Carboxyhemoglobin (CO-Hb), Carbon Monoxide (CO) Poisoning
Carboxyhemoglobin (CO-Hb)
Sample for Carboxyhemoglobin (CO-Hb)
- Collect the venous blood immediately when CO poisoning is suspected.
- Heparinized arterial or venous blood for spectrophotometric methodology.
- Because CO is rapidly cleared from the hemoglobin when the patient is exposed to fresh air.
- Whole blood in heparin is stable >4 months infilled well-caped bottle.
- Blood in EDTA anticoagulant is stable at room temperature for over a week.
Precautions for Carboxyhemoglobin
- Don’t use oxalate for the blood sample.
- Collect the blood sample before oxygen therapy is started.
- O2 saturation and oximetry are inaccurate in the CO-poisoning because it measures all forms of O2 – saturated hemoglobin and CO-Hb.
Purpose of the test (Indications) for Carboxyhemoglobin (CO-Hb)
- This test is done to detect carbon monoxide poisoning.
- It is prescribed for patients who are exposed to smoke inhalation, exhaust fumes, and fires.
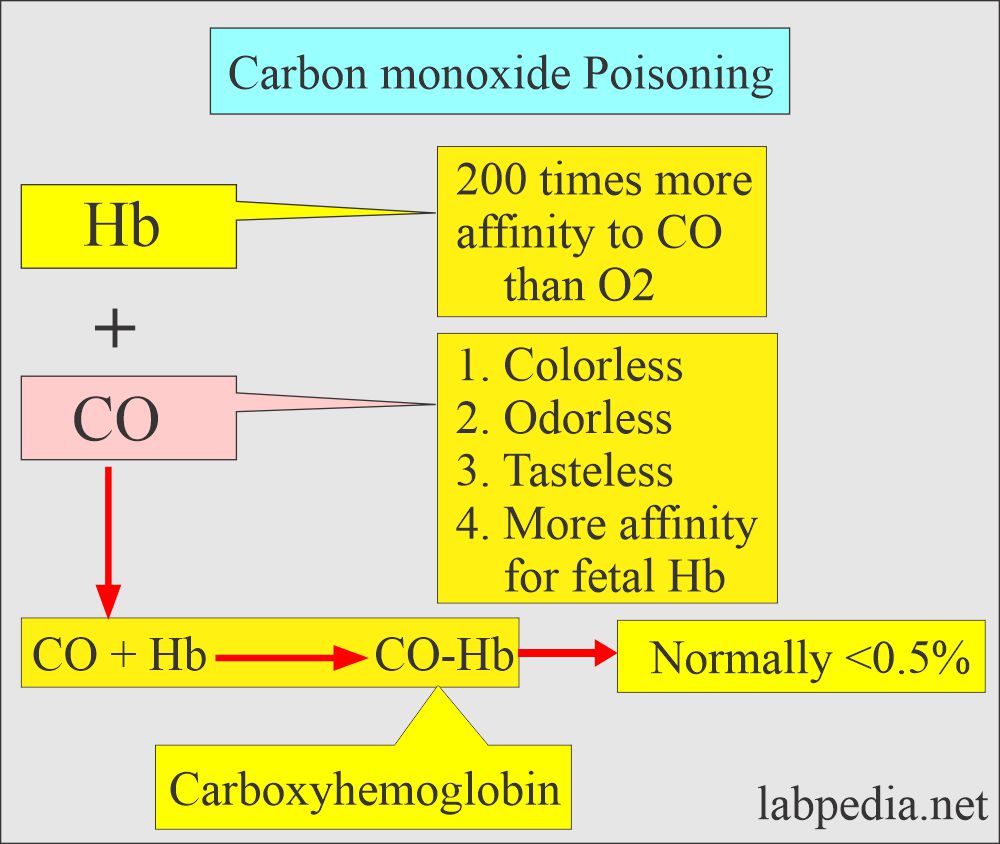
Pathophysiology of Carboxyhemoglobin (CO-Hb)
Definition of Carboxyhemoglobin:
- Carbon monoxide (CO) is colorless, odorless, and tasteless, undetectable unless mixed with a visible or odorous pollutant.
- Carboxyhemoglobin (CO-Hb) is produced by the incomplete combustion of fuels such as gasoline.
- Carbon monoxide (CO) binds more tightly with hemoglobin than O2. It displaces the O2 and causes hypoxia.
- Carbon monoxide (CO) is a chemical agent which produces hypoxic injury due to O2 deprivation.
- There is Cherry red skin is a good clue for Carbon monoxide poisoning.
Carboxyhemoglobin (CO-Hb) Poisoning mechanism:
- Carbon monoxide (CO) is produced in the environment where there is partial combustion of Carbon-containing fossil fuels.
- Complete oxidation leads to the production of CO2.
- Carbon monoxide (CO) combines with hemoglobin with 200 times more affinity than oxygen.
- CO + Hb = CO-Hb
- CO-Hb produces a cherry-red or violet color on the skin.
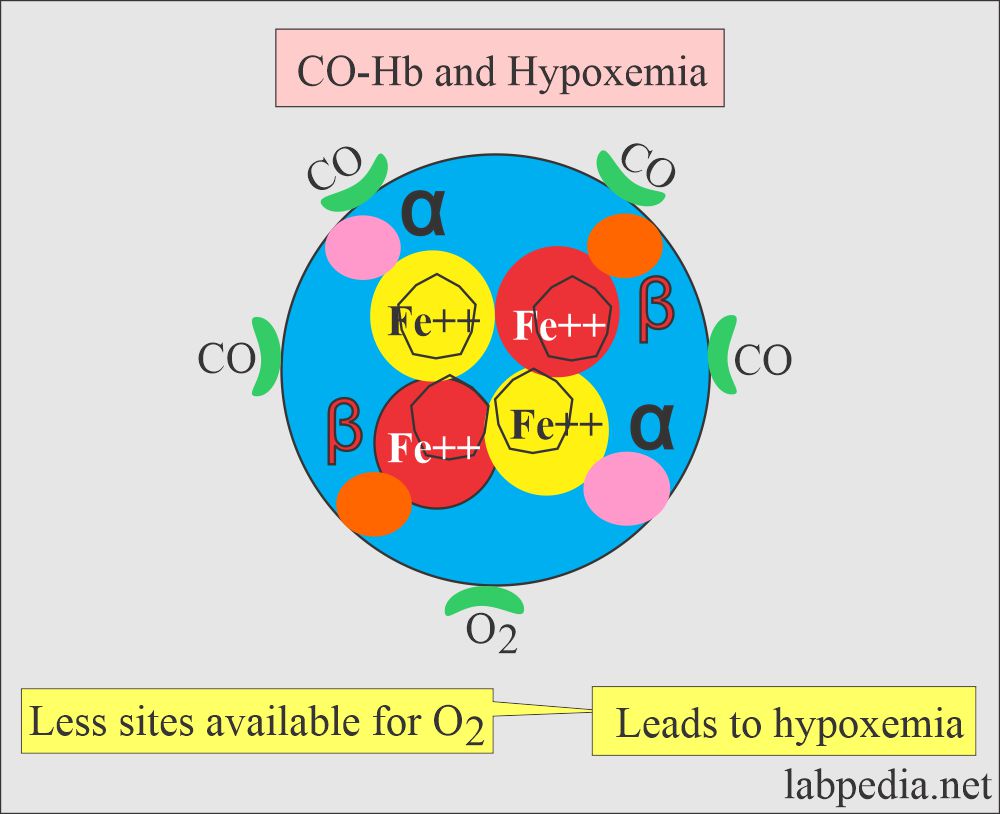
- So in the presence of CO, few sites are available for O2 to combine with Hb.
- Less O2 is available for tissue respiration leads to Hypoxemia because CO-Hb cannot transport O2.
- CO has a high affinity for hemoglobin, almost 210 times that of oxygen.
- CO will combine with the hemoglobin and form carboxyhemoglobin (CO-Hb).
- Normally carboxyhemoglobin (CO-Hb) is a small fraction of the total hemoglobin <0.5%.
- CO-Hb at a higher level leads to toxic symptoms.
- CO poisoning is directly toxic to the intracellular oxidative mechanism and produces more nitric oxide (NO).
- When CO poisoning takes place, ask for Hb analysis for CO-Hb.
- CO is readily cleared by breathing normal air.
- Fetal Hb has more affinity for CO, and if these fetuses are exposed to CO, they are more at risk.
Sources of carbon monoxide (CO) are:
- Newborn where the fetal Hb breakdown yields endogenous CO.
- Tobacco smoke.
- Automobile exhaust fumes.
- Natural gas heaters where there is less ventilation.
- Industrial pollution like:
- Coal gas.
- Charcoal burning.
- Tobacco smoke.
- Defective gas stoves.
- Petroleum and natural gas fuel fumes.
- Endogenous production of the CO:
- It is produced from the heme, and the CO-Hb level is ≥1% ( 0.2% to 0.8%).
- It is increased in hemolytic anemia and smokers.
- Bleeding in the intestine.
- In smokers, it may vary from 4% to 20%.
- In the case of smokers exposed to CO may have CO-Hb of around 10%.
- CO is also produced in the liver by metabolizing dichloromethane (methyl chloride), which is found in paints and varnish.
- People who are prone to get CO-poisoning:
- In defective furnaces.
- A worker such as a coal miner.
- The firefighter.
- Smokers of cigarettes, cigars, or pipes in the closed space.
- Accidental poisoning was most often seen in house fires, engine exhaust (car left starting in the closed garage), indoor heaters, and stoves.
- Unventilated spaces where charcoal and gas are burning are the source of poisoning during winter power outages.
- Intentional CO poisoning is common in suicide cases.
- The half-life of elimination of CO is about 4 hours for a person breathing atmospheric air.
- But for smokers, this level may remain high.
Signs and symptoms of Carbon monoxide (CO) poisoning:
- The brain and the heart are more prone to be affected by CO.
- Chronic exposure to CO may lead to polycythemia.
- CO-Hb produces cherry-red color on the blood and skin.
- There is a direct relationship between CO and heart disease, angina, and myocardial infarction symptoms.
- This CO poisoning occurs from house fires, gas heaters, stoves, and engine exhausts.
- 30% to 40% of carboxyhemoglobin contents are associated with severe symptoms.
- >50% is associated with coma.
- Cigarette smoking may produce levels as high as 10% to 15%.
- There are nausea and weakness.
- There is a headache, dizziness, and vomiting.
- Tinnitus is ringing in the ears.
- It upsets the stomach.
- The patient may have chest pain.
- The patient will be confused.
- Drunk or sleeping people may die due to CO poisoning.
Carbon monoxide % level effects on the body:
| Carbon monoxide (CO) level | Clinical presentation of the patient |
|
|
|
|
|
|
|
|
|
|
Various levels of Carboxyhemoglobin (CO-Hb) % and clinical effects on the body:
| Carboxyhemoglobin (CO-Hb)-Saturated Hb % | Signs and Symptoms |
|---|---|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
Symptoms are correlated with % of carbon monoxide (CO) poisoning:
| Carbon-monoxide % | Clinical presentation |
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
Measurement (Lab diagnosis) of CO poisoning:
- For CO estimation, we can use venous or arterial blood.
- CO-oximeter measures CO.
- A blood gas analyzer measures oxyhemoglobin by calculation.
- Lactate can be measured.
- Calculation of the anion gap.
- Check myocardial markers.
The normal level of carboxyhemoglobin
Source 1
- CO-Hb = <0.5% of total hemoglobin.
- Newborn = up to 5 % saturation of total Hb.
- Nonsmoker = <3 % saturation of total Hb.
- Smoker Light = 2% to 5 % saturation of total Hb.
- Smoker heavy = 5% to 10 % saturation of total Hb.
- Critical value = >20 % saturation of total Hb.
- Lethal value = >50 % saturation of Hb.
Source 2
| Clinical condition | % saturation of Hb |
|
|
| Smokers | |
|
|
|
|
| Toxic level | |
|
|
|
|
Source 3
Saturation of hemoglobin by carbon monoxide (CO)
- Nonsmoker = <3%
- Smoker = ≤ 12%
- Newborn = ≥ 12%
Source 2
Clinical values and their effects:
| CO-Hb % | Clinical signs and symptoms |
|
|
|
|
|
|
|
|
Source 4
- Nonsmoker = <2% of total Hb.
- Light smoker = 4 to 5% of total Hb.
- Heavy smoker = 6 to 8% of total Hb.
- Newborn = 10 to 12% of the total Hb.
Another source
- Smoker = 2.1% to 4.2%
- Nonsmoker = <2.3%
Increased level of CO:
- This is 50% to 60% seen in CO poisoning.
Lab findings in CO- poisoning:
- Whole blood with heparin or EDTA as an anticoagulant is used.
- The specimen should be mixed thoroughly before performing the test.
- Blood pH is decreased, leading to metabolic acidosis due to tissue hypoxia.
- Arteria Oxygen (pO2) is normal. Oxygen (O) is markedly decreased.
- Arterial pCO2 may be normal or slightly decreased.
- Confirm the carbon monoxide (CO) in the exhaled breath.
Treatment:
- CO- toxicity needs a high concentration of O2 to replace the CO-Hb.
- In the case of severe CO, toxicity may be treated with hyperbaric oxygen (100% O2 gas).
Questions and answers:
Question 1: What is the fatal level of CO-Hb?
Question 2: What is the affinity of the hemoglobin with Carbon monoxide (CO)?