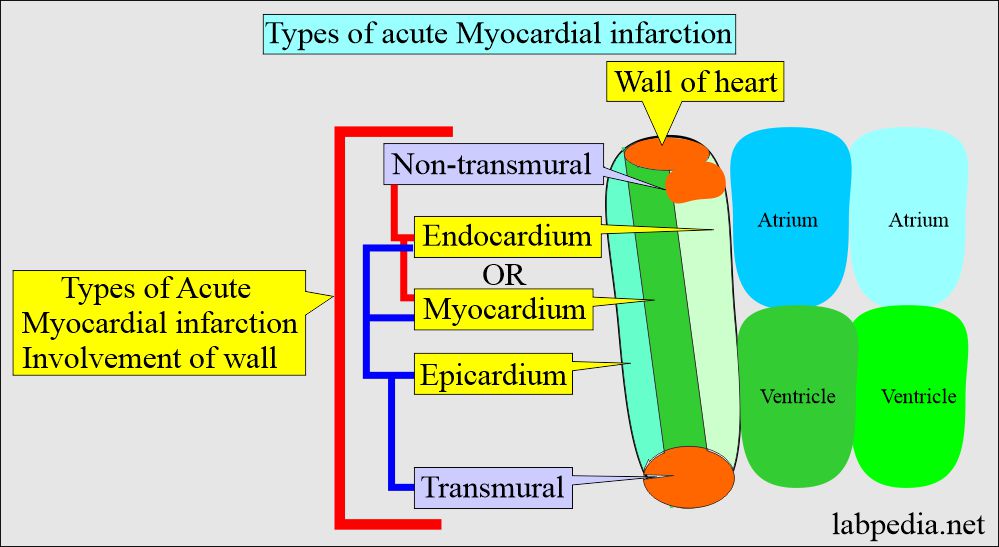
- The AMI is classified based on anatomic, morphologic, and diagnostic clinical data:
- Nontransmural AMI is when there is the involvement of only the endocardium or both endo and myocardium.
- Transmural MI occurs when all three endo, myo, and epicardium layers are involved.
- Another classification is:
- Non-Q wave subendocardial infarction.
- Q-wave was transmural infarction.
Pathophysiology of acute myocardial infarction
- There is an increased risk of AMI with increasing age.
- 4 to 5 times more risk in men between the ages of 45 to 54 years than women.
- The risk is the same in both sexes (men and women) after the age of 80 years.
- Before acute myocardial infarction occurs, there is transient ischemia where the oxygen supply is deprived of the muscle, which is called an Anginal attack.
- In angina, there is no necrosis.
- The major cause of AMI is atherosclerotic plaques and thrombus formation.
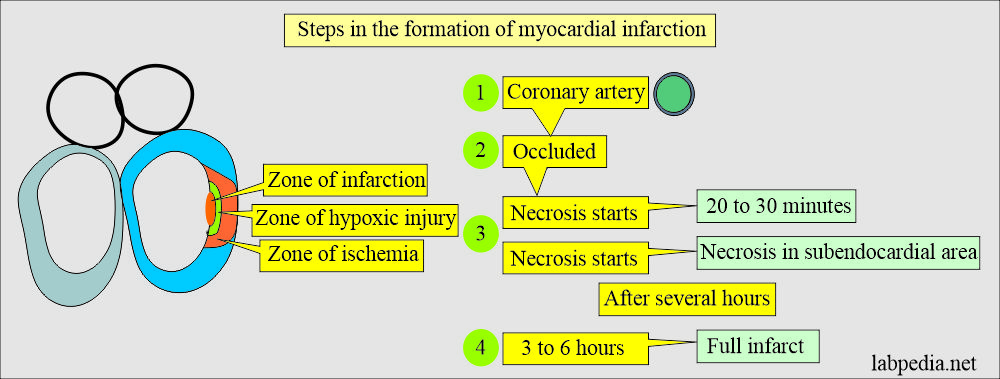
- Ischemia starts from the endocardium and then spreads outwards.
- Irreversible muscle damage occurs during ischemia for at least 15 to 20 minutes.
- Vasospasm and platelet aggregation may contribute to coronary occlusion.
- Myocardial necrosis starts:
- The necrosis process starts in 20 to 30 minutes.
- Infarcts start in the subendocardial area.
- After several hours, a mid and subepicardial area of the myocardium is involved.
- After 3 to 6 hours, there is full infarct formation.
- Streptokinase injection can limit the infarct.
Changes in the myocardial infarction:
| Time period | Gross changes | Microscopic changes |
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
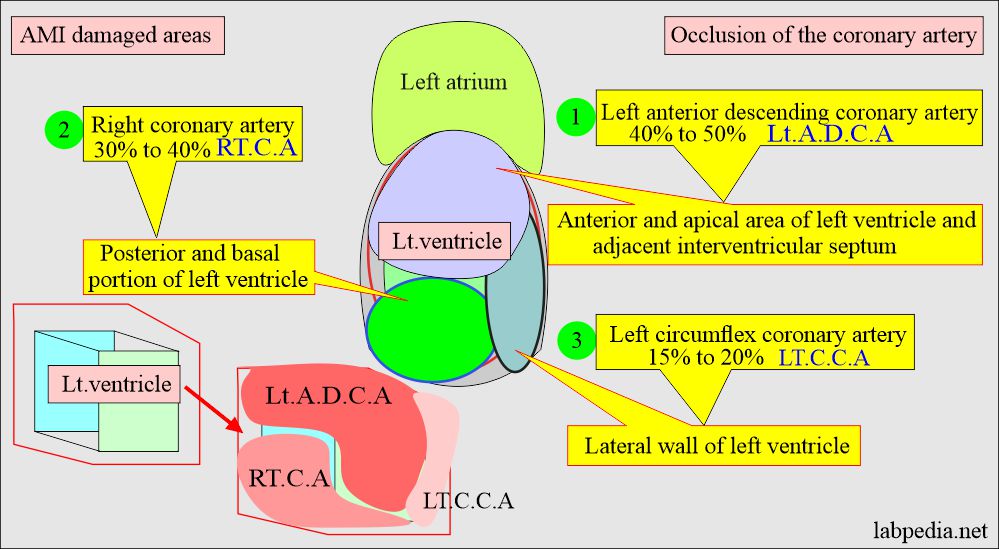
Distribution of the infarct:
- The ischemic necrosis involvement of the heart muscle depends upon the involvement of the anatomical blood vessel occlusion.
- The anterior left descending coronary artery involves the Anterior and apical part of the left ventricle and adjacent interventricular septum.
- The left circumflex coronary artery involves the Lateral wall of the left ventricle.
- The right coronary artery involves a Posterior and basal portion of the left ventricle.
Risk factors for Acute myocardial infarction (AMI) are:
- Family history is a very important factor.
- Physical activity, including walking or exercise.
- Lifestyle.
- Hypertension.
- Tobacco use.
- Weight (obesity), diet, and nutrition.
- Diabetes mellitus.
- Hyperlipidemia.
- High cholesterol.
- Sex is more common in males.
- More common in the case of family history.
Signs and symptoms of Acute myocardial infarction (AMI):
- Chest pain in the mid-thorax, and there is crushing substernal pain.
- Pain may radiate to teeth, jaw, shoulder, arm, or back.
- There may be dyspnea or shortness of breath.
- There may be sweating.
- There may be epigastric discomfort with or without nausea and vomiting.
- The patient may go into syncope.
- In 50% of patients, the AMI is preceded by angina pectoris.
- The pain of AMI is not relieved by nitroglycerin.
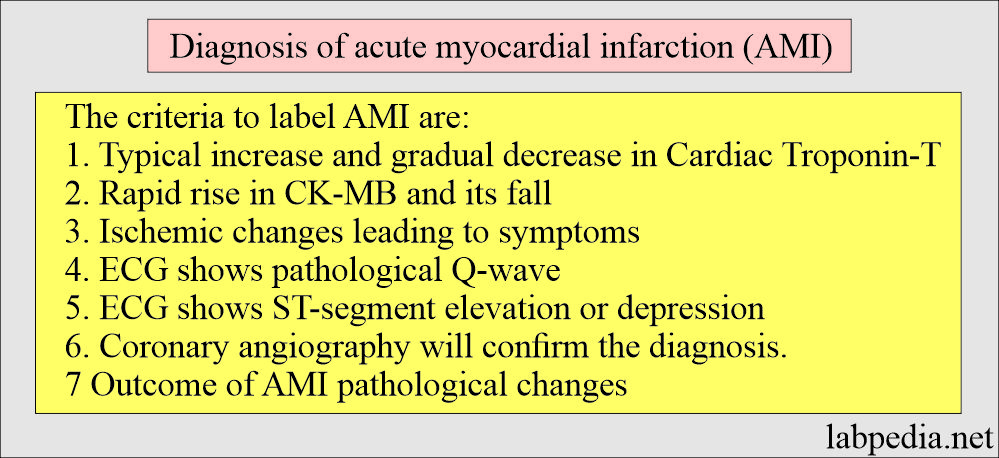
Acute Myocardial infarction is characterized by:
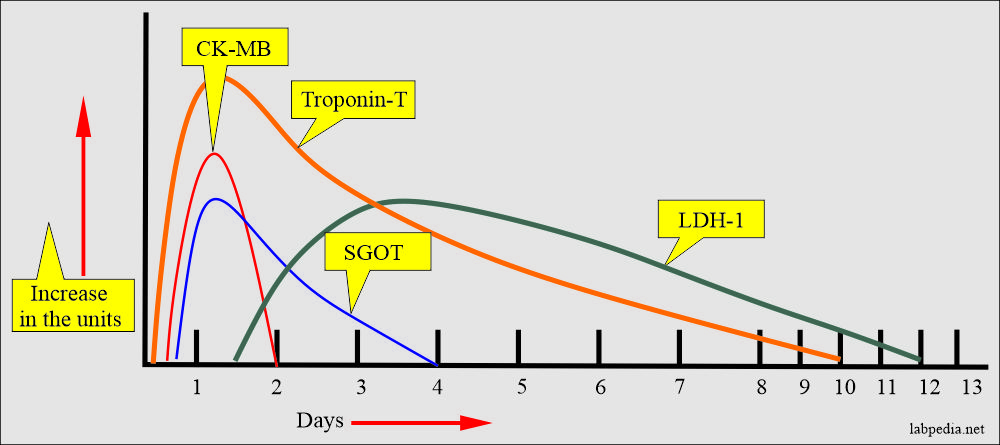
- The typical rise of CK-MB. The more rapid rise and fall of CK-MB.
- Raised level of Troponins. The more rapid rise and fall of Troponins.
- ECG changes.
- Development of Q-wave.
- ST-segment elevation.
- A coronary angiogram shows coronary artery abnormality.
Diagnose of acute Myocardial infarction (AMI):
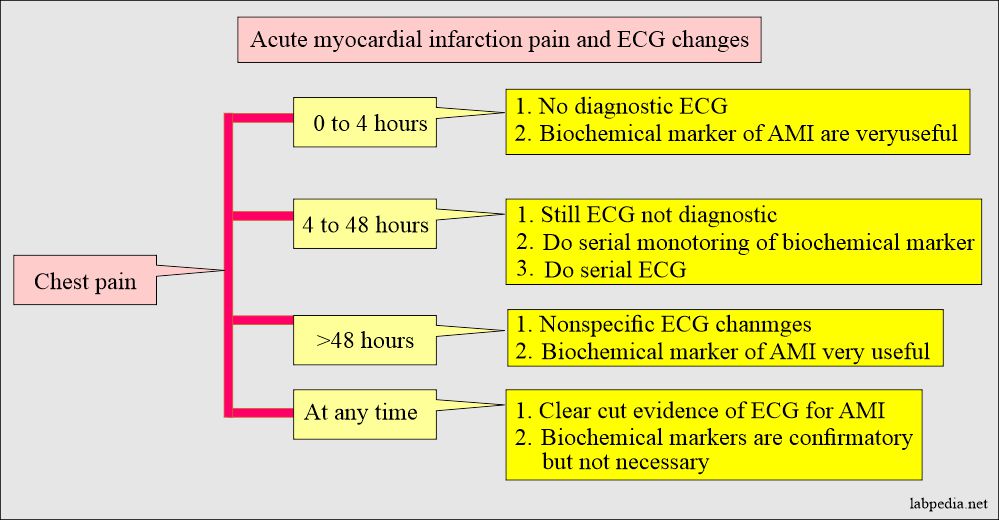
H/O chest pain:
- Chest pain may be typical in the case of AMI. This may be present in the left arm and may radiate to the mandible.
- This pain may be in the interscapular area, mimicking gallbladder pain.
- In some patients, there is silent AMI, which is most common in people with diabetes.
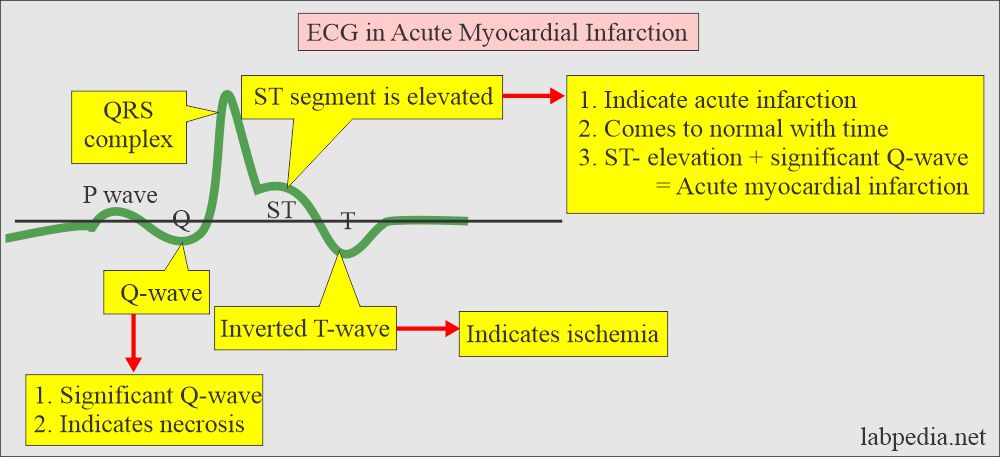
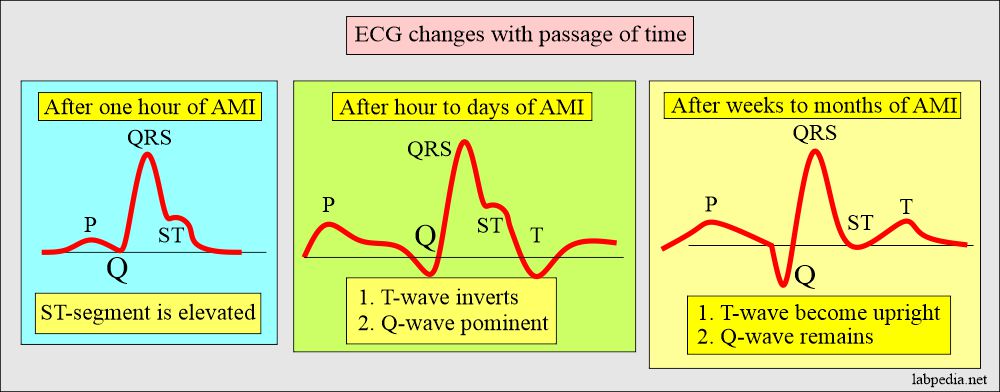
Changes in the ECG:
- The initial ECG is diagnostic in more than 50% of the cases.
- 15% of the cases show no initial changes in ECG.
- Follow-up for 24 hours shows positive ECG in 75% of the cases.
- These changes are reflected in the ST-segment, T-wave, and enlarged Q-wave.
- Initially, there is the elevation of the ST segment.
- Later on, Q-wave becomes prominent.
- After weeks to months, the ST segment becomes normal.
- T-wave also comes back to its original position.
- But Q-wave remains abnormal.
Abnormal cardiac enzymes:
- CK.
- CK-MB.
- LDH.
- Myoglobin.
- Troponin T and I.
- SGOT.
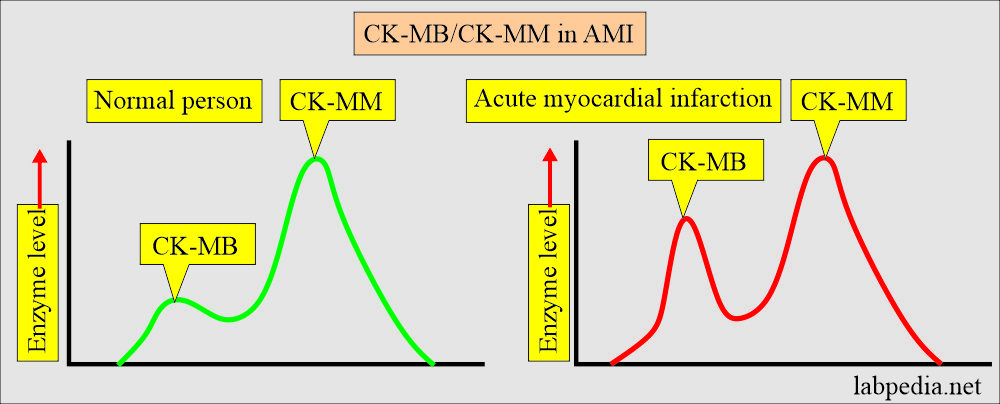
CK and CK-MB
- CK is found in the heart muscles, skeletal muscles, and brain.
- CK Can reflect the timing, quantity, and resolution of MI.
- CK has isoenzymes:
- CK-1 =BB = Found predominantly in the brain and lung.
- CK-2 =MB = Found predominantly in the cardiac muscles.
- CK-3 =MM = Found predominantly in the skeletal muscles.
- CK-MB is more specific for cardiac muscle injury.
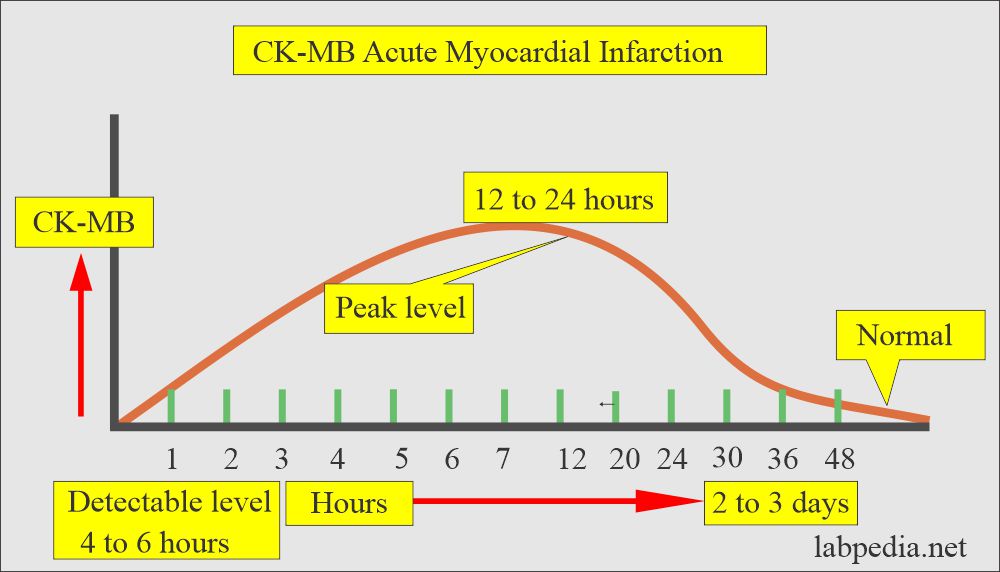
CK-MB interpretations:
- This also helps in quantifying and giving a degree of myocardial injury.
- If there is no further myocardial damage, then:
- CK-MB was detected in the first 3 to 6 hours.
- The peak level is at 20 to 24 hours.
- This returns to normal in 12 to 48 hours (another reference becomes normal in 72 hours).
- By 72 hours, 2/3 of the patients still show some increase in CK-MB.
- Sampling every 6 hours is more likely to find peak levels.
- Diagnosis of AMI is confirmed within 8 to 12 hours.
- Sampling beyond 24 hours is not advised.
- The single sample value is not diagnostic; serial estimation at least 4 hours apart shows ≥a 50% increase.
- Serial measurement is more important, and diagnosis reaches 100%.
- Total CK may be normal, but CK-MB will be raised.
- Raised CK-MB with normal total CK will represent patients with non-Q-wave AMI.
Disadvantages of CK-MB:
-
- A rapid return to normal makes it a poor marker.
- CK-MB is not as specific as Troponin, and there are false-positive reports of non-ischemic cardiac injuries like pericarditis and myocarditis.
- CK-MB is also positive in muscular dystrophy, exercise, and rhabdomyolysis.
- CK-MB usually does not arise in the case of angina, pulmonary embolism, or congestive heart failure.
- CK-MB may rise in case of shock, malignant hyperthermia, myopathy, or myocarditis.
- There is a small amount of CK-MB in the skeletal muscles.
- A case of severe skeletal muscle injury may give rise to a significantly high level of CK-MB.
- CK-MB is more helpful and more specific than Myoglobin when the patient comes with chest pain after 10 to 12 hours.
CK-MB relative index:
- This is done to avoid skeletal muscle injury with myocardial muscle damage.
- Calculation:
- CK-MB/total CPK
- Normal CK-MB/Total CPK index = <2.5.
- Examples:
- If CK-MB = 3.0 ng/mL
- Relative index = ≥2.5
- This is highly suggestive of myocardial injury.
- If CPK-MB = >3.0 ng/mL
- Relative index = <2.5
- Not diagnostic for myocardial injury.
- If CK-MB = 3.0 ng/mL
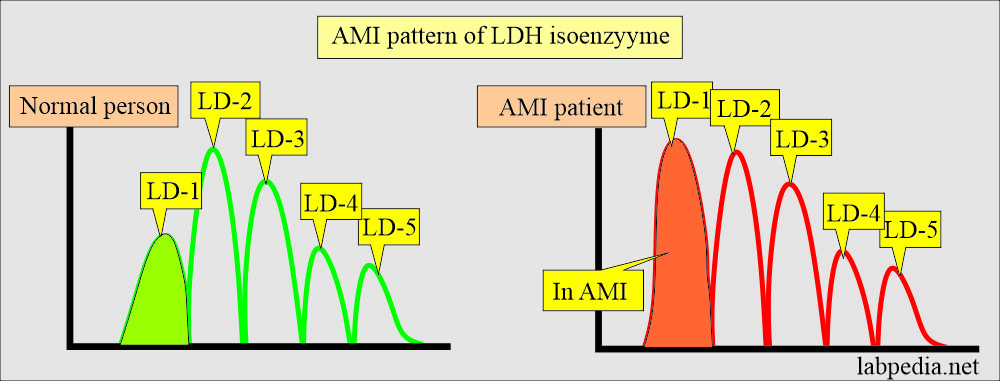
- Rises within 24 to 48 hours of Acute MI.
- The peak level is 2 to 3 days.
- Returns to normal in 5 to 10 days.
Lactate dehydrogenase (LDH):
Disadvantages of LDH:
- LDH has significance in other diseases like:
- The elevated level in the urine indicates malignancy or injury to the urinary system.
- LDH is also found in pleural, cardiac, or peritoneal effusions.
- When the effusion LDH/serum LDH ratio is >0.6, it indicates exudate in the effusion fluid.
- LDH is not tissue-specific because of its distribution throughout the body.
- It is raised in a variety of diseases, including myocardial injury.
- It is also not specific to cardiac diseases.
Myoglobin:
- Myoglobin is an oxygen-binding protein of the skeletal and cardiac muscles.
- Myoglobin is most sensitive to the cardiac marker and is the earliest marker of acute myocardial infarction.
- But this is the least cardio-specific of cardiac markers.
- This is cardiac and skeletal muscle protein. This can increase after trauma to skeletal muscle or cardiac muscle injury.
- This is not specific to cardiac muscle injury because it will rise even with there is a minor injury to skeletal muscle.
- It is raised in the trauma, inflammation, or ischemic changes to skeletal muscles.
- But Myoglobin is very sensitive to CK and CK-MB during the first hour of chest pain.
- It rises in the first 1 to 4 hours and is detectable in 6 to 9 hours.
- The peak level is at 8 to 12 hours.
- It becomes normal within 24 to 36 hours.
- Sensitivity is >95% within 6 hours of the appearance of the symptoms.
- It appears before the CK-MB around 2 to 5 hours.
- If Myoglobin remains within the reference range 8 hours after the start of chest pain, then essentially, Acute MI can be ruled out.
- Myoglobin is not recommended in patients with renal failure because they will have a raised level due to decreased kidney clearance.
- The disadvantage of myoglobin:
- A myoglobin sample is taken at a 1-hour interval.
- There is a wide range of the normal value from 6 to 90 ng/mL.
- Myoglobin displays a low specificity for AMI, as this is also raised in renal diseases, shock, open-heart surgery, skeletal muscle damage, and drastic exercise.
- This may also be raised in muscular dystrophy.
- Values are usually high in uremia and muscular trauma as compared to AMI.
SGOT
- This was the first enzyme marker for MI but lakes cardiac specificity, so it lost its value.
- SGOT sometimes raised in 90% to 95% of acute AMI.
- It is raised and found in the first 8 to 12 hours of heart muscle necrosis (ischemia), AMI.
- The peak level is 24 to 48 hours after the AMI attack.
- It falls to normal within 3 to 8 days.
- The disadvantage of SGOT:
- SGOT level does not correlate with tissue necrosis of the heart in AMI. There may be a minimal rise in the SGOT level.
- This may be raised in the case of liver cells, skeletal muscles, kidneys, and pancreas parenchymal cells injury.
- SGOT’s main drawback in diagnosing AMI is that it may be raised in many other conditions.
Hydroxybutaric acid dehydrogenase (HBD)
- It is used as a substitute for LDH-1.
- HBD indirectly measures LDH-1 (heart) activity.
- HBD is easy to measure and cheaper as compared to LDH isoenzymes.
- Once there are elevated cardiac enzymes, they may follow with HBD.
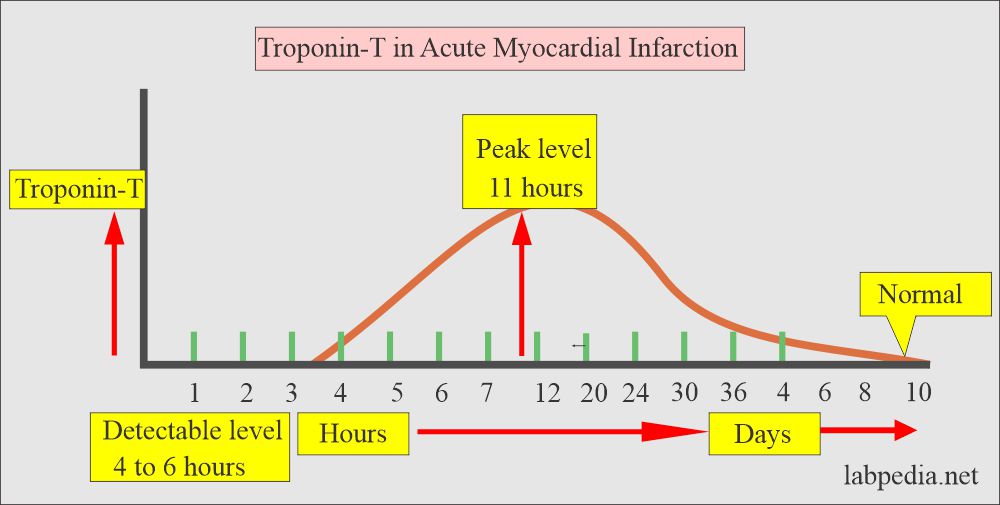
Troponin (Tn) T
- The troponin protein complex is situated on the thin filament of skeletal and cardiac muscles.
- Troponin is highly concentrated in cardiomyocytes.
- The role of Troponin is calcium-mediated contraction through its action with actin and myosin.
- Troponin complex can be separated by the monoclonal antibodies consisting of:
- TnT (Troponin – T) is a tropomyosin-binding subunit.
- TnI (Troponin – I) is the myosin ATPase inhibiting subunit that blocks the myosin movement without calcium.
- TnC (Troponin – C) is the calcium-binding subunit.
- Cardiac troponins are separated by the immunoassay with the help of monoclonal antibodies into:
- Troponin – T.
- Troponin – I.
- Troponin is localized in:
- Myofibrils are 94% to 97%.
- A cytoplasmic fraction is 3% to 6%.
- Troponin -T allows the early and late diagnosis of MI.
- The serum level remains raised beyond 7 days.
- It can be detected as early as 3 hours after the myocardial injury.
- Troponin -T remains elevated for 10 to 14 days.
- Troponin-I stays elevated for 7 to 10 days.
- The sensitivity of Troponin – T is 100% from 12 hours to 5 days after the chest pain.
- The raised level is also significant because it may go even up to 200 times.
- Serial measurement of Troponin-T and Troponin-I is advisable and specific for diagnosing AMI (myocardial damage).
- Raised levels of Troponin-T in unstable angina predict poor outcomes in some patients.
- Troponin measurement is better than LDH, particularly in patients who seek medical attention more than 24 to 48 hours after the onset of symptoms.
- Troponins are measured by:
- Monoclonal antibody immunoassay.
- Enzyme-linked immunoassay.
- Monoclonal sandwich antibody qualitative technique.
Advantage of Troponins over CK-MB:
| Characteristic features | Troponins | CK-MB |
|
|
|
|
|
|
|
|
|
|
|
|
Normal values of cardiac markers:
Source 1
- CK-MB = 0 to 3 ng/mL
- Or 0 to 3 µg/L
Source 2
- Troponin T = <0.2 ng/mL
- Troponin I = <0.3 ng/mL
Source 4
- Troponin-T = <0.2 ng/mL
- Or <o.2 µg/L
- Troponin-T = >1.0 ng/mL indicates current myocardial injury.
- Troponin-I = <0.35 ng/mL
- Or <0.35 µg/L
- LDH = 140 to 280 U/L
- LDH = 300 to 800 U/L indicates myocardial infarction.
- Myoglobin = <55 ng/mL (25 to 72 ng/mL or 1.28 to 3.67 nmol/L)
- SGOT (AST) = Adult male = 5 to 40 U/L
- Slightly lower in the female.
- HBD = Male = 150 to 300 units/100 mL (Rosalki-Wilkerson)
- Female = 95 to 210 units/100 mL (Rosalki-Wilkerson)
- (55 to 125 units by Sigma)
- Female = 95 to 210 units/100 mL (Rosalki-Wilkerson)
Table of cardiac markers:
| Marker | Time to rise in the blood (hours) | When detectable in the blood (Hours) | Peak | Days to become normal |
|---|---|---|---|---|
| Creatine Kinase | 5 to 8 | 6 to 8 | 24 to 36 hours | 3 to 4 days |
| CK -MB | 5 to 15 | 4 to 6 | 12 to 24 hours | 2 to 3 days |
| LDH | 2 to 4 | 8 to 12 | 2 to 4 days | 8 to 14 days |
| Myoglobin | 1 to 3 | 1 to 3 | 6 to 9 hours | 1 day |
| Troponin I | 4 to 6 | 3 to 8 | 10 to 24 hours | 3 to 10 days |
| Troponin T | 3 to 4 | 3 to 8 | 10 to 24 hours | 5 to 10 days |
| AST (SGOT) | 3 to 5 | 6 to 8 | 24 to 48 hours | 4 to 6 days |
- Thrombolytic therapy is helpful if applied within the first 12 hours of AMI.
- Note: You may find some differences in these tests to become normal in different references.
Critical values
- Troponin-I = >1.5 ng/mL (>1.6 µg/L)
- Troponin-T = >0.1 µg/L
- CK-MB = >5% or >10 µg/L
Questions and answers:
Question 1: Which test is more specific for AMI?
Question 2: What is the significance of myoglobin for the diagnosis of AMI?