C-Peptide, Insulin, Proinsulin and Interpretations
C-Peptide, Insulin, Proinsulin
What sample is needed for C-Peptide?
- Venous blood is collected to prepare the serum.
- A fasting sample is needed.
- Glucose samples should also be taken simultaneously.
- Keep the blood at 4 °C.
- Stable for 30 days when frozen.
- A urine 24-hour sample is needed.
- Neutralize the urine to pH 7.0 to 7.5.
- It can be stored at -15 °C.
What are the precautions for C-Peptide?
- As most of the C-peptide is degraded in the kidneys, renal failure will increase the level of C-peptide.
- Take H/O drugs that may increase the level of hypoglycemic agents (sulfonylureas).
- Oral hypoglycemic agents may increase the C-peptide level.
What are the Indications for the C-Peptide test?
- This test is done to evaluate diabetic patients.
- This test is the best tool for the diagnosis of hypoglycemia.
- It provides a reliable indication of pancreatic secretory function and insulin secretion.
- It is helpful to diagnose an Insulinoma (a Tumor of the islets of Langerhans).
- It is advised for the follow-up of a patient treated for insulinoma.
- To find patients injecting exogenous insulin.
- The C-peptide level can be used to diagnose insulin resistance syndrome.
- It is helpful for patients with pancreatectomy, where it will be undetectable.
How will you define C-Peptide?
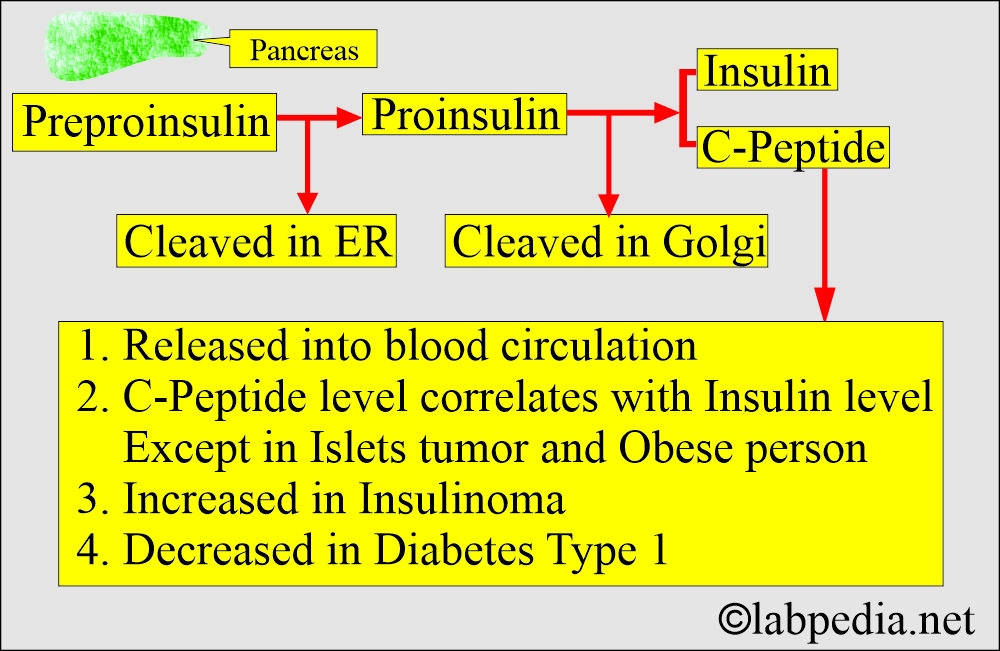
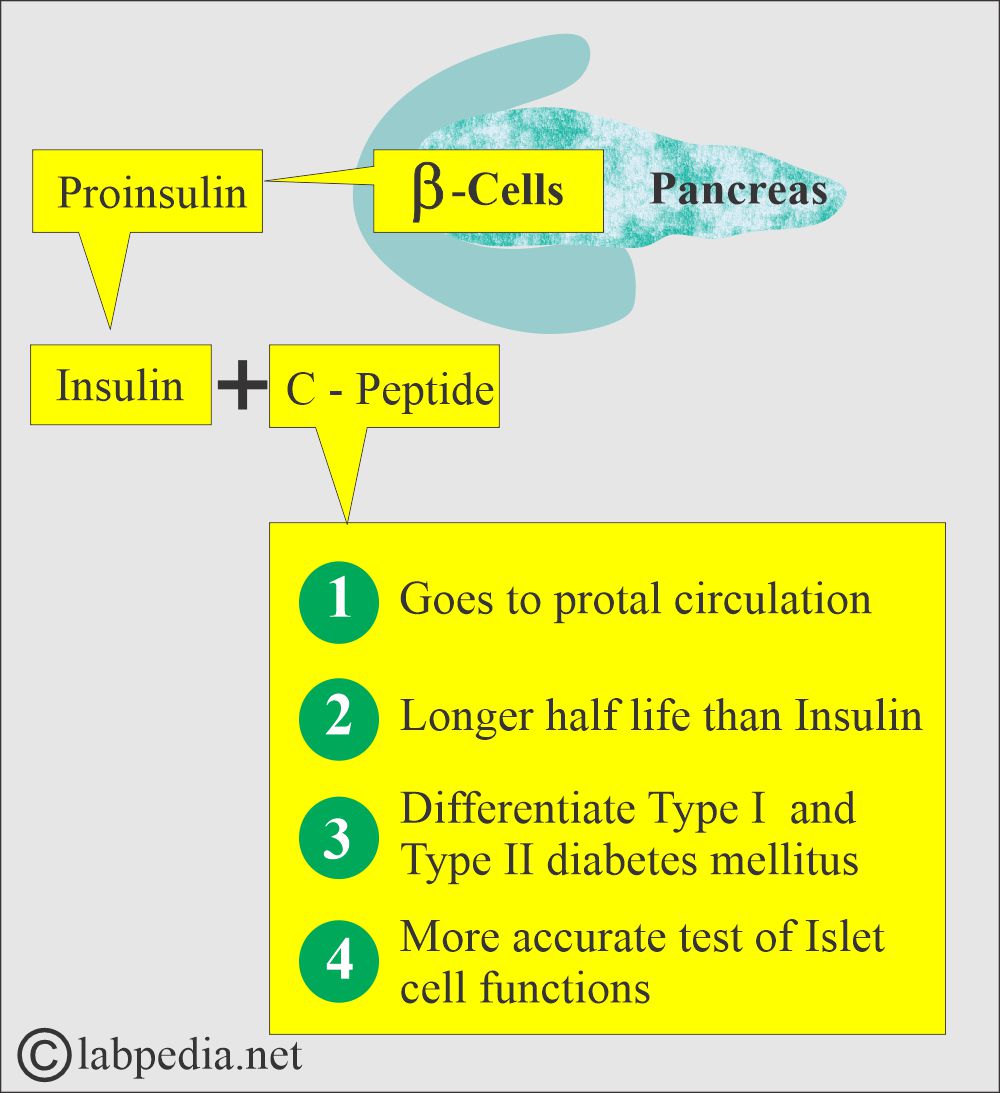
- Proinsulin is converted into insulin and C-peptide.
- C-peptide is released into the bloodstream.
- C-peptide serum levels correlate with insulin levels in the blood, except in cases of islet cell tumors and possibly in obese patients.
How will you discuss the pathophysiology of C-peptide?
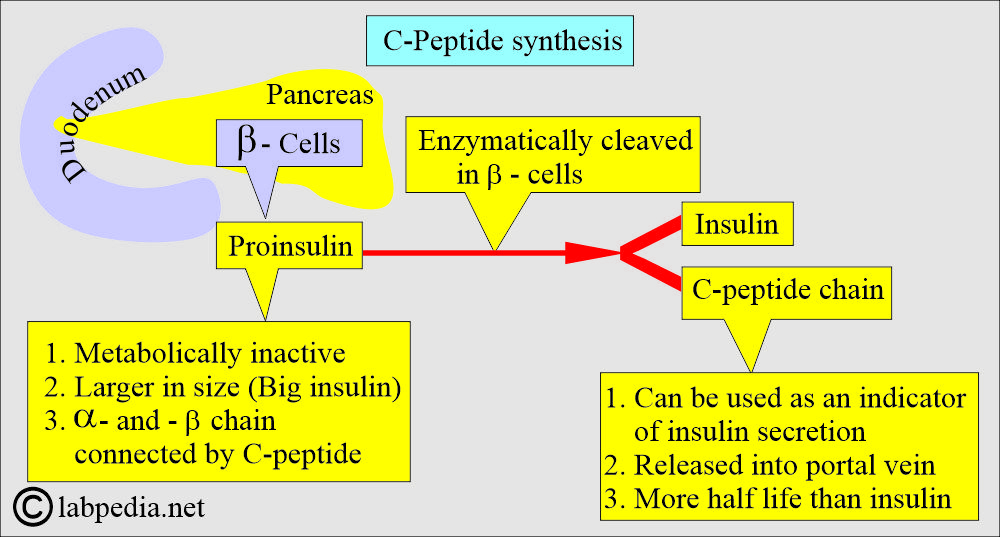
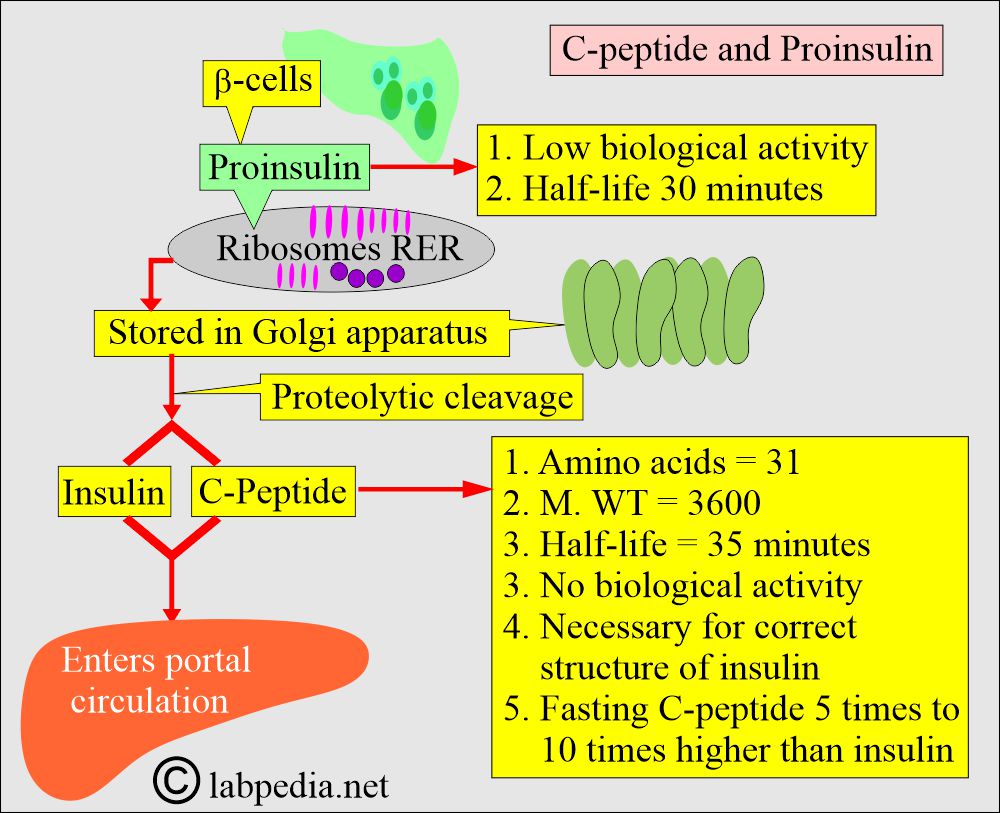
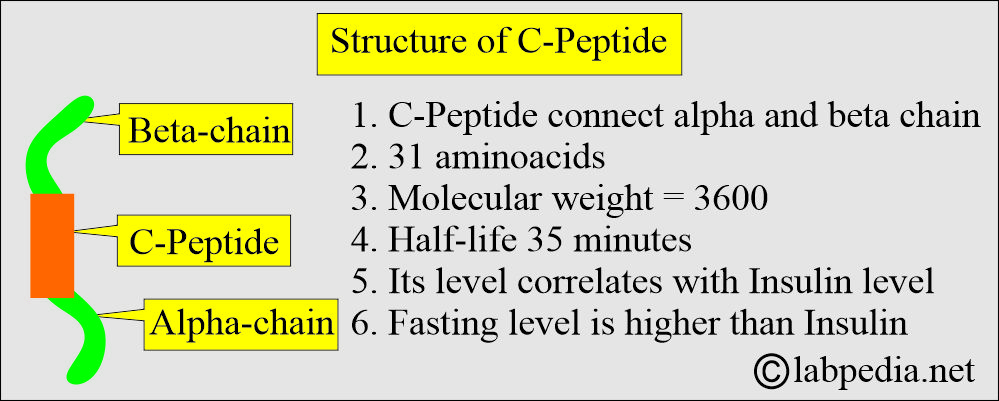
- C-peptide is a connecting peptide for the β and α-chains of proinsulin.
- C-peptide is formed during the conversion of proinsulin to Insulin.
- C-peptide is released into the portal vein in an equal amount.
- It has a longer half-life than insulin. So more C-peptides are present in the circulation.
What do you know about Proinsulin?
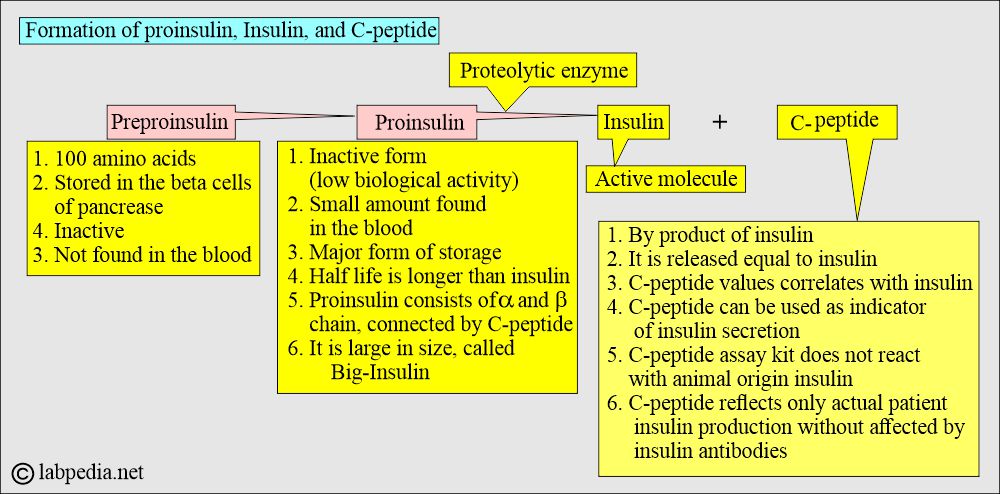
- Proinsulin is cleaved into Insulin + C-peptide (biologically inactive).
- Proinsulin is synthesized in the pancreas and is metabolically inactive.
- It is larger and is also called big insulin.
- It consists of 100 amino acids and has a molecular weight of 12,000 and is formed by the ribosomes in the rough endoplasmic reticulum of the pancreatic β-cells.
- Preproinsulin is not detected in blood circulation and is rapidly converted by cleaving enzymes into proinsulin.
- Proinsulin consists of α and β chains connected by an area called the connecting peptide (C-Peptide).
- Proinsulin is cleaved by a proteolytic enzyme in the β-cells into equal amounts of insulin and C-peptide.
The C-peptide:
How will you define C-Peptide?
- C-Peptide connects the α and β-chains of the proinsulin.
- Its assay provides the difference between endogenous and exogenous insulin.
- C-peptide consists of 31 amino acids connecting peptides with a molecular weight of 3600.
What is the metabolism of C-Peptide?
- Its half-life is 35 minutes, slightly longer than insulin.
- The liver does not extract the C-peptide, which is removed from the circulation by the kidneys and degraded.
- A small fraction of unchanged is excreted in the urine.
- C-peptide levels correlate with insulin levels in the blood, except in cases of islet cell neoplasm and possibly in obese patients.
- C-peptide level and insulin level generally correlate with each other (except for obese patients and patients with insulinoma).
- The fasting C-peptide level is five to 10 times higher than the insulin due to a longer half-life.
- The capacity of beta cells in the pancreas to produce insulin can be measured either by directly measuring insulin or C-peptide.
- C-Peptide level estimation is helpful in the following conditions:
- Differentiate type 1 and type 2 diabetes mellitus. Type 1 diabetes mellitus typically has a low level of C-peptide and insulin, whereas type 2 diabetes mellitus usually has a normal or elevated level of C-peptide.
- In patients taking exogenous insulin, C-peptide is a more accurate measure of islet cell function. This will also help to see the endogenous production of insulin.
- DM patients are treated with insulin and have anti-insulin antibodies. These antibodies falsely increase the level of insulin.
- In people who produce hypoglycemia, by giving them insulin. There will be raised insulin levels, but the C-peptide level will be normal.
- Exogenous insulin suppresses the production of endogenous insulin and C-peptide.
- A rise in the C-peptide level in a treated patient with insulinoma indicates recurrence.
What are the advantages of C-peptide over Insulin?
- C-peptide is a better indicator of β-cell function due to its good concentration level in the blood than peripheral insulin concentration.
- It does not cross-react with the insulin antibody, interfering with insulin immunoassay.
- The C-peptide assay doesn’t measure the exogenous insulin.
- C-peptide is not found in the commercial preparation of insulin.
- C-peptide has a longer half-life than insulin.
- C-peptide is a better indicator of fasting hypoglycemia.
- C-peptide has negligible metabolism in the liver, so its concentration is a better indicator of the β-cell’s function than the peripheral insulin.
- To evaluate insulin reserve or production in diabetics who are on insulin therapy.
- It is used to assess the pancreatectomy status.
- It is used to detect or prove false medication and insulin-induced hypoglycemia.
| Parameter | C-Peptide | Insulin |
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
What will be the C-peptide value in the following conditions?
- The insulin assay cannot differentiate between exogenous insulin and that produced by an insulinoma.
- The C-peptide level is estimated on the same specimen as elevated insulin levels.
- In hyperinsulinemia due to an islet tumor, C-peptide levels are also elevated.
- In the case of exogenously administered insulin, the C-peptide level is low.
| Clinical condition | Glucose level | Insulin level | C-peptide |
|
|
|
|
|
|
|
|
|
|
|
|
What is normal C-peptide?
Source 2
|
|
|
|
|
|
-
- (values vary from lab to lab; it’s best to establish your values)
Source 1 Normal C-Peptide
|
|
|
|
|
|
|
|
|
What are the causes of a raised level of C-peptide?
- Insulinoma.
- Oral hypoglycemic drugs.
- Islet cell tumor-producing insulin (Insulinomas).
- Type 2 DM (non-insulin-dependent).
- Renal failure.
- Hyperthyroidism.
- Cirrhosis.
What are the causes of decreased C-peptide levels?
- Exogenous administration of insulin, e.g., Factitious hypoglycemia.
- Type 1 diabetes mellitus.
- Pancreatectomy.
How will you discuss the insulin/C-peptide ratio?
- This insulin/C-peptide ratio is 1:5 to 1:15.
- 50% of the insulin is removed from the blood during its initial passage through the liver.
- Insulin is metabolized in the liver, with a half-life of 30 minutes, while the half-life of C-peptide is 35 minutes.
- The normal molar fasting ratio of C-peptide: Insulin = 5.
- <1.0 ratio is seen in:
- Insulinoma.
- Sulfonylurea administration.
- Renal failure.
- >1.0 ratio is seen in:
- Exogenous insulin administration.
- Cirrhosis.
- <1.0 ratio is seen in:
Questions and answers:
Question 1: What is the half-life of C-Peptide?
Question 2: What is the level of glucose in insulinoma?