C-Reactive Protein (CRP), High-Sensitivity C-Reactive Protein (hs-CRP), Acute Phase Protein
Acute-phase protein (Acute Phase Reactants)
- Acute-phase proteins are raised in inflammatory conditions; these may be called:
- Acute inflammatory response pattern.
- Acute stress pattern.
- Acute-phase protein pattern.
- Acute stress pattern.
- When there is an increase in an acute-phase protein called positive acute-phase protein.
- In the case of a decrease in the acute phase protein, it is called the negative phase protein.
- The acute phase proteins (positive) are proteins whose concentration increases in the plasma, and after the disease episode is over, it decreases and may become normal.
C-Reactive Protein (CRP)
Sample for C-Reactive Protein (CRP)
- The venous blood of the patient is needed to prepare the serum.
- A fasting sample is preferred.
- A random sample can be taken.
- Analyze the fresh sample.
- Or it can store at 4 °C for <72 hours.
- At -20 °C for six months.
Indications for C-Reactive Protein (CRP)
- Advised in bacterial infection.
- It is advised for rheumatic fever.
- It is advised in rheumatoid arthritis.
- It may be advised after the surgery.
- This is done in inflammatory diseases like acute rheumatic fever, rheumatoid arthritis, and bacterial infection.
- It will help in the diagnosis of coronary artery disease.
- This test can be done to diagnose bacterial endocarditis.
- To diagnose appendicitis.
- To diagnose active collagen vascular diseases.
Precautions for C-Reactive Protein (CRP)
- This may be raised in cigarette smoking.
- Avoid hemolysed and lipemic samples.
- Raised values are seen in hypertension, diabetes mellitus, metabolic syndrome, gingivitis, and bronchitis.
- Decreased values have seen weight loss, moderate consumption of alcohol, and exercise.
- Estrogens and progesterone increase the C-Reactive Protein (CRP).
- Niacin, statin, and fibrates decrease the C-Reactive Protein (CRP).
- Keep in mind that:
- Cigarette smoking may increase the level.
- Estrogen and progesterone may increase the level.
- Niacin and statin may decrease the value.
- There may be an increased level of CRP in hypertension, diabetes mellitus, and metabolic syndrome.
- Avoid lipemic or hemolyzed samples.
Definition of C-Reactive Protein (CRP):
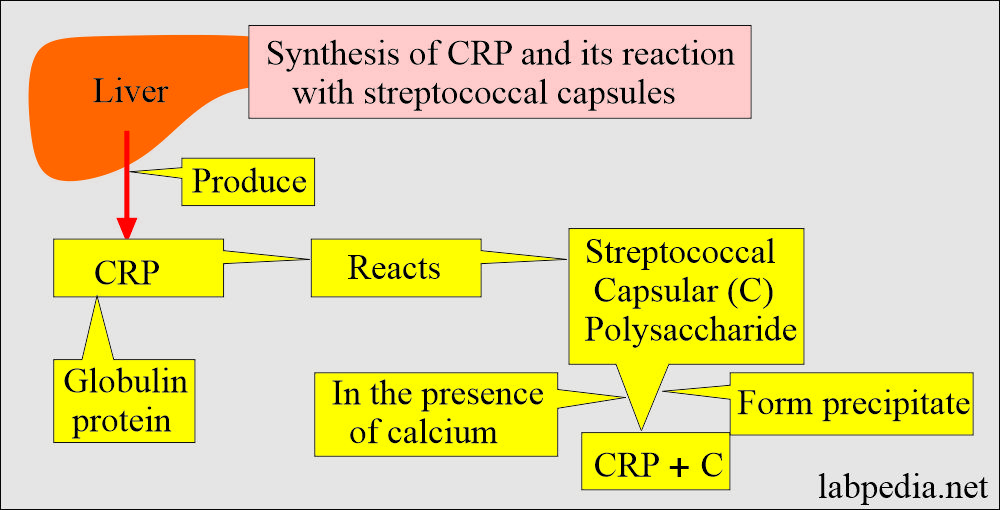
- CRP is produced in the liver, and its name is derived from its reaction with streptococcal capsular polysaccharides (capsule).
- CRP level supporting the diagnosis of bacterial endocarditis, appendicitis, and active collagen diseases was >10 mg/L.
- There are changes in the plasma protein in response to:
- Acute illness.
- Trauma.
- Necrosis.
- Infarction.
- Burns.
- Chemical injury.
- Malignant tumors.
- The acute reaction proteins pattern is also called:
- Acute inflammatory response pattern.
- Acute stress pattern.
- Acute-phase protein pattern.
History of C-Reactive Protein (CRP):
- In 1930 Tillet and Francis found substance in the sera of acutely ill patients.
- CRP was given its name in 1941 because it is a protein.
- This substance binds the C-polysaccharides cell wall of Strept. pneumomiae.
- This leads to the agglutination of the bacteria.
- In 1940, this substance was shown to be a protein called C-reactive protein (CRP).
- Its detection limit for infection and autoimmune diseases was 3 to 8 mg/L.
- CRP molecular weight is ∼115 kDa.
- It is synthesized in the liver and has little or no carbohydrates.
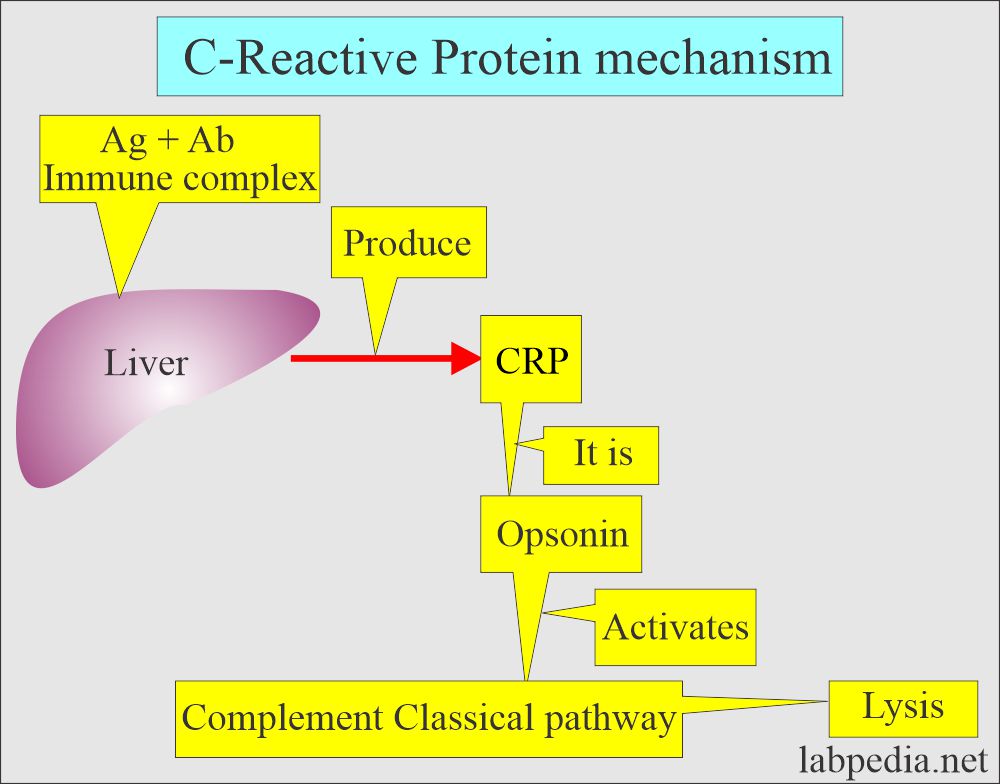
Mechanism of action of C-Reactive Protein (CRP):
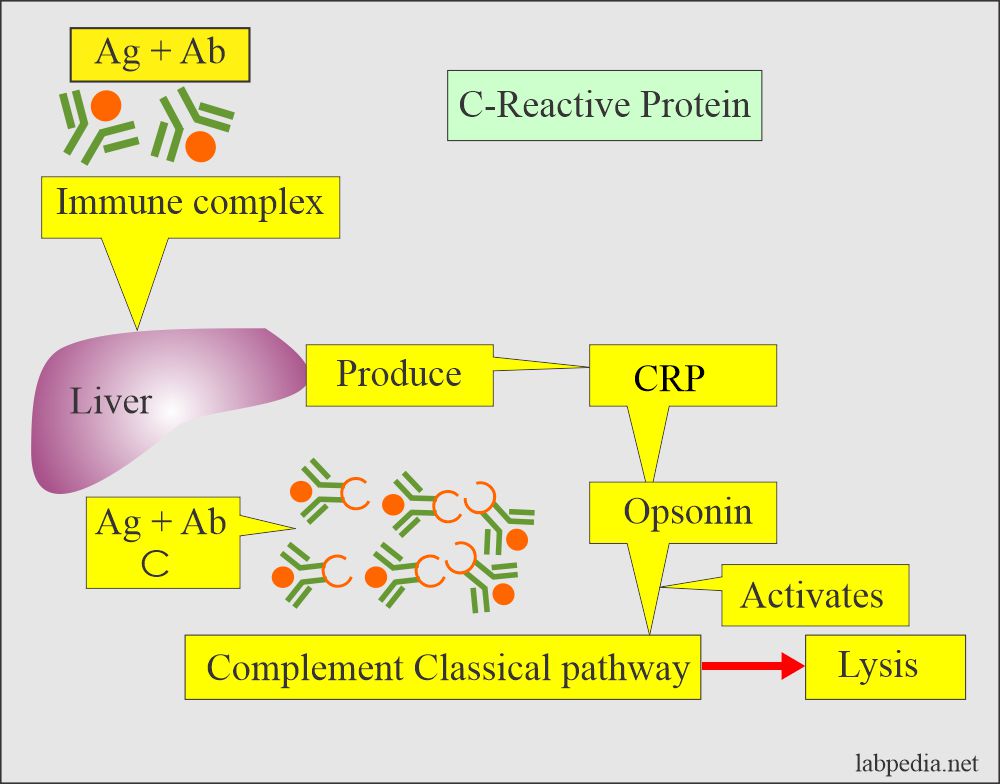
- It binds the C-polysaccharide of streptococcus pneumoniae and agglutinates the bacteria.
- This complex CRP is a potent opsonin for monocytes, leading to phagocytosis and activating the complement system.
- It activates the classical complement pathway.
- It binds to polysaccharides present in many bacteria, fungi, protozoal parasites, and histones.
- Its production is under the control of IL-1 and IL-6.
Pathophysiology of C-Reactive Protein (CRP)
- The C-reactive protein name originates from its reaction with streptococcal capsular (C) polysaccharides.
- CRP is the fastest-responding acute-phase protein, increasing 100 times with infection.
- So this is the most sensitive indicator.
- This increases in many diseases, so this has no specificity.
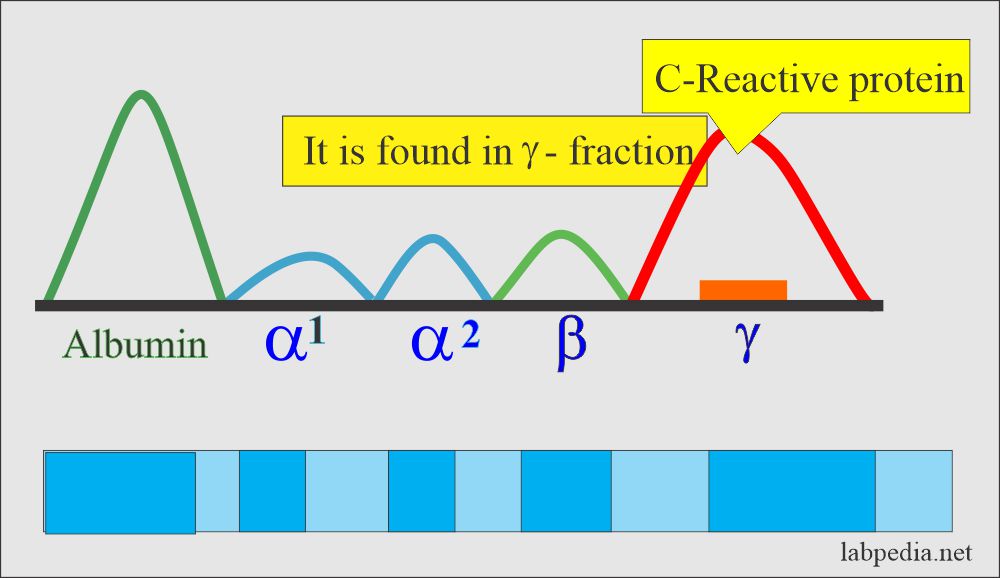
- This is a nonspecific acute-phase protein with gamma mobility and is very helpful in monitoring inflammation.
- C-reactive protein on serum electrophoresis is found in the gamma region.
- CRP is synthesized in the liver, and antigen complexes initiate its synthesis.
-
- Its production is controlled by interleukin-6.
-
- CRP forms complex on the surface of bacteria (E.coli, S.pneumoniae), fungi, and other microorganisms.
- CRP binds to polysaccharides present in many bacteria, fungi, protozoal parasites, and histones.
- It is found in the Gamma-region band on serum electrophoresis.
C-Reactive protein (CRP) pattern:
- CRP is absent from a healthy person.
- CRP increased after any injury (trauma, bacterial infection, surgery, neoplasm, and inflammation) to 100 times.
- This is a nonspecific acute-phase protein.
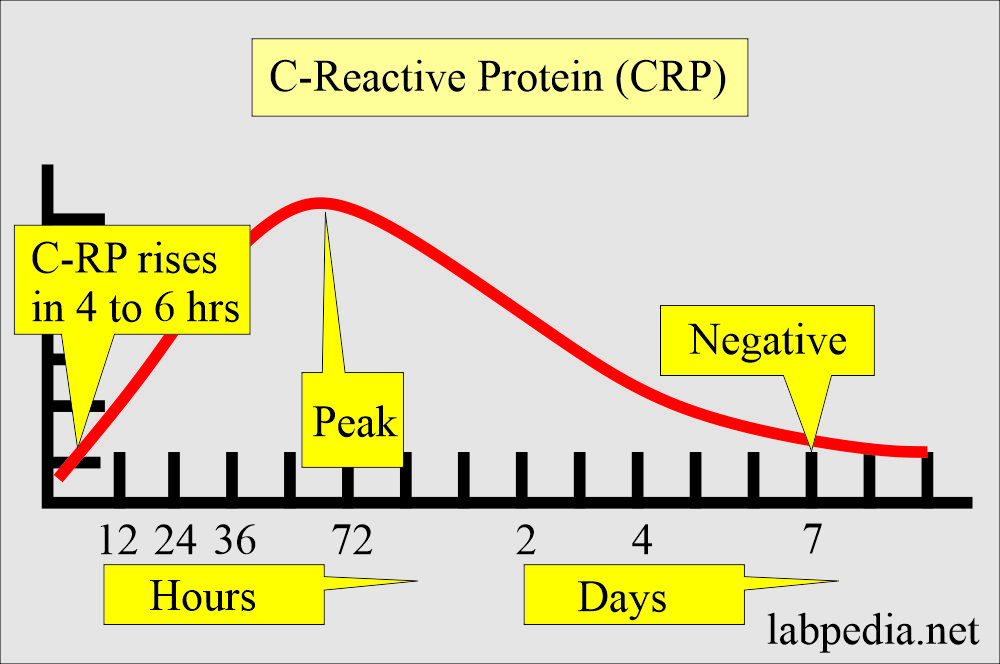
- CRP rises after 4 to 6 hours of the infection (within 24 hours), while other proteins rise after 12 to 36 hours of the initiating cause.
- The peak level is at 72 hours.
- C-Reactive Protein (CRP) becomes negative after 7 days.
Synthesis of C-Reactive Protein (CRP) curve:
- CRP is functionally analogous to IgG, except it is not antigen-specific.
- This protein is synthesized in the liver and released into blood circulation after tissue injury in a few hours.
- The synthesis of the CRP is initiated by:
- Antigen immune complexes.
- Bacterial infection.
- Fungal infection.
- Trauma or tissue injury.
High-sensitivity CRP (hs-CRP):
- hs-CRP is produced in the liver and is an acute phase reactant.
- It is induced by the release of interleukins 1 and 6; these interleukins reflect systemic inflammation activation.
- It detects the lower level of CRP, which is important for finding the risk of cardiac events.
- The sensitivity is 0.01 mg/dL.
- In the case of raised hs-CRP, follow-up serial measurements are needed.
- hs-CRP is useful for the risk of developing acute myocardial infarction with a history of acute coronary syndrome.
- Value ≥1.0 mg/L indicates subclinical infection/inflammation; the test must be repeated in 3 to 4 weeks.
Coronary risk grades:
| hs-CRP level | Degree of risk for cardiovascular diseases |
|
|
|
|
|
|
C-Reactive Protein (CRP) and its significance:
- It is the first acute-phase protein raised in inflammatory diseases, and its level increases tremendously.
- It is raised in acute and chronic inflammation.
- This promotes the binding of Complements and helps in phagocytosis.
- The antigen-antibody immune complex initiates the C-Reactive Protein (CRP) formation.
- Failure of the CRP to return to normal indicates tissue damage in the heart or elsewhere.
- The absence of CRP increase raises the question of necrosis prior 2 to 10 days.
- CRP is usually normal in unstable angina patients where there is no necrosis.
- CRP may remain increased for at least 3 months after Acute myocardial infarction (AMI).
- Peak CRP correlates with the peak of CK-MB in AMI.
- This can induce the production of cytokines.
- This can cause inhibition of chemotaxis and modulation of the WBC function.
- The average CRP level is <2 to 3 mg/L.
- The markedly raised level of >10 mg/L indicates an active inflammatory condition like collagen disease and infection.
- Its level does not rise consistently in the virus infection.
CRP vs. ESR:
- More sensitive and rapidly responding than the ESR.
- Other physiologic factors influence ESR, but CRP does not.
- CRP tends to increase before the increase in ESR and antibody titer.
- CRP shows an earlier and more rapid increase in the acute inflammatory process than ESR.
- In recovery, it becomes normal before the ESR.
- It disappears when the disease is treated with cortisone or salicylates.
- This is useful for assessing the risk of myocardial infarction in patients with acute coronary signs and symptoms.
| Parameters | CRP | ESR |
| Normal level | <1.0 mg/L | Men = 0 to 5 women = 5 to 15 mm/Hour |
| Sensitivity of the test | More sensitive | Less sensitive |
| Pathophysiology (Etiology) | Dead and dying tissue release chemical factors, which stimulate the liver to produce CRP (IL1 and IL6) | Fibrinogen level goes up in the serum, which causes RBCs to clump |
| Rise of the test | Earlier increase | Late increase |
| Influence of other physiological factors | Not affect | Affected |
| Relation to antibody titer | Increase before antibodies | No relation to antibody |
| In acute inflammation | Early increase | Late increase |
| In recovery stage | Becomes normal early | Becomes normal late |
| AMI | Best indicator | No relation |
| Anginal attack | Normal | No relation |
| After the surgery | A good relationship with recovery | No relation |
| Bacterial meningitis | The normal level excludes meningitis | No relation |
C-Reactive protein role in various diseases:
CRP may be an indicator of various diseases like:
- Tissue injury or necrosis of the tissues.
- Various infections.
- Monitoring course and effect of therapy.
In myocardial infarction (AMI):
- CRP is raised, and it correlates with CK-MB isoenzyme in AMI.
- Its peak level occurs 1 to 3 days later than CK-MB.
- hs-CRP values >10 mg/L within 6 to 24 hours after the symptom onset indicates an increased risk for a recurrent cardiac event within 30 days to 1 year.
- In unstable angina, hs-CRP values >10 mg/L will predict a higher chance of myocardial infarction/death than in patients with hs-CRP <10 mg/L.
- CRP may remain increased in AMI for at least three months.
- If the level persists, being raised indicates ongoing damage to myocardial tissue.
- The baseline level is a good marker for future cardiovascular disease.
- CRP is a strong predictor of cardiovascular diseases than the low-density-lipoprotein (LDL) and cholesterol.
- CRP is a good marker for assessing the likelihood of recurrent myocardial infarction, restenosis, or death in patients with stable coronary disease.
- Its raised level is also reported as a risk factor for the development of hypertension.
- Its level is normal in the case of angina.
In Pancreatitis:
- A level of 150 mg/L distinguishes mild from severe acute pancreatitis.
Rejection phenomenon:
- It helps rejection of kidney or bone marrow transplants but is not helpful in heart transplants.
Malignant tumors:
- In 1/3 of the cases, CRP is >10 mg/L in malignant tumors of the breast, lungs, and GI tract.
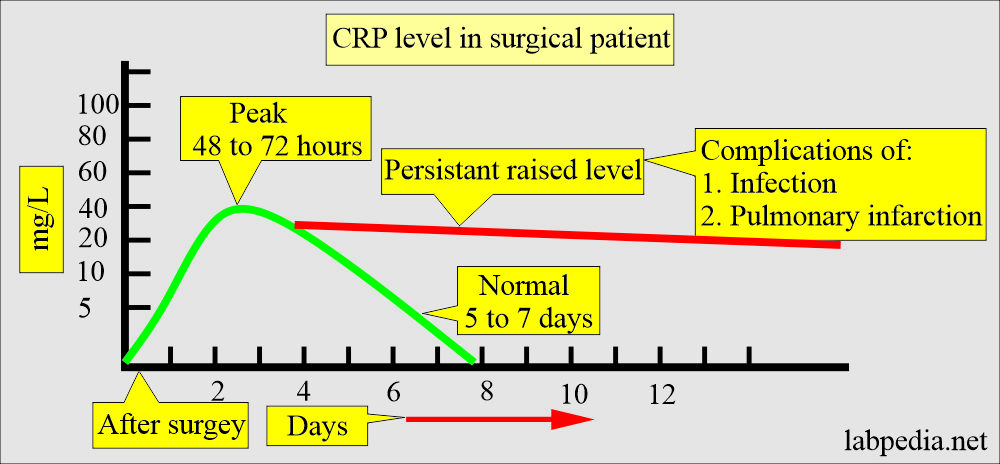
After surgery:
- It may be advised after the surgery when it’s level increases in 4 to 6 hours.
- The peak level reaches 48 to 72 hours.
- It starts going down after a 3rd postoperative day.
- It returns to normal in 5 to 7 days.
- Failure to return to a normal level raised level indicates a complication of infection or pulmonary infarction.
- In that cases, advise CBC, ESR, temperature check, and pulse rate.
Meningitis:
- It helps in the differential diagnosis of bacterial or viral meningitis.
- In viral meningitis, it will not be raised.
- The normal value excludes bacterial meningitis.
In burns,
- The level may exceed 1000 mg/L.
CRP level is useful in:
- Clinical evaluation of SLE, Leukaemia, Blast crisis, and ulcerative colitis.
- There is a good correlation with ESR, but CRP appears and disappears earlier than changes in ESR.
- The level of CRP increases dramatically than other Acute-phase proteins. So CRP is more useful as acute-phase protein.
- The quantitative test is more useful than a qualitative test.
Jones criteria for the diagnosis of Rheumatic fever:
| Manifestations | Signs and symptoms |
| Major | Polyarthritis, carditis, subcutaneous nodule, chorea, Erythema marginatum |
| Minor | Fever and arthralgia |
| Minor | Raised CRP, raised ESR, evidence of group A streptococcal infection, and prolonged PR interval on ECG |
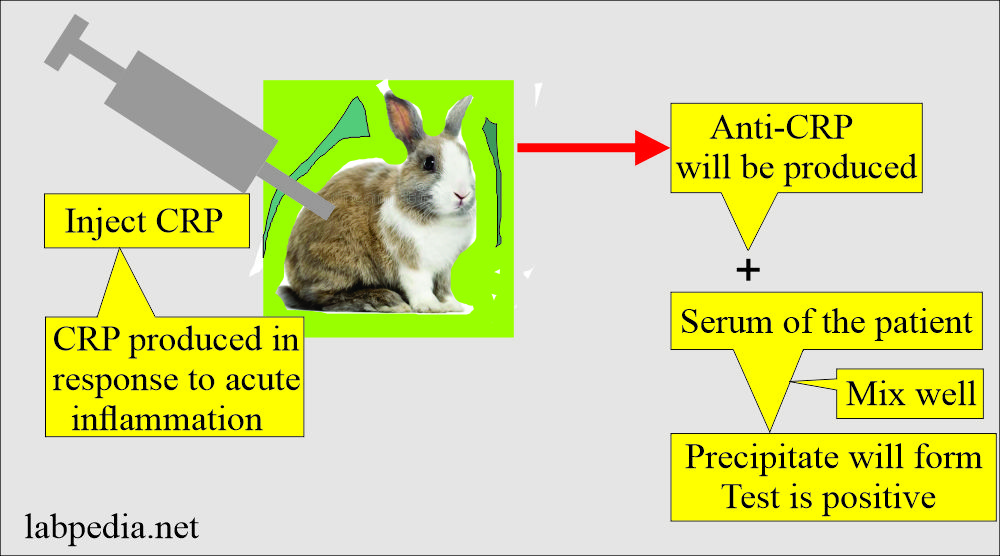
Serology of CRP:
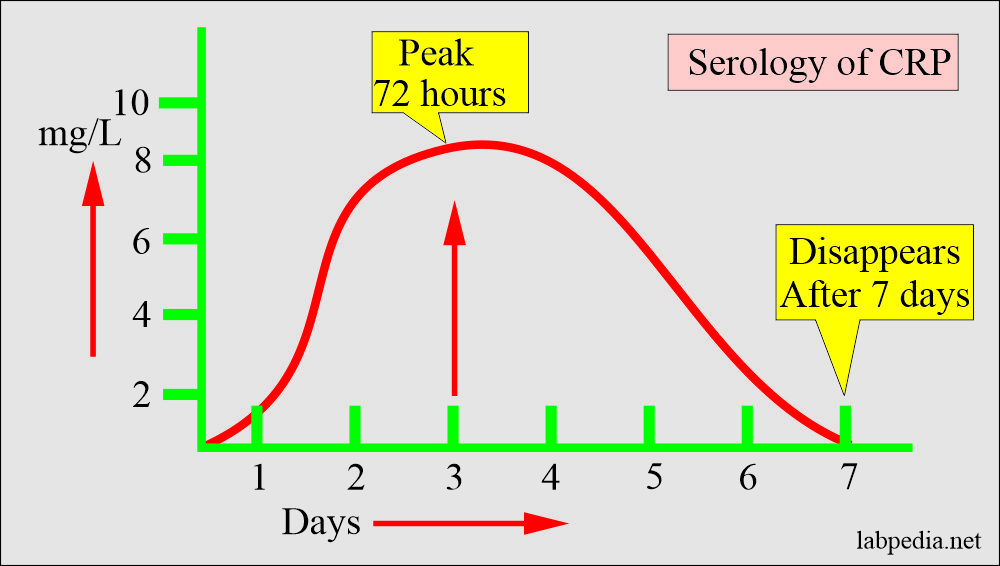
- CRP appears 24 to 48 hours after the onset of infection.
- The peak level reaches 72 hours.
- It disappears from circulation after seven days.
- Based on the CRP level, there are the following categories:
- Normal level = <3 mg/L.
- High-level CRP = >10 mg/L (active inflammation).
- Low-level CRP = 3 to 10 mg/L. (Cellular stress).
Normal C-Reactive Protein (CRP)
- <1.0 mg/dL
- Source 2
- <1.0 mg/dL or <10.0 mg/L
- Cardiac disease risk:
- Low = <1.0 mg/dL
- Average = 1.0 to 3.0 mg/dL
- High = >3.0 mg/dL
- Source 4
- CRP = <0.8 mg/dL (<8.0 mg/L) (by nephelometry)
- CRP reportable value = 0.3 to 20 mg/dL
- hs-CRP = 0.020 to 0.800 mg/dL (o.2 to 8.0 mg/L) (by immunoassay)
- Value ≥1.0 mg/L represents subclinical infection/inflammation and should be repeated in 3 to 4 weeks.
The raised level is seen in:
- Soft tissue Trauma.
- Infection.
- Tissue necrosis.
- Patients with Rheumatoid arthritis.
- In Rheumatic fever.
- Patients with systemic lupus erythematosus.
- Patient with pneumonia.
- Patient with malignancies.
- In pregnant ladies.
- Pulmonary tuberculosis.
- Urinary tract infection.
- Myocardial infarction.
- Vasculitis syndrome.
- Bacterial meningitis.
Decreased CRP level is seen in:
- This may be seen in the moderate use of alcohol.
- In weight loss.
- Strenuous exercise.
- Medicine like Niacin and statin.
- Pregnancy.
- Angina.
- Seizures.
- Asthma.
- Common cold.
- Rejection of heart transplant.
- Autoimmune diseases like SLE, scleroderma, dermatomyositis, and mixed connective tissue disease.
The panic value of hs-CRP
- >3.5 mg/L
- In acute inflammation = >10.0 mg/L
Questions and answers:
Question 1: When is the peak level of CRP in infection?
Question 2: Is there any value of CRPP in post-surgery?


Excelente articulo! Muchas gracias!
Thanks for the encouraging remarks
thank u very much sir
Thanks a lot.