Bone Marrow Aspiration and Trephine Biopsy Part 1
Bone Marrow Aspiration and Trephine Biopsy
Indications:
- A bone marrow examination is done to diagnose Leukemia or myeloma.
- Bone marrow is done to diagnose anemias e.g Megaloblastic anemia, aplastic anemia or sideroblastic anemia.
- To find a deficient iron stored by special stains (Prussian blue).
- To rule out any infiltration of the tumors.
- To rule out the presence of fibrosis.
- Bone marrow did as a staging part of lymphoma.
- In Fever due to unknown cause of pyrexia (PUO).
- This can be indicated for infections.
- In the case of thrombocytopenia.
Procedure for Bone Marrow aspiration and Trephine biopsy:
- This procedure can be done as an outdoor procedure.
- Children and patients in tension need mild sedatives before the procedure.
- If there are hairs, then shave the area.
- Wash with the soap, then clean with the antiseptic.
- Drap the area with a sterile cloth.
- Bone marrow aspiration is done on the patient under local analgesia.
- 1 to 2% Xylocaine is injected locally.
- Go deep to infiltrate the periosteum of the bone.
- A small 3 mm incision may be made to pierce the skin and subcutaneous tissue easily.
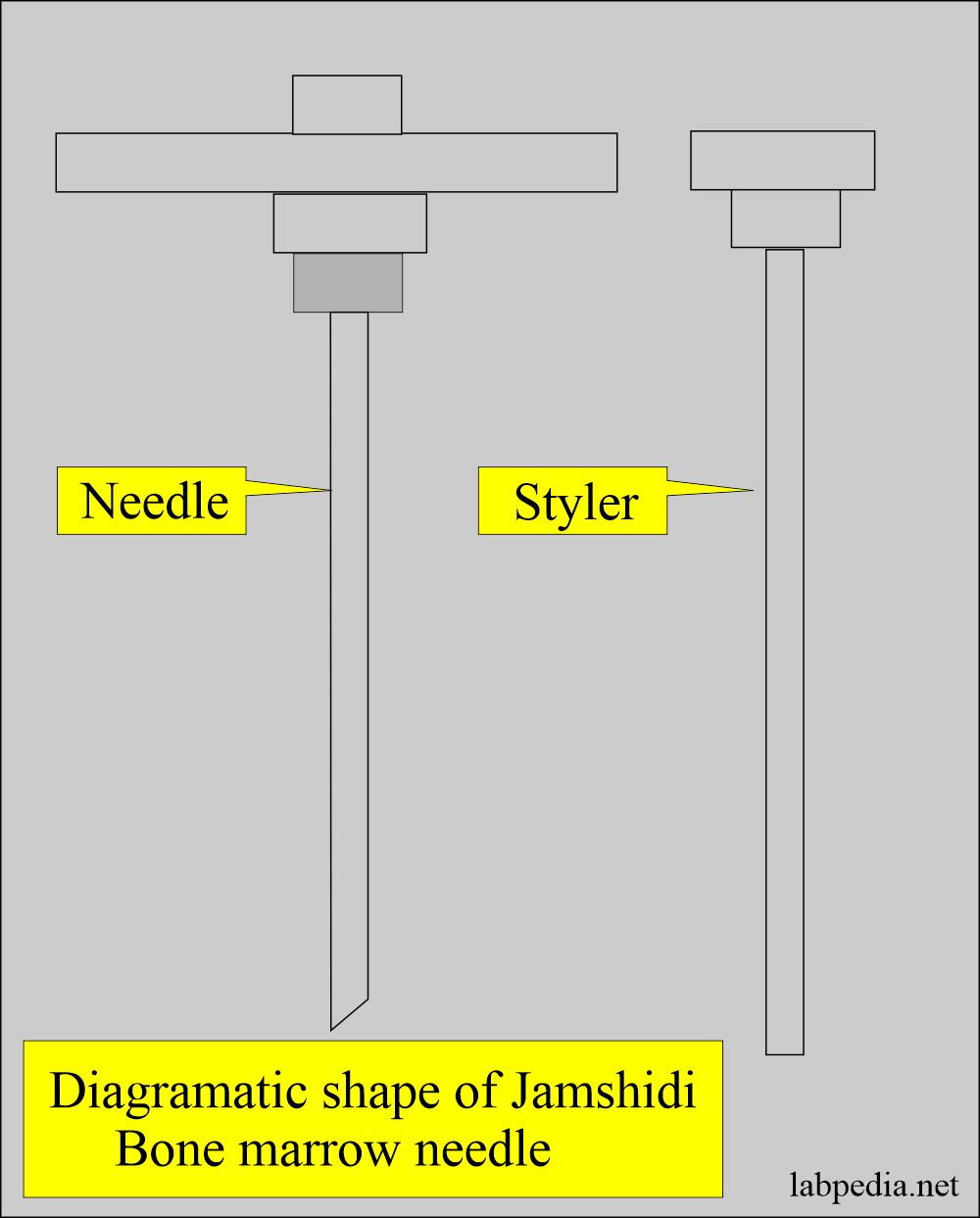
- An adult-size Jamshidi needle is needed.
- It is an 11-gauge x 4-inch length.
- Penetrate the bone and take out the stylet when entering the marrow cavity.
- Attach the syringe (20 to 50 ml size), and suck the marrow; the patient will feel sharp pain, indicating that you are in the marrow cavity.
- Get 1 to 1.5 mL of the marrow particles.
- The marrow tissue is seen as grey particles floating in the blood and fat droplets.
- More samples may be aspirated for flow cytometry, chromosome studies, culture, and other tests.
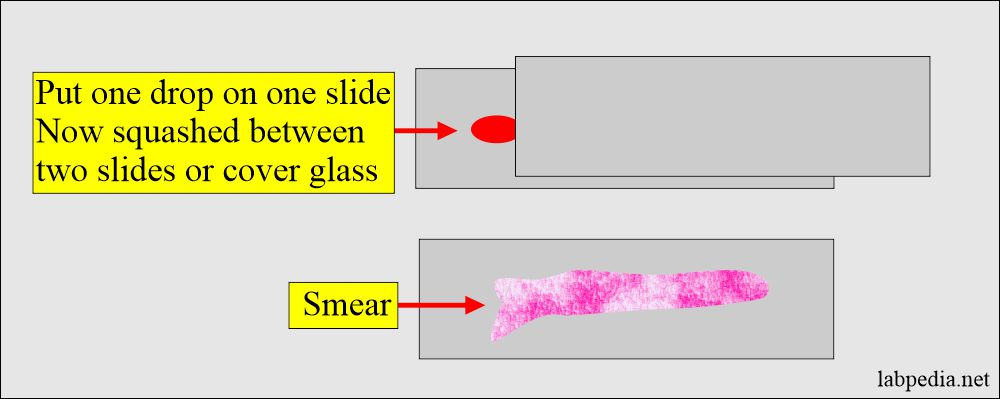
- Immediately make the smears before the blood clots.
- You make a slide by putting one drop on one slide and spreading it on another.
- The clotted sample is put into fixative (10% buffered formalin), which is used for the sections.
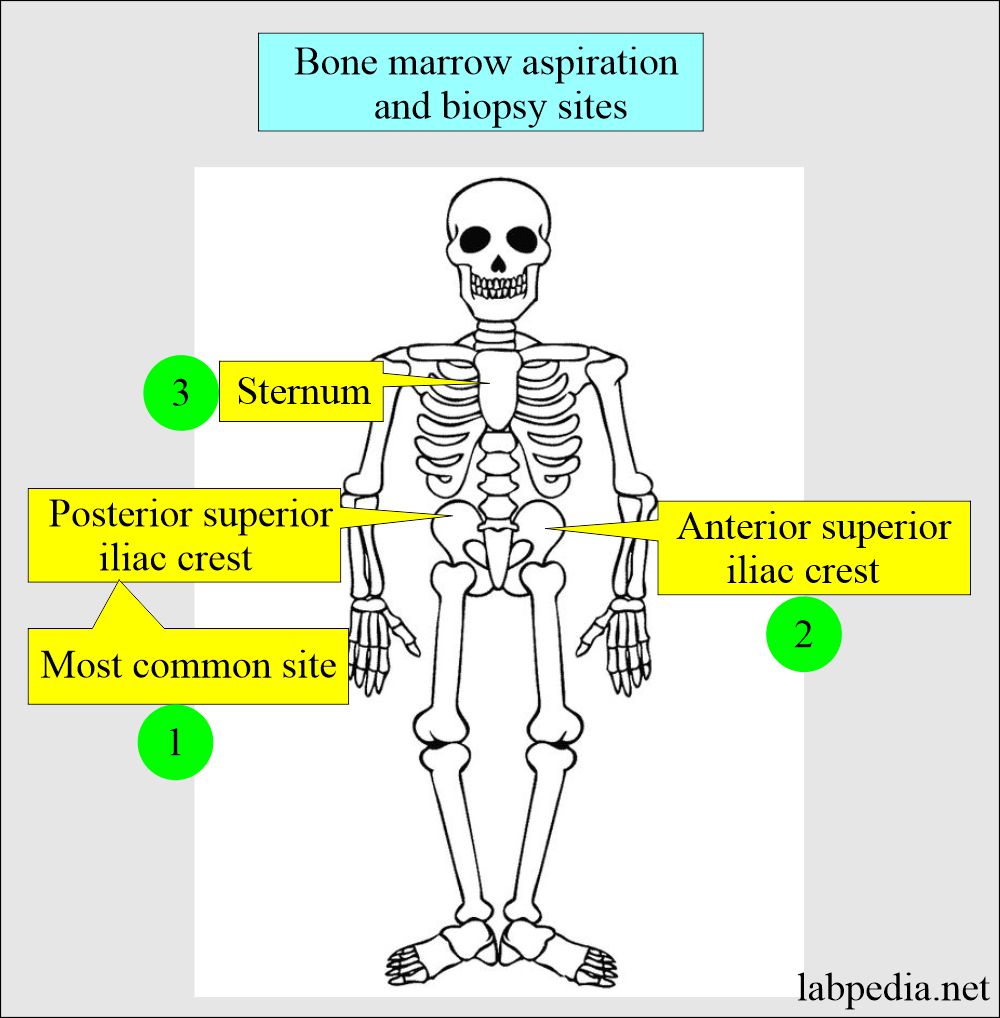
- The most common site is the Posterior Iliac crest (pelvis).
- Other sites are sternum and anterior iliac crest.
- One-half to 2 ml of bone marrow is aspirated.
- Bone marrow aspiration is done first.
- A bone biopsy follows bone marrow aspiration.
- During the aspiration of marrow.
- Liquid bone marrow is aspirated or sucked into the syringe.
- Then spread the sample on the slides.
- The patient may feel a sharp pain on suction, indicating marrow aspiration.
- Before the bone marrow aspiration, makes the peripheral blood smear and perform the Differential count.
- For infants, general anesthesia may be needed.
Complications of Bone Marrow Aspiration and Trephine Biopsy:
- The needle may break.
- There may be a hemorrhage.
- There may be infections.
- Rarely may there be chronic pain at the bone marrow aspirate or biopsy site.
- There are chances of bleeding if the patient has an increased tendency for bleeding.
- There are chances for infection in the case of leukopenia.
- The sternum is not a safe site, and chances for complications are increased.
- There may be a sternal fracture in case of a sternal puncture.
- Sometimes patient complains of pain and tenderness at the site of the puncture.
Contraindications of bone marrow aspiration and biopsy:
- In patients who are not cooperative.
- The patients with a bleeding tendency or coagulation disorders.
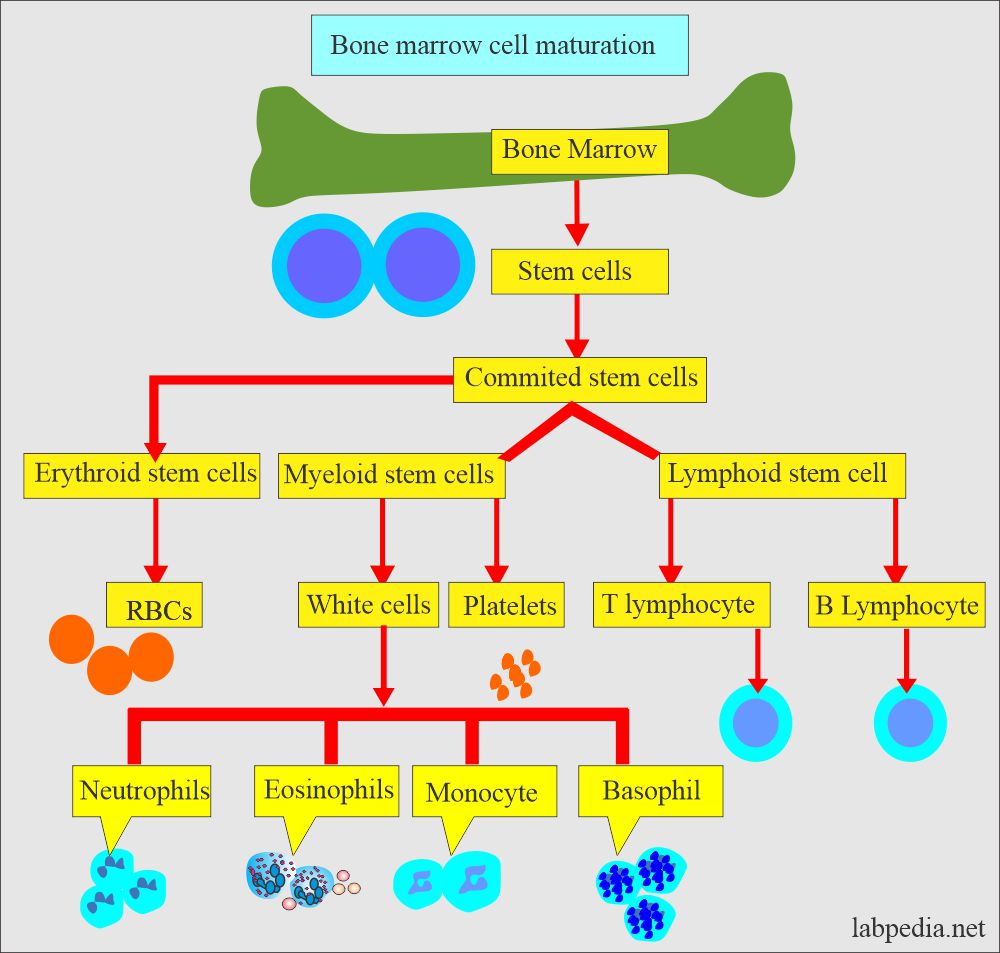
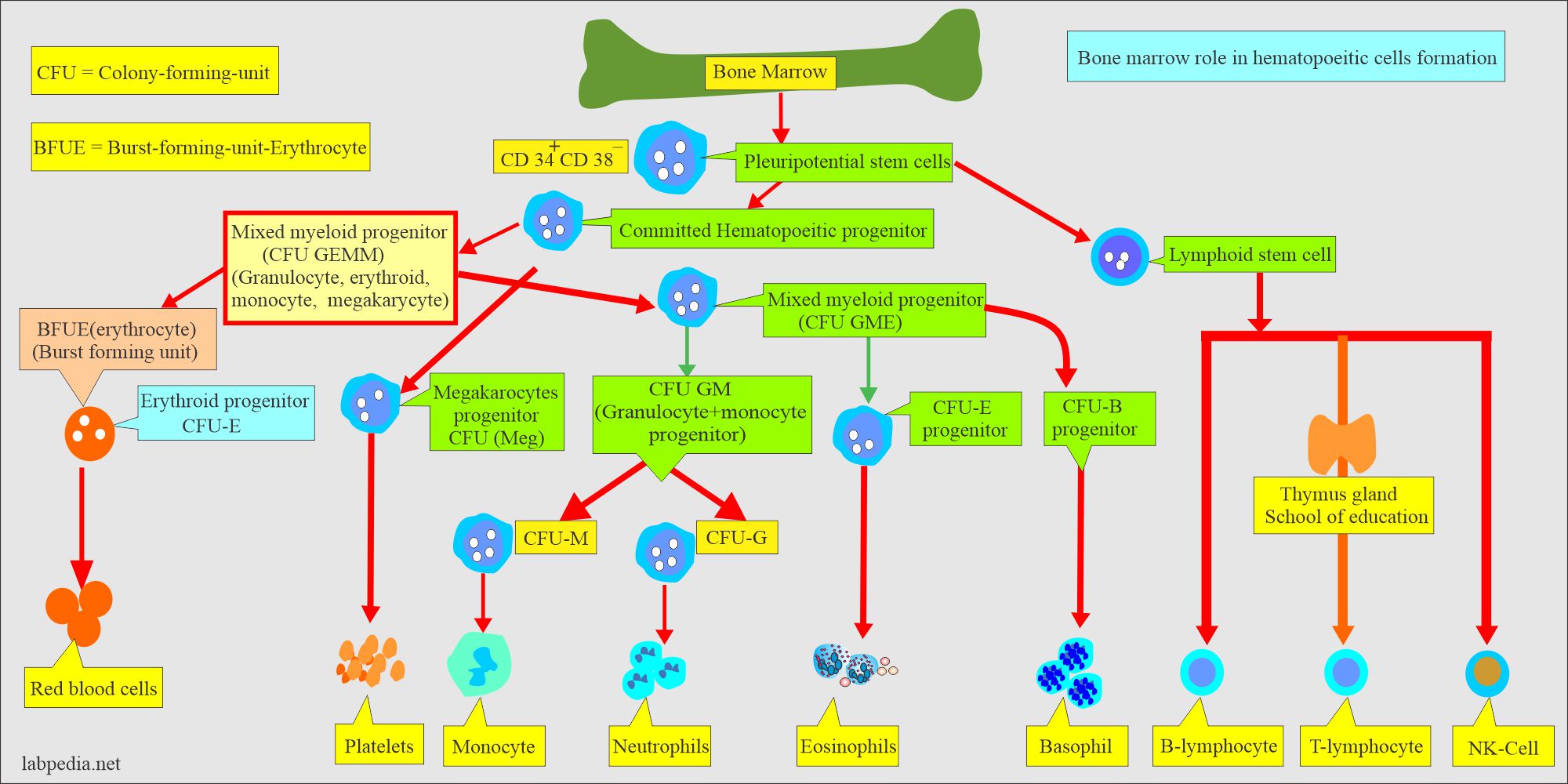
Pathophysiology of Bone Marrow:
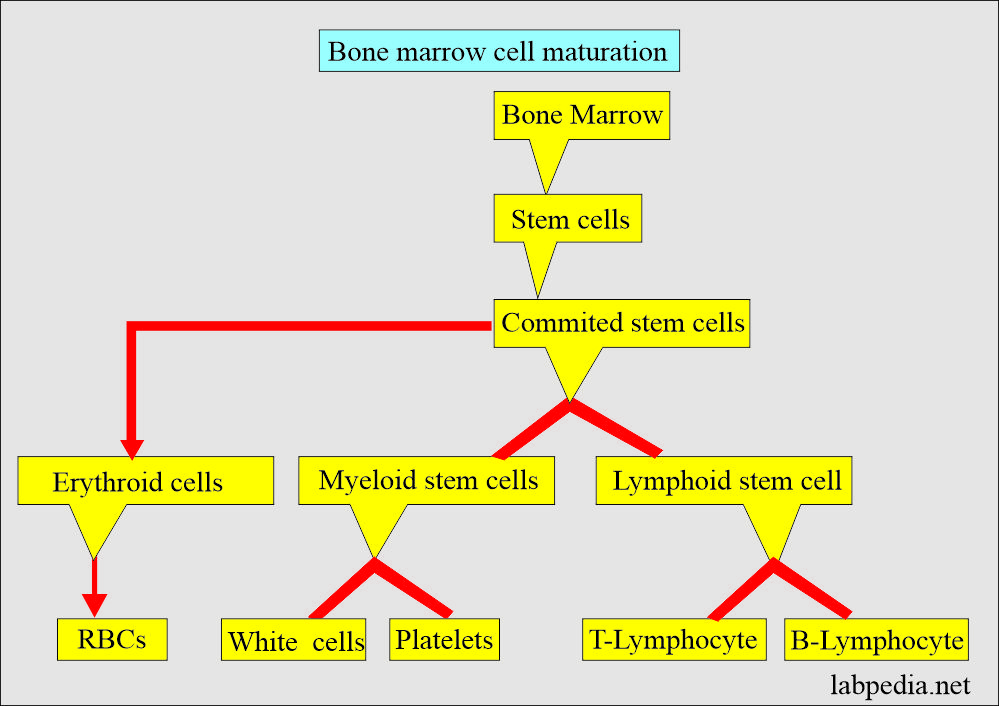
- Bone marrow is found in the central fatty portion of the ribs, sternum, pelvis, and long bones like the femur, tibia, and humerus.
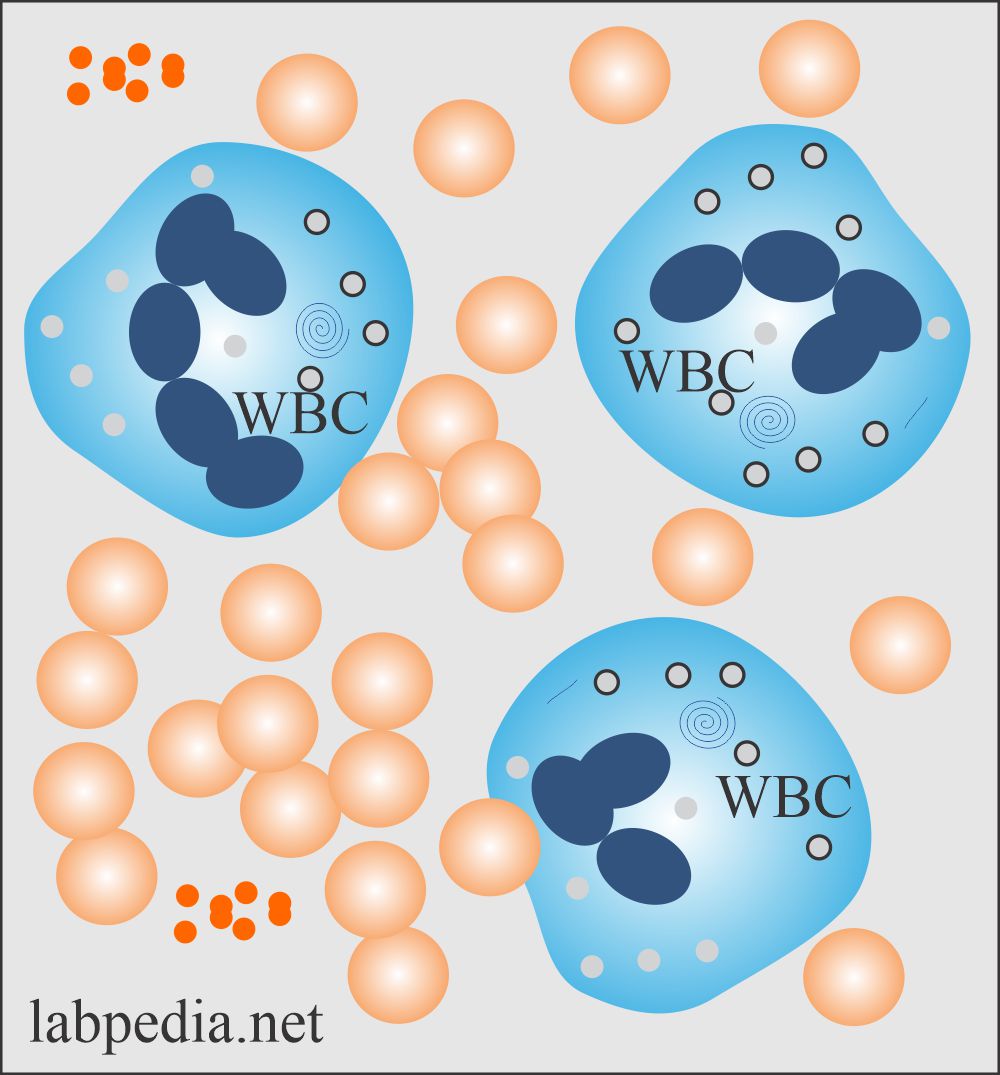
- Bone marrow consists of differentiated and undifferentiated hematopoietic cells, Reticuloendothelial cells, and fatty tissue.
- These stem cells differentiate into the different types of cells in the blood.
- These cells, after maturation, gain entrance to the peripheral blood.
Stages of Red cell maturation.
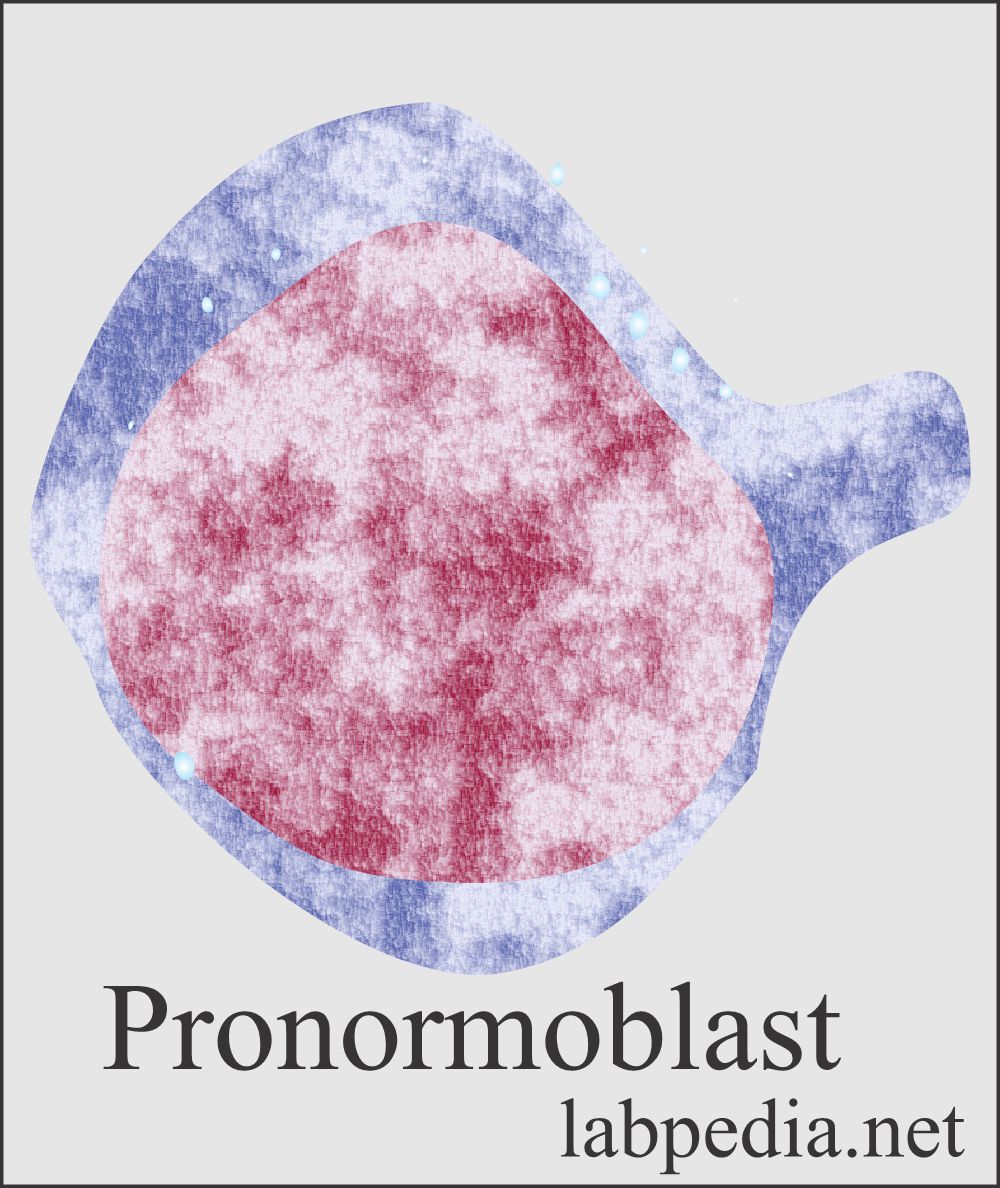
Pronormoblast:
- It is the most immature and largest in erythropoiesis.
- The nucleus is round and stains dark violet.
- Densley packed chromatin and indistinct nucleoli blue in color.
- There are cytoplasmic extrusions.
Basophilic normoblast:
- The cell size is decreased.
- The nucleus is round and contains chromatin with strong contrast.
- The cytoplasm is slightly basophilic.
Polychromatic normoblast:
- The shape of the cells and the structure of the nucleus is similar to basophilic normoblasts.
- The cell size further decreased.
- The cytoplasm is blue-grey-violet due to the presence of hemoglobin.
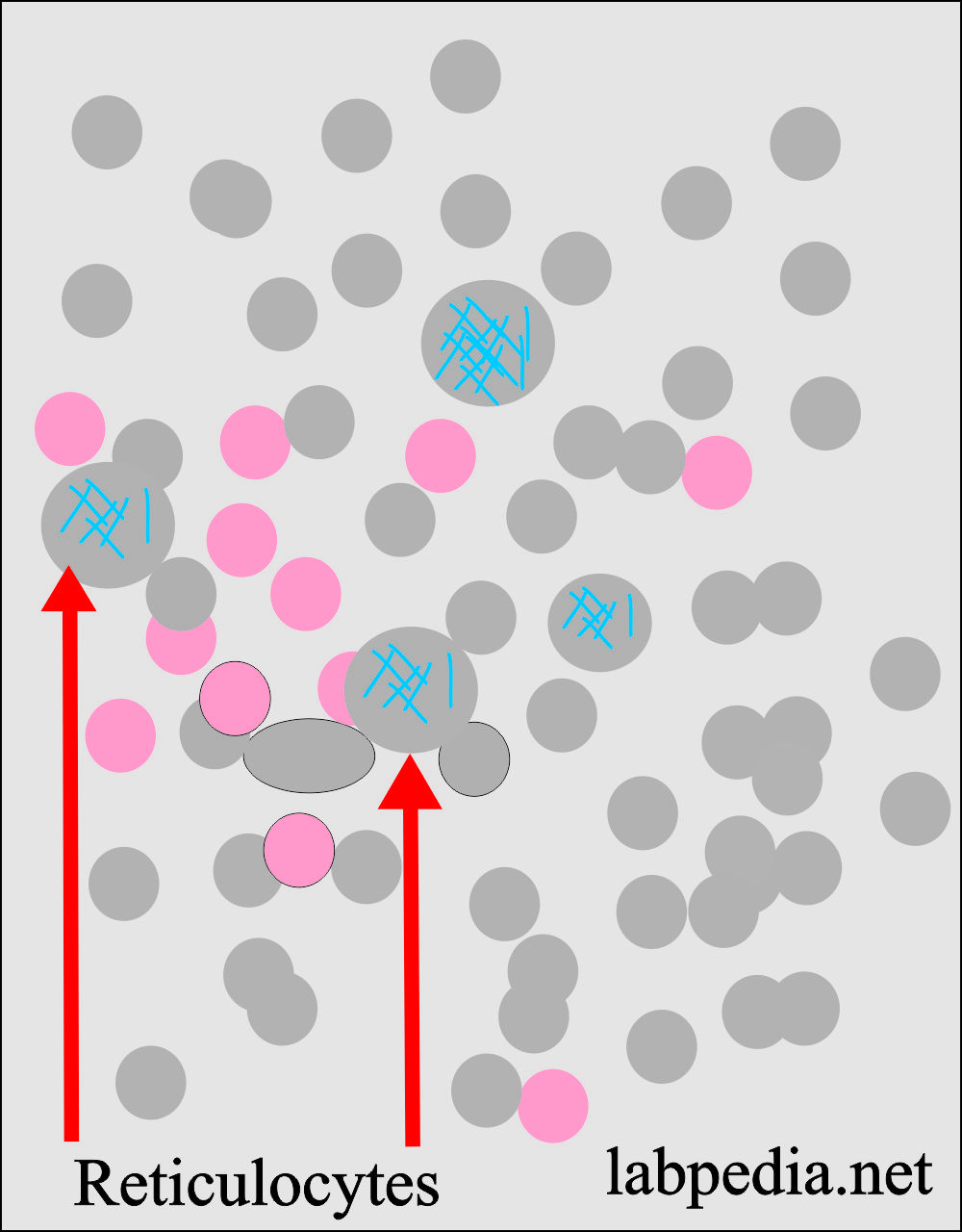
Reticulocytes:
- It is characterized by the presence of granular or reticular filamentous structures.
- These are present in 0.5% to 1.5% of the mature RBCs.
- These are only seen after staining with methylene blue.
- RBCs are pale greenish-blue, and the filamentous structures are blue-black.
Erythrocytes (Normal red blood cells):
- It is a circular, biconcave, and reddish RBC.
- Size is mostly the same, measuring 7 to 8 µm in diameter.
- There is no visible inner structure.
Stages of Neutrophils maturation.
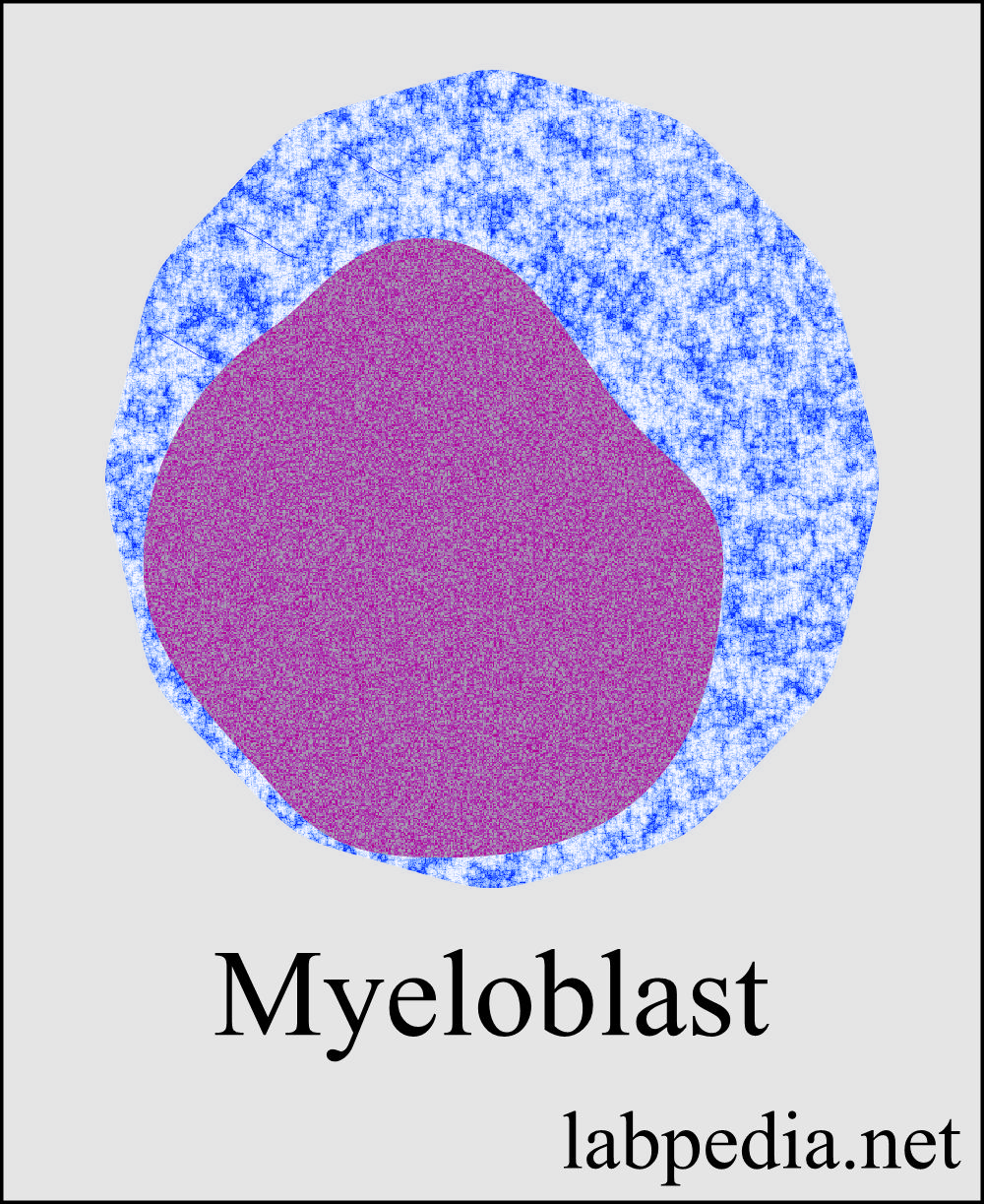
Myeloblast:
- This is the least mature white cell.
- Its number is scanty in the bone marrow.
- The size is slightly smaller than the proerythroblast.
- Myeloblast exists in various forms.
- The nucleus is oval and may have a slight indentation on one side.
- Chromatin is in fine, closely meshed, transparent filaments.
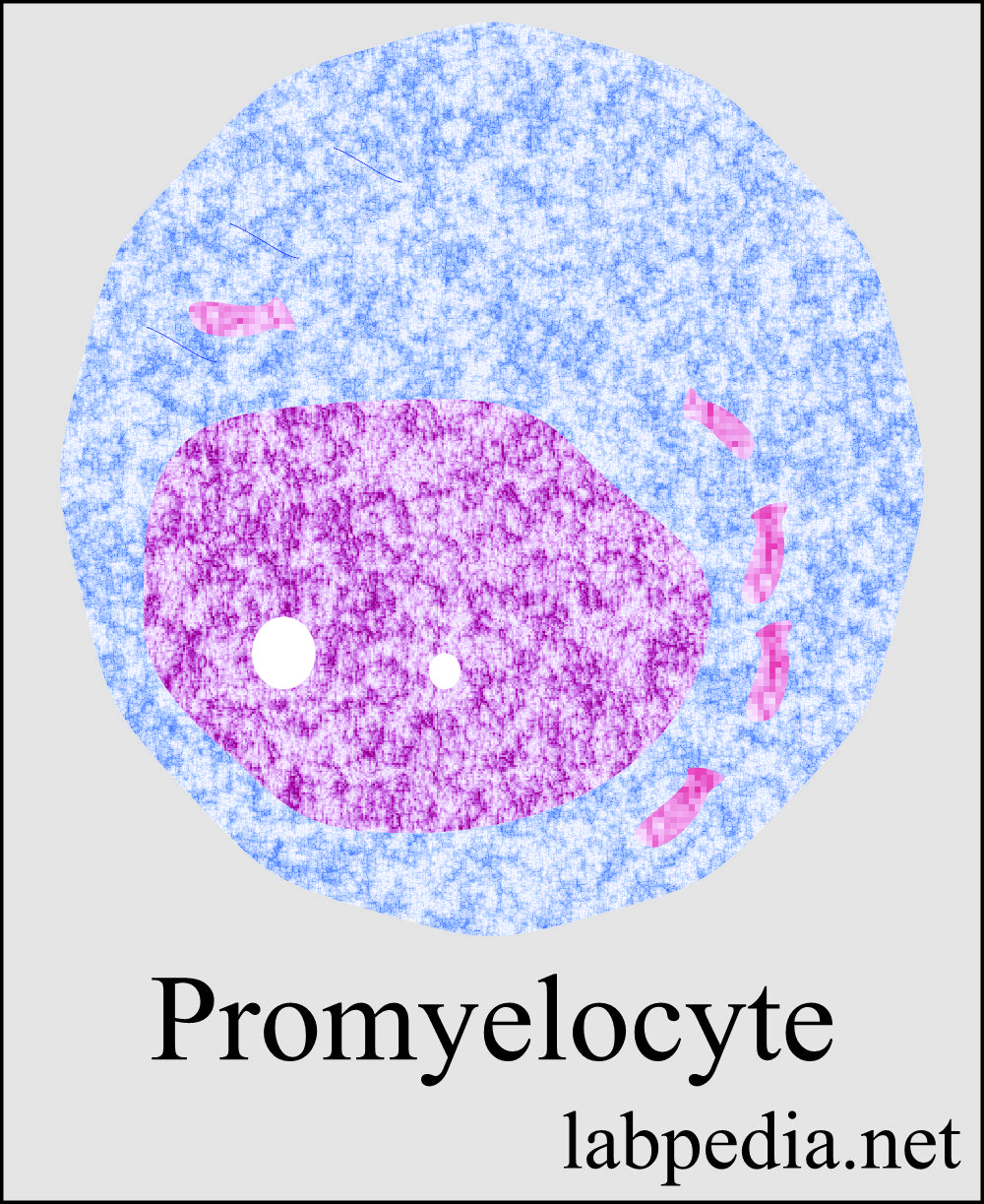
Promyelocytes:
- These have a variable nuclear-cytoplasm ratio.
- The granulation is variable.
- Characteristic as an oval-shaped nucleus. These are often flattened or indented on one side (kidney-shaped).
- Chromatin density is moderate.
- The cytoplasm is light-blue, with a lighter area near the nucleus.
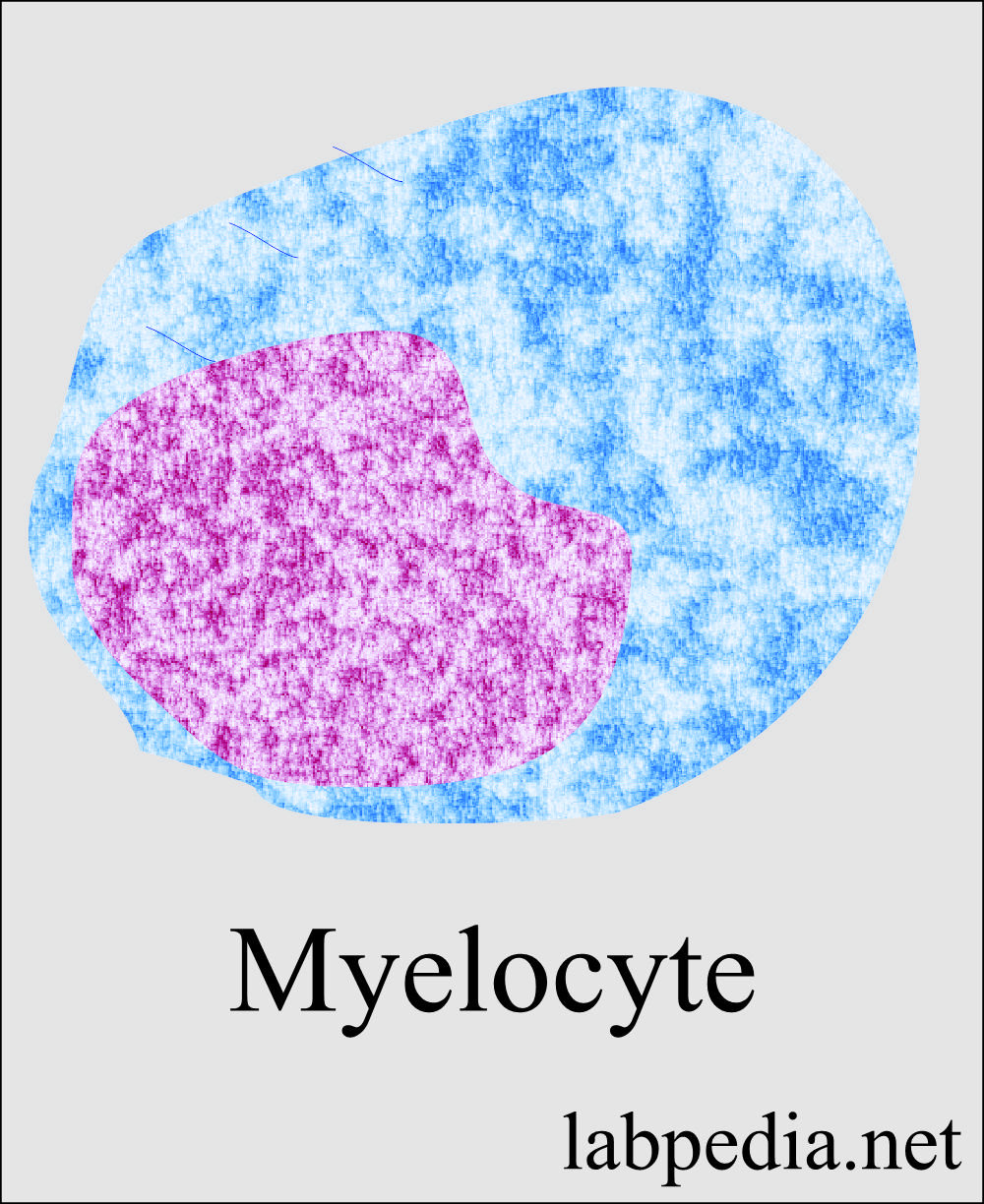
Myelocytes:
- There is a decrease in cell size and the nucleus.
- Chromatin is more coarse, and nucleoli are barely visible.
- The cytoplasmic is no longer basophilic; it takes on a pale grey-brown or pink-brown color.
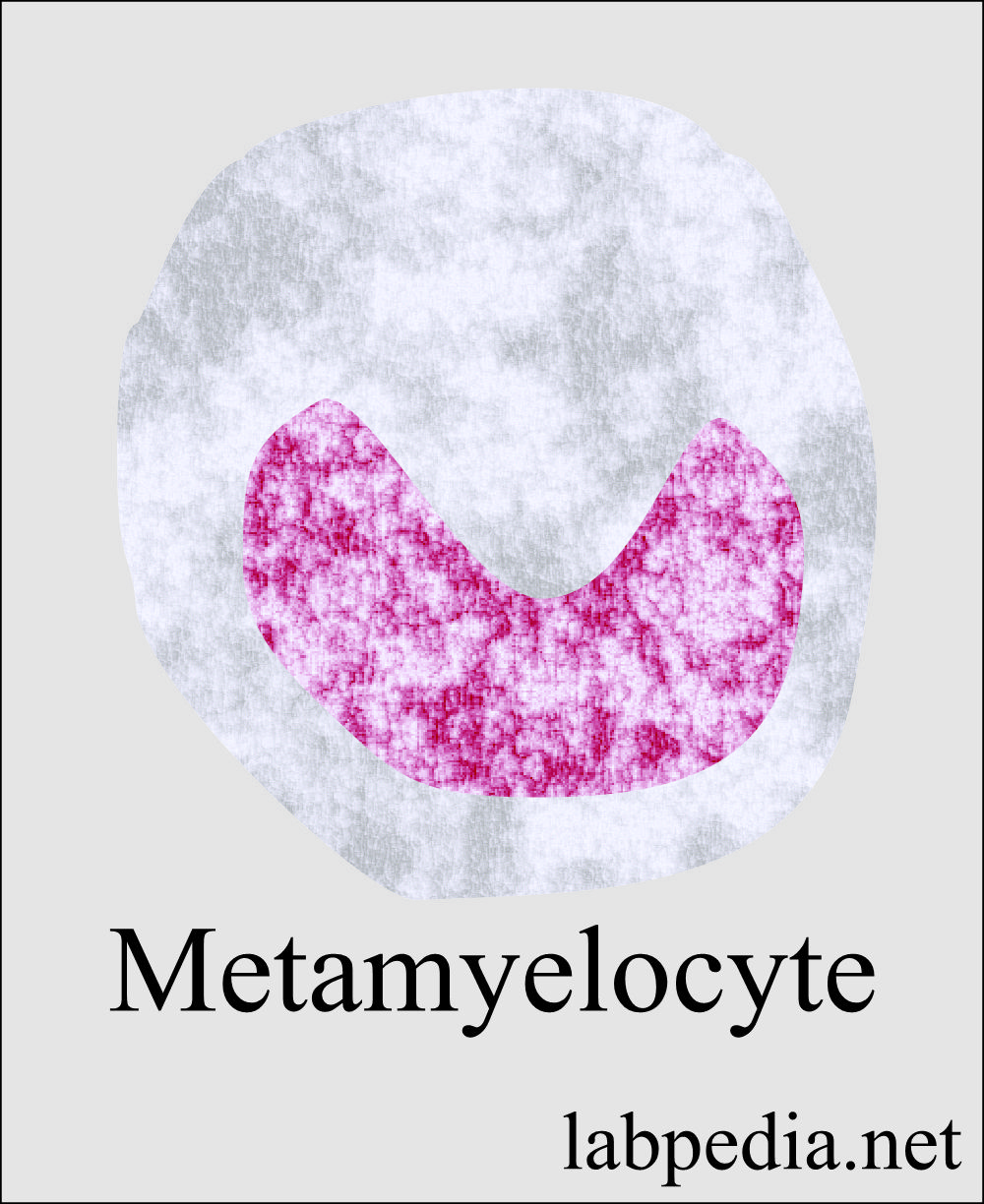
Metamyelocytes:
- The nucleus is bean or kidney-shaped.
- Chromatin is coarse and compact in areas.
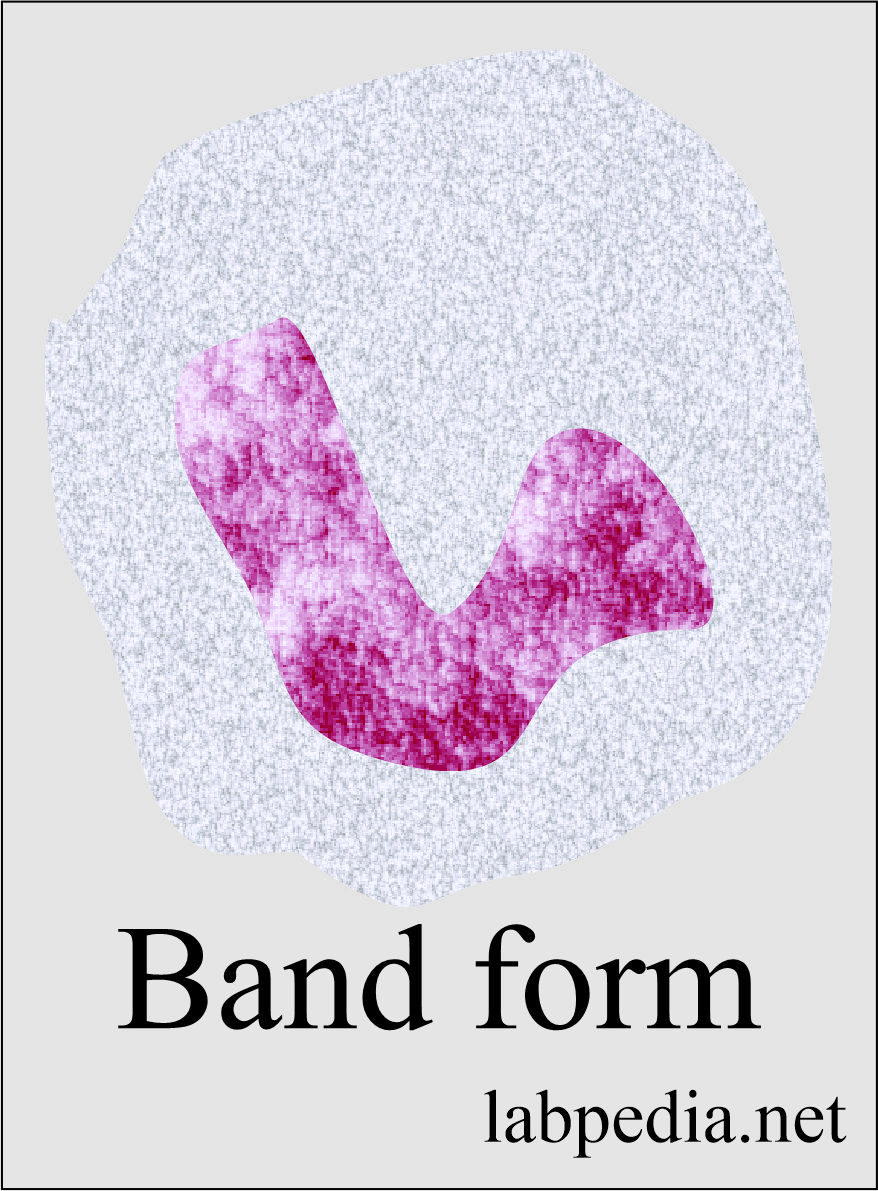
Band neutrophils:
- The nucleus is C or S shape.
- Chromatin is coarser.
Mature neutrophils or Polys:
- These are mature neutrophilic granulocytes.
- The nucleus is made of 3 to 5 lobes connected by the filament.
Bone marrow evaluation needed for:
- Maturation of red blood series.
- Maturation of white blood series.
- Presence of megakaryocytes.
- Myeloid/erythroid ratio.
- Iron stores.
- Presence or absence of granulomas.
- Any tumor cell infiltrate.
- Overall bone marrow activity.
B.M examination reveals the following information:
- Bone marrow examination shows:
- RBCs shape, number, and size.
- White blood cells’ shapes, size, and number.
- Megakaryocytes and platelets formation.
- Evaluate cellularity, fibrosis, and infiltrate.
- Estimation of iron contents.
- The presence or absence and ratio of cells are characteristic of the suspected disease.
- Multiple myeloma, Plasma cell myeloma, and macroglobulinemia.
- Chronic or acute Leukemia.
- Anemia,e.g., Megaloblastic, macrocytic, and normocytic anemia.
- Toxic states produce bone marrow depression or destruction.
- Neoplastic conditions where the bone marrow is involved with metastatic carcinoma and lymphoproliferative diseases.
- Platelets dysfunctions.
- Some types of infections like Tuberculosis and Histoplasmosis.
- Lipid or glycogen storage disease.
- Deficiency of Iron stores like microcytic anemia.
- Prussian blue stain on bone marrow slides shows iron contents.
Normal Bone Marrow Components:
| Type of cells | Percentage (%) of cells in Bone Marrow | Percentage (%) of cells in peripheral blood |
| Myeloid cells |
||
| Myeloblast | 3 to 5 % (mean 2.0%) | 0 |
| Promyelocytes | 1 to 8 % (mean 5.0%) | 0 |
| Myelocytes neutrophils | 5 to 19 % (mean 12%) | 0 |
| Myelocytes eosinophils | 0.5 to 3 % (mean1.5%) | 0 |
| Myelocytes basophils | 0 to 0.5 %(mean 0.3%) | 0 |
| Metamyelocytes | 17 to 33 % (mean 0.4%) | 0 |
| Neutrophils | 11 to 33 % (mean 20%) | 40% to 70% |
| Monocytes | 0 to 3 % (mean2.0%) | 2% to 10% |
| Lymphocytes | 8 to 20 % (mean 10%) | 20% to 40% |
| Megakaryocytes | 0 to 3 % (mean 0.4%) | 0 |
| Plasma cells | 0 to 2.0 % (mean 0.9%) | 0 |
| Erythroid series cells | ||
| Pronormoblast | 0.2 to 4.0 % (mean 0.5%) | |
| Polychromatic normoblast | 3.5% to 20.5% (mean 10.4%) | |
| Myeloid/Erythroid ratio (WBC: Nucleated RBC) | 2: 1 to 4: 1 | Slightly higher in infants |
- M: E ratio in infection may be 6:1, and in Leukemia, 25:1.
- Hypercellular or hyperplasia of marrow refers to an increase in one or more cell components. This may be due to compensation or a leukemic process.
- Hypocellular or hypoplasia of marrow is due to loss of cellularity or incomplete development in one or more lines of the cells.
Abnormal bone marrow findings are seen in the following:
- Infections:
- Viral.
- Bacterial.
- Fungal.
- Chronic inflammatory diseases.
- Myelofibrosis.
- Agranulocytosis.
- Malignancy:
- Multiple myelomas.
- Hodgkin’s lymphoma.
- Lymphoma.
- Polycythemia vera.
- Leukemias.
- Anemias.
- AIDS.
- Rheumatic Fever.
Difference between bone marrow aspiration and trephine biopsy:
| Feature | Bone marrow aspiration | Bone marrow trephine biopsy |
| Site | Posterior iliac crest, sternum. | Posterior iliac crest. |
|
|
|
|
|
|
|
|
|
|
|
|
Questions and answers:
Question 1: What is the characteristic feature of reticulocytes?
Question 2: Can we see myeloblast in the peripheral blood smear?