Carboxyhemoglobin (CO-Hb), Carbon Monoxide (CO) Poisoning
Carboxyhemoglobin (CO-Hb)
What sample is needed for Carboxyhemoglobin (CO-Hb)?
- Collect the venous blood immediately when CO poisoning is suspected.
- Heparinized arterial or venous blood for spectrophotometric methodology.
- Because CO is rapidly cleared from the hemoglobin when the patient is exposed to fresh air.
- Whole blood in heparin is stable for more than 4 months in a well-capped bottle.
- Blood in EDTA anticoagulant is stable at room temperature for over a week.
What are the precautions for Carboxyhemoglobin?
- Don’t use oxalate for the blood sample.
- Collect the blood sample before starting oxygen therapy.
- O2 saturation and oximetry are inaccurate in CO poisoning because they measure all forms of O2, including O2-saturated hemoglobin and CO-Hb.
What are the Indications for Carboxyhemoglobin (CO-Hb)?
- This test is done to detect carbon monoxide poisoning.
- It is prescribed for patients who are exposed to smoke inhalation, exhaust fumes, and fires.
How will you define Carboxyhemoglobin?
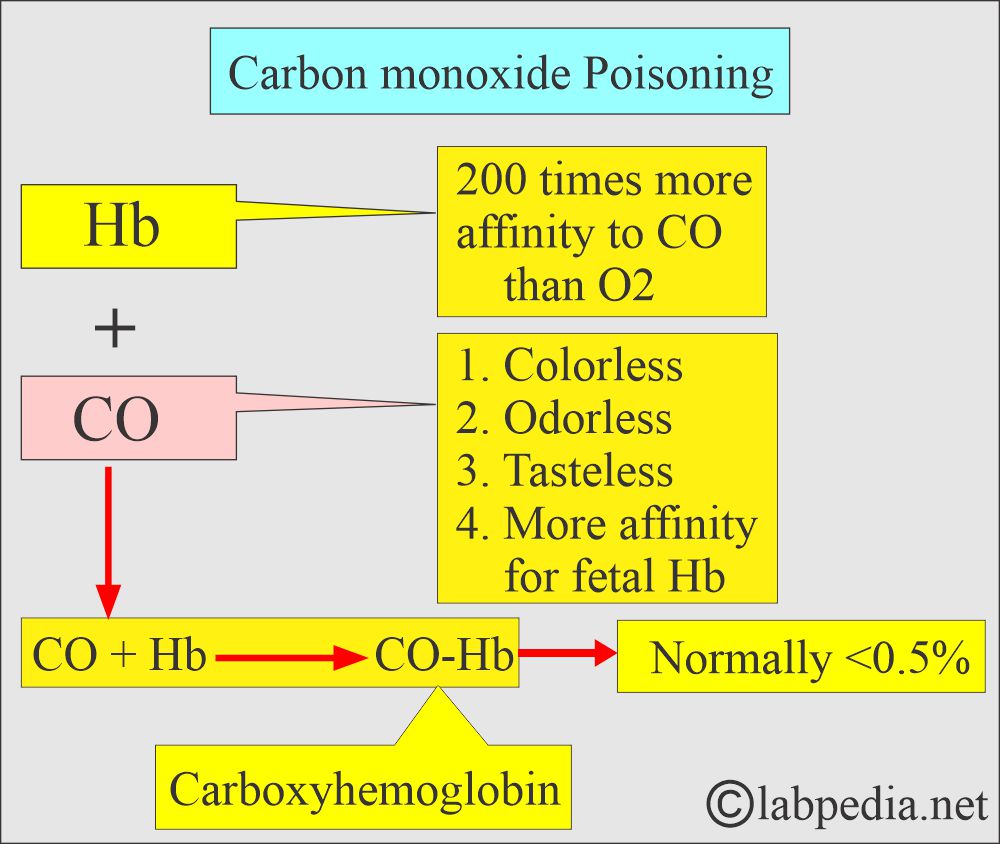
- Carbon monoxide (CO) is colorless, odorless, and tasteless, undetectable unless mixed with a visible or odorous pollutant.
- The incomplete combustion of fuels such as gasoline produces carboxyhemoglobin (CO-Hb).
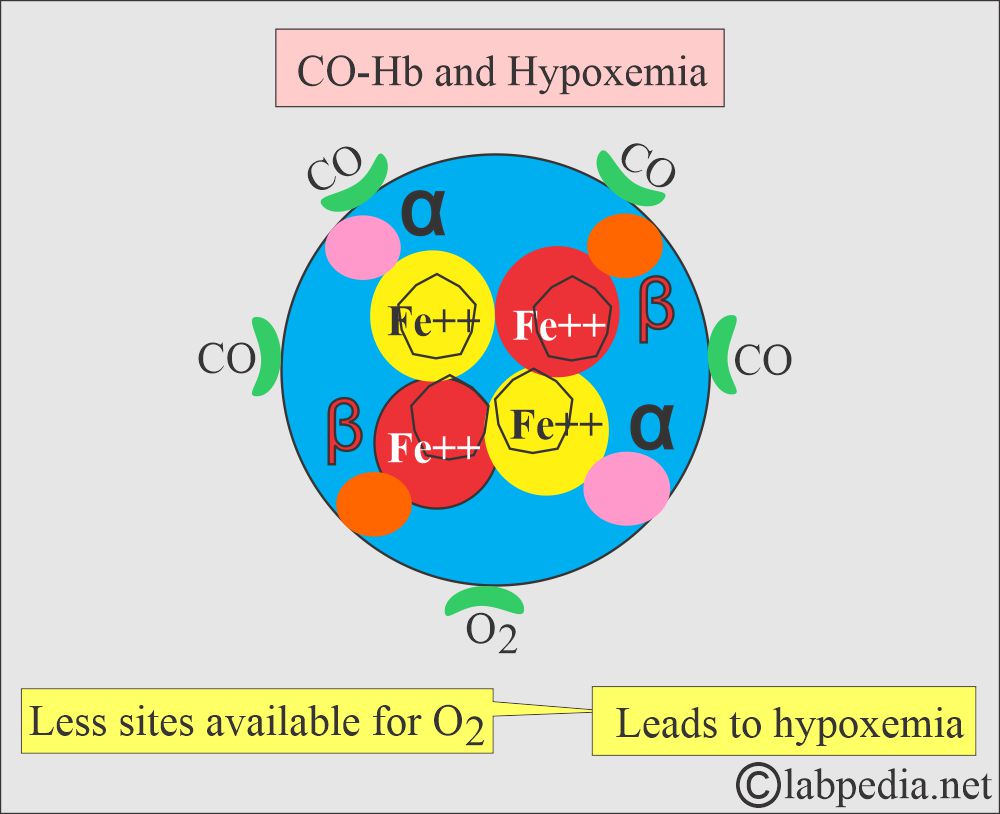
- Carbon monoxide (CO) binds more tightly with hemoglobin than O2. It displaces the O2 and causes hypoxia.
- Carbon monoxide (CO) is a chemical agent that produces hypoxic injury due to O2 deprivation.
- Cherry-red skin is a good clue for Carbon monoxide poisoning.
What is the mechanism of Carboxyhemoglobin (CO-Hb) poisoning?
- Carbon monoxide (CO) is produced in the environment where there is partial combustion of carbon-containing fossil fuels.
- Complete oxidation leads to the production of CO2.
- Carbon monoxide (CO) combines with hemoglobin with 200 times more affinity than oxygen.
- CO + Hb = CO-Hb (200 times more affinity than oxygen).
- CO-Hb produces a cherry-red or violet color on the skin.
- In the presence of CO, few sites are available for O2 to bind to Hb.
- Less O2 is available for tissue respiration, leading to Hypoxemia because CO-Hb cannot transport O2.
- CO has a high affinity for hemoglobin, almost 210 times that of oxygen.
- CO will combine with the hemoglobin and form carboxyhemoglobin (CO-Hb).
- Normally, carboxyhemoglobin (CO-Hb) is a small fraction of the total hemoglobin <0.5%.
- CO-Hb at a higher level leads to toxic symptoms.
- CO poisoning is directly toxic to the intracellular oxidative mechanism and produces more nitric oxide (NO).
- When CO poisoning occurs, request a Hb analysis for CO-Hb.
- CO is readily cleared by breathing normal air.
- Fetal Hb has more affinity for CO, and if these fetuses are exposed to CO, they are more at risk.
What are the sources of carbon monoxide (CO)?
- Newborns, where the fetal Hb breakdown yields endogenous CO.
- Tobacco smoke.
- Automobile exhaust fumes.
- Natural gas heaters are used in areas with limited ventilation.
- Industrial pollution includes:
- Coal gas.
- Charcoal burning.
- Tobacco smoke.
- Defective gas stoves.
- Petroleum and natural gas fuel fumes.
- Endogenous production of the CO:
- It is produced from heme, and the CO-Hb level is ≥1% (0.2% to 0.8%).
- It is increased in hemolytic anemia and in smokers.
- Bleeding in the intestine.
- In smokers, it may vary from 4% to 20%.
- In the case of smokers exposed to CO, they may have CO-Hb of around 10%.
- CO is also produced in the liver by metabolizing dichloromethane (methyl chloride), which is found in paints and varnishes.
- People who are prone to poisoning:
- In defective furnaces.
- A worker, such as a coal miner.
- The firefighter.
- Smokers of cigarettes, cigars, or pipes in a closed space.
- Accidental poisoning was most often seen in house fires, engine exhaust (such as a car left running in a closed garage), indoor heaters, and stoves.
- Unventilated spaces where charcoal and gas are burning are the source of poisoning during winter power outages.
- Intentional CO poisoning is common in suicide cases.
- The half-life of CO elimination is approximately 4 hours for a person breathing atmospheric air.
- But for smokers, this level may remain high.
What are the signs and symptoms of Carbon monoxide (CO) poisoning?
- The brain and the heart are more susceptible to the effects of CO.
- Chronic exposure to CO may lead to polycythemia.
- CO-Hb produces a cherry-red color on the blood and skin.
- There is a direct relationship between CO and heart disease, angina, and myocardial infarction symptoms.
- This CO poisoning occurs from house fires, gas heaters, stoves, and engine exhausts.
- A carboxyhemoglobin content of 30% to 40% is associated with severe symptoms.
- A 50% association is noted with coma.
- Cigarette smoking may produce levels as high as 10% to 15%.
- There is nausea and weakness.
- There is a headache, dizziness, and vomiting.
- Tinnitus is ringing in the ears.
- It upsets the stomach.
- The patient may have chest pain.
- The patient will be confused.
- Drunk or sleeping people may die due to CO poisoning.
What are the effects of Carbon monoxide % levels on the body?
| Carbon monoxide (CO) level | Clinical presentation of the patient |
|
|
|
|
|
|
|
|
|
|
What are the various levels of Carboxyhemoglobin (CO-Hb) % and clinical effects on the body?
| Carboxyhemoglobin (CO-Hb)-Saturated Hb % | Signs and Symptoms |
|---|---|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
What symptoms are correlated with % of carbon monoxide (CO) poisoning?
| Carbon-monoxide % | Clinical presentation |
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
How will you do a Lab diagnosis of CO poisoning?
- For CO estimation, we can use venous or arterial blood.
- CO-oximeter measures CO.
- A blood gas analyzer measures oxyhemoglobin by calculation.
- Lactate can be measured.
- Calculation of the anion gap.
- Check myocardial markers.
What is the normal level of carboxyhemoglobin (CO-Hb)?
Source 1
- CO-Hb = <0.5% of total hemoglobin.
- Newborn = up to 5 % saturation of total Hb.
- Nonsmoker = <3 % saturation of total Hb.
- Smoker Light = 2% to 5 % saturation of total Hb.
- Smoker heavy = 5% to 10 % saturation of total Hb.
- Critical value = >20 % saturation of total Hb.
- Lethal value = >50 % saturation of Hb.
Source 2
| Clinical condition | % saturation of Hb |
|
|
| Smokers | |
|
|
|
|
| Toxic level | |
|
|
|
|
Source 3
Saturation of hemoglobin by carbon monoxide (CO)
- Nonsmoker = <3%
- Smoker = ≤ 12%
- Newborn = ≥ 12%
Source 2
What are the clinical values and their effects due to Carboxyhemoglobin?
| CO-Hb % | Clinical signs and symptoms |
|
|
|
|
|
|
|
|
Source 4
- Nonsmoker = <2% of total Hb.
- Light smoker = 4 to 5% of total Hb.
- Heavy smoker = 6 to 8% of total Hb.
- Newborn = 10 to 12% of the total Hb.
Another source
- Smoker = 2.1% to 4.2%
- Nonsmoker = <2.3%
What is the cause of the increased level of CO?
- This is 50% to 60% seen in CO poisoning.
What are the Lab findings in CO poisoning?
- Whole blood, with heparin or EDTA as the anticoagulant, is used.
- The specimen should be mixed thoroughly before performing the test.
- Blood pH is decreased, leading to metabolic acidosis due to tissue hypoxia.
- Arterial Oxygen (pO2) is normal. Oxygen (O) is markedly decreased.
- Arterial pCO2 may be normal or slightly decreased.
- Confirm the carbon monoxide (CO) in the exhaled breath.
How will you treat CO poisoning?
- CO-toxicity needs a high concentration of O2 to replace the CO-Hb.
- In the case of severe CO, toxicity may be treated with hyperbaric oxygen (100% O2 gas).
Questions and answers:
Question 1: What is the fatal level of CO-Hb?
Question 2: What is the affinity of the hemoglobin with Carbon monoxide (CO)?