Blood sample Types, Anticoagulants, Preservatives, Adverse effects of Additives
Blood Sample Types
What are the indications for whole blood, plasma, and serum?
- A whole blood sample is used for blood gases and ammonia.
- It may be used for estimating glucose, urea nitrogen, and lactate.
- Serum and plasma are used for the majority of the chemical tests.
What are the disadvantages of plasma?
- There is a chance of forming fibrin clots if you store the sample.
- These microclots may block the analyzer’s probe.
- Plasma is not a good sample for electrophoresis.
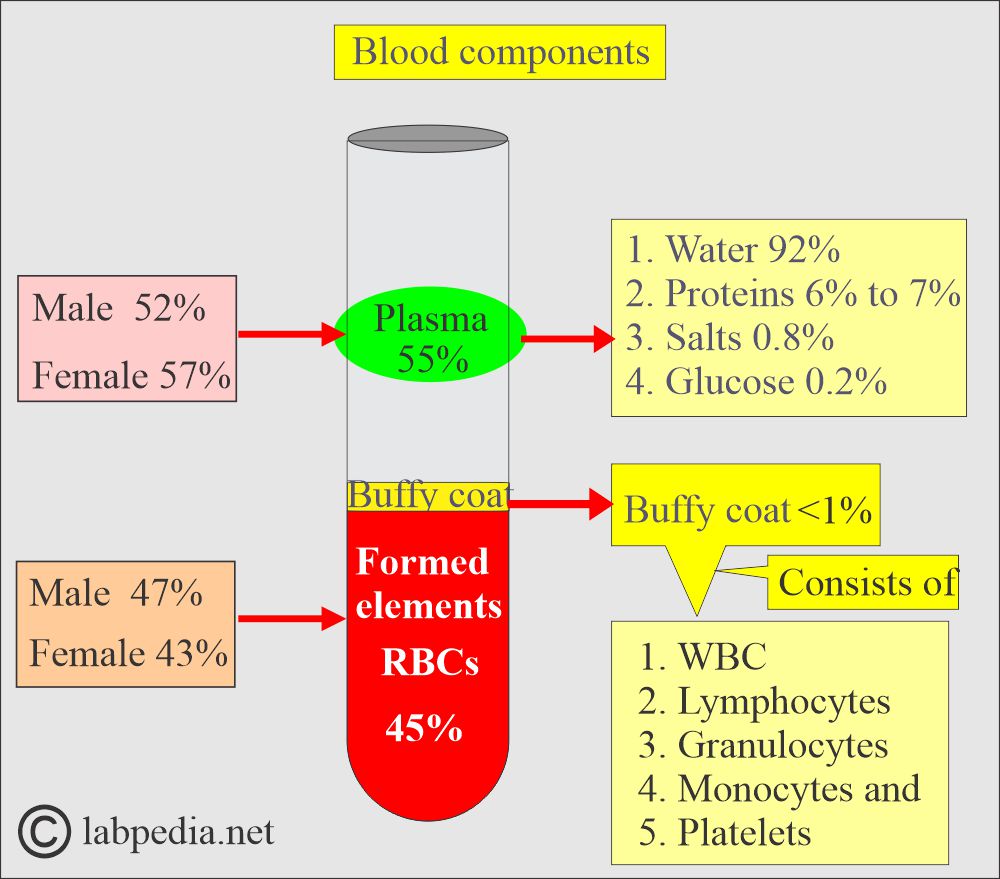
How will you define blood?
- Blood consists of formed elements (RBCs, WBCs, Platelets) in a liquid portion called plasma.
- There is a difference between plasma and serum in estimating various substances in the blood.
What are the types of patients for the blood samples?
Pediatric patients:
- If this is the first time sampling from the child, then try to gain his confidence.
- Blood for neonatal screening is collected to rule out hypothyroidism, phenylketonuria, galactosemia, and hemoglobinopathies.
- For phenylketonuria: The baby must have received 3 to 4 days of full milk, and the infant must have taken the feed.
Adult patients:
- Be friendly and explain the procedure.
Patients in the ICU:
- Patients are unconscious, but there may still be a need to take blood samples.
What are the types of blood samples?
- Various types of blood are:
- Arterial blood.
- This is the best sample for studying blood gases (O2).
- Venous blood.
- It differs from arterial blood in that it has lower concentrations of substances than arterial blood.
- It has a higher concentration of body waste products, such as CO2, organic acids, and ammonia.
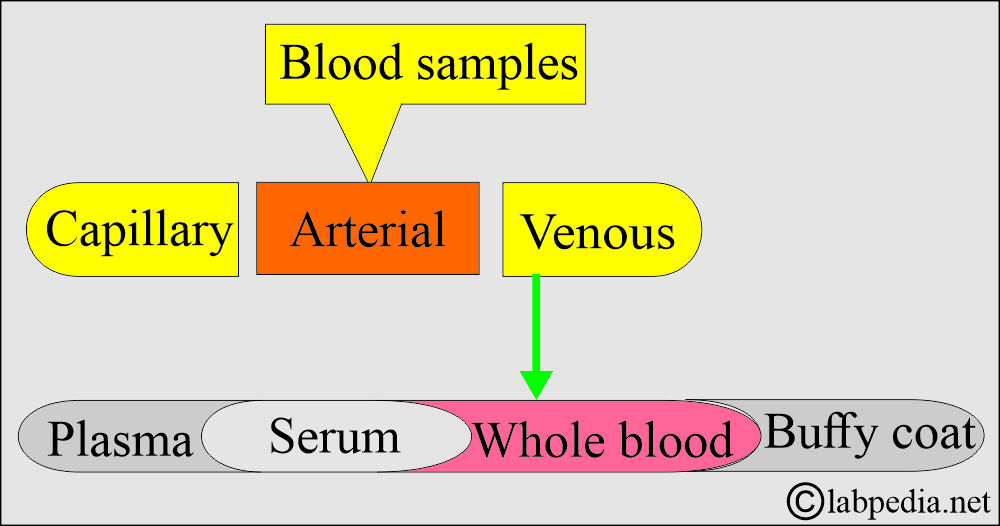
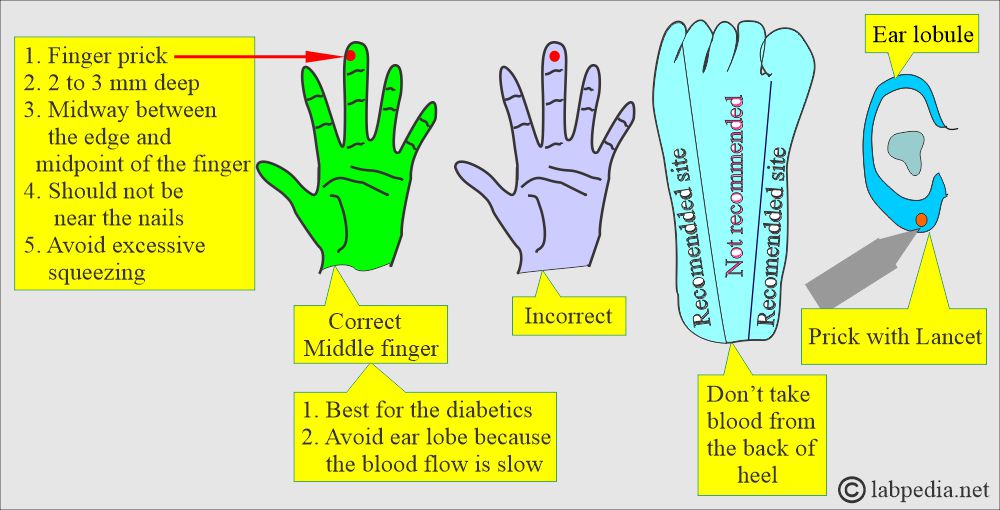
Blood sample types
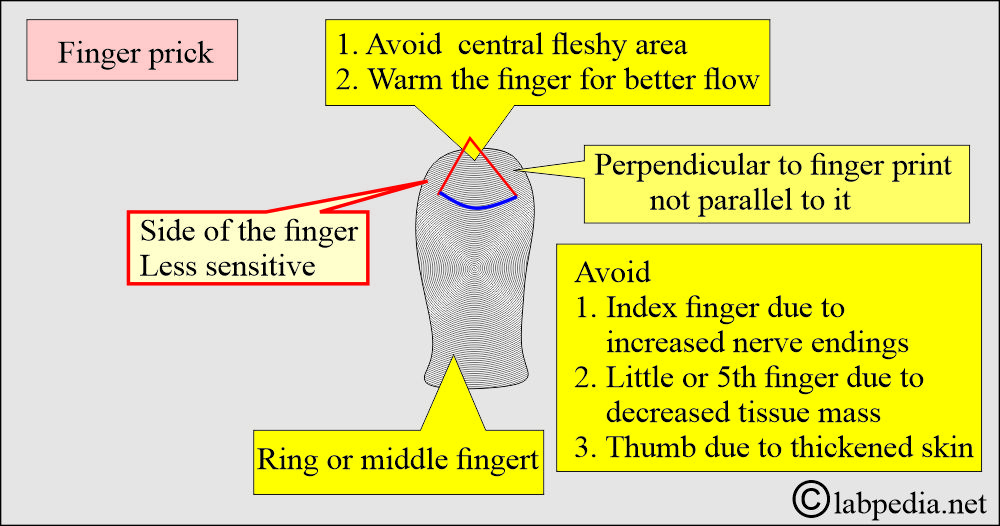
- Capillary blood (skin puncture).
- This is good for a small quantity of blood.
- This is closer to arterial blood than venous blood.
- The patient in shock has 50% less blood glucose than venous blood.
- Warm the finger from which you are taking the blood sample.
- The heel is the best site for obtaining a small blood sample from a newborn under 3 months old.
- The depth should not be >2.4 mm on the heel.
- Avoid the central portion and back of the heel.
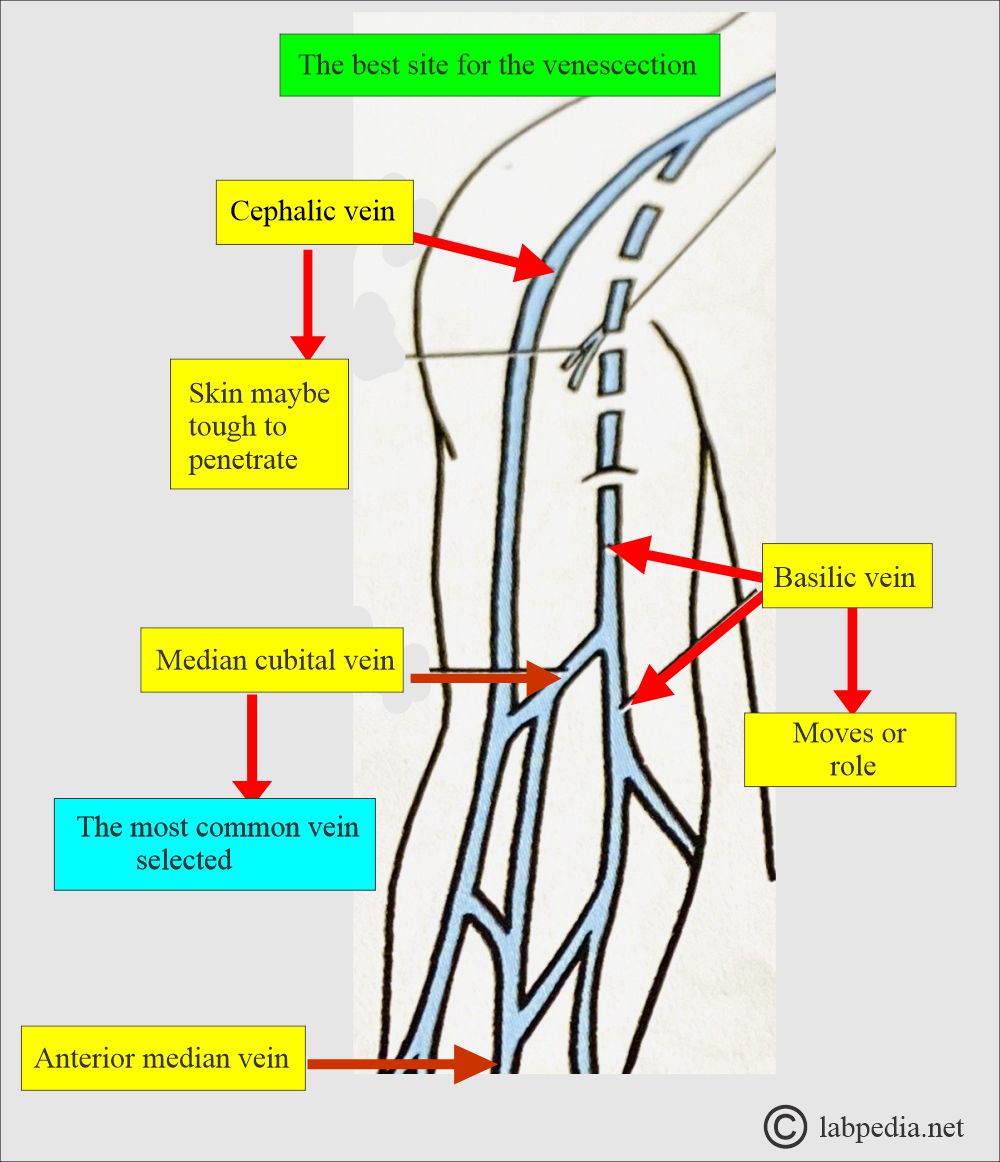
How will you take a Venous blood (venipuncture) sample?
- For larger quantities, we will take venous blood.
- The blood sample is taken from a vein in the forearm, wrist, or ankle.
- A forearm site is preferred. Blood is taken directly from a vein, a procedure called phlebotomy.
- The median cubital vein is usually preferred.
- Mostly venous blood is drawn in the fasting state.
- Blood collected after the meal is called a postprandial sample.
What are the biological variations in blood collection?
- There are biological variables in blood collection:
- The patient is lying in bed or standing up.
- After the exercise.
- Diurnal variations.
- Recent food intake.
- Recent intake of Tea/coffee (caffeine), smoking (nicotine), alcohol ingestion, and drug administration.
- Can take a blood sample in vacutainers, syringes, and with the help of butterfly needles.
- The blood samples can also be taken for blood culture.
What is the difference between the values of venous and capillary blood?
| Capillary blood values < than venous blood | No difference in capillary and venous blood values | Capillary blood values > than venous blood. |
|
|
|
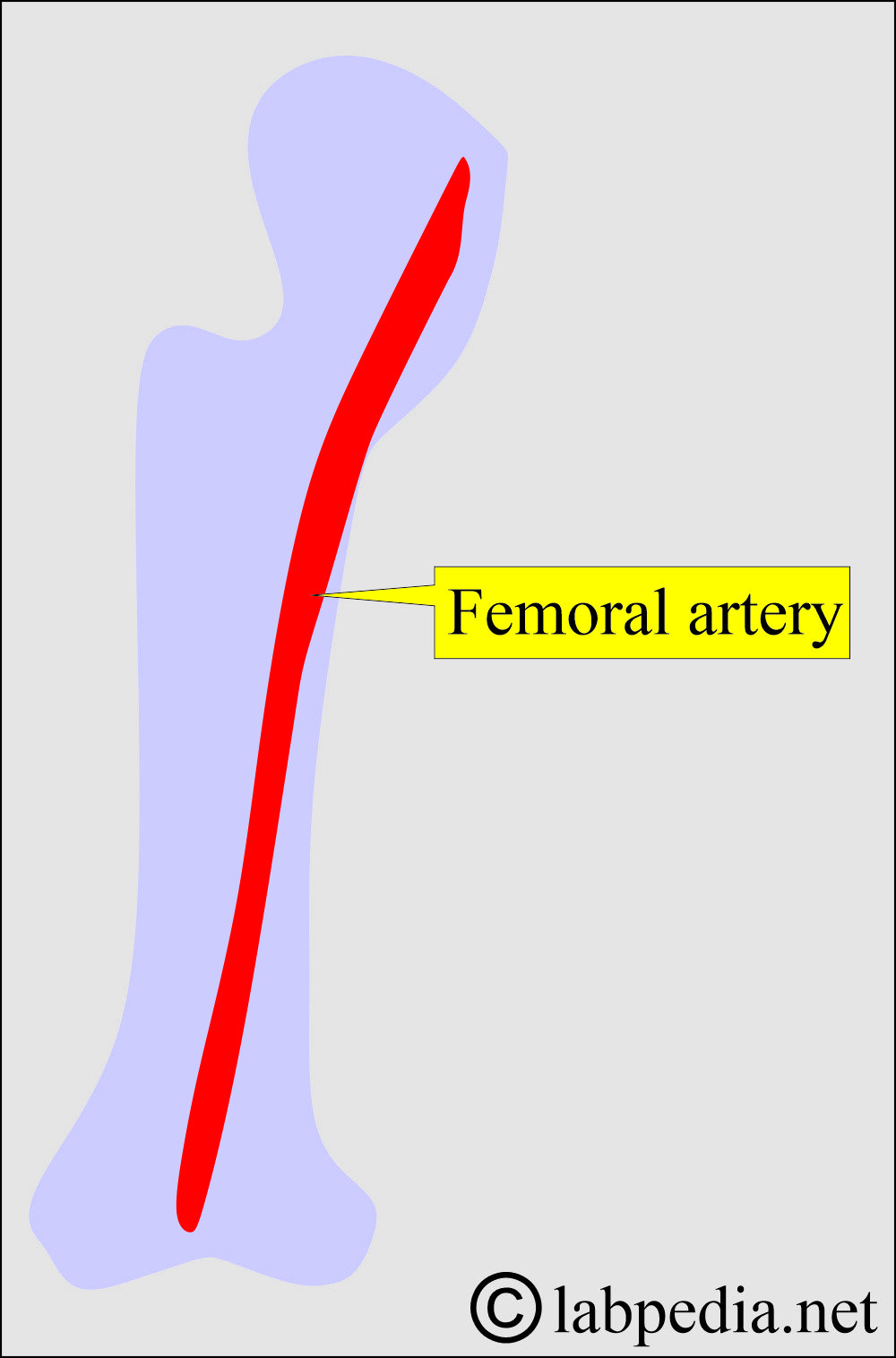
Why is arterial blood needed?
- Arterial blood is needed for the estimation of body gases.
- Arterial blood is usually taken from the femoral artery.
- Blood for gases should be processed immediately without any delay.
What are the types of blood samples and their indications?
| Type of blood sample | Special features | Indications |
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
How will you summarize the blood samples?
Whole blood
How will you define blood?
- Obtain a blood sample in a test tube containing an anticoagulant.
- This sample will contain cells (white blood cells, platelets, RBCs, proteins) and plasma.
- This blood sample can be taken from the capillaries or the veins.
What is the difference between the capillary and venous blood values?
| Characteristic features | Capillary blood vs. Venous blood |
|
|
|
|
|
|
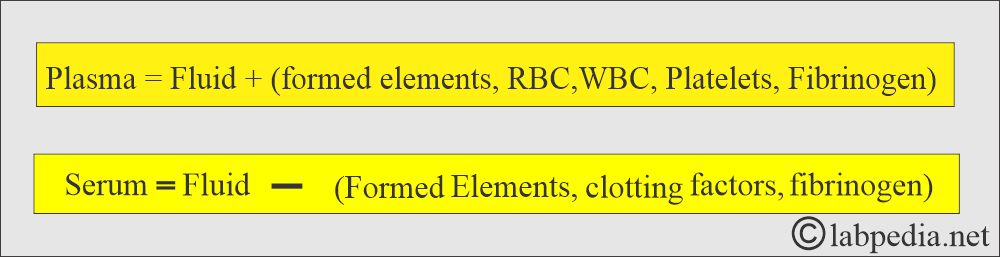
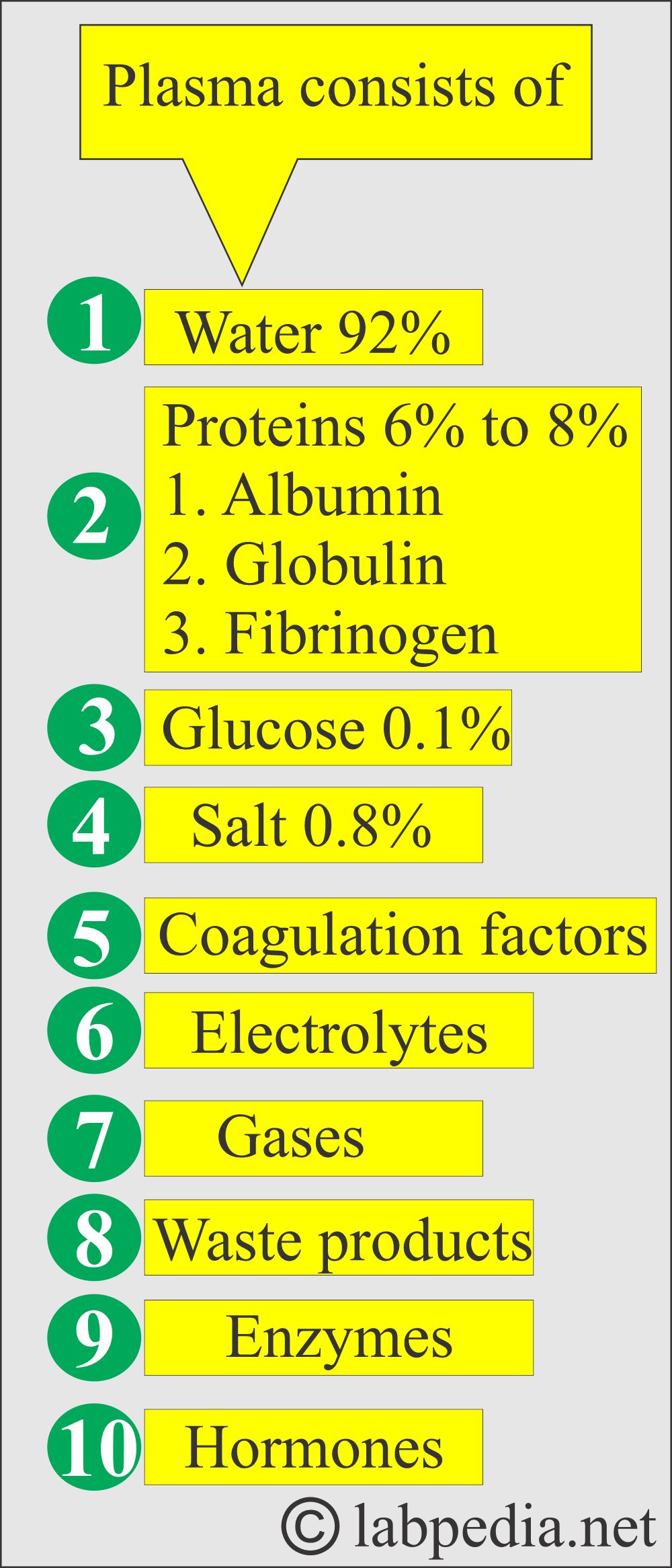
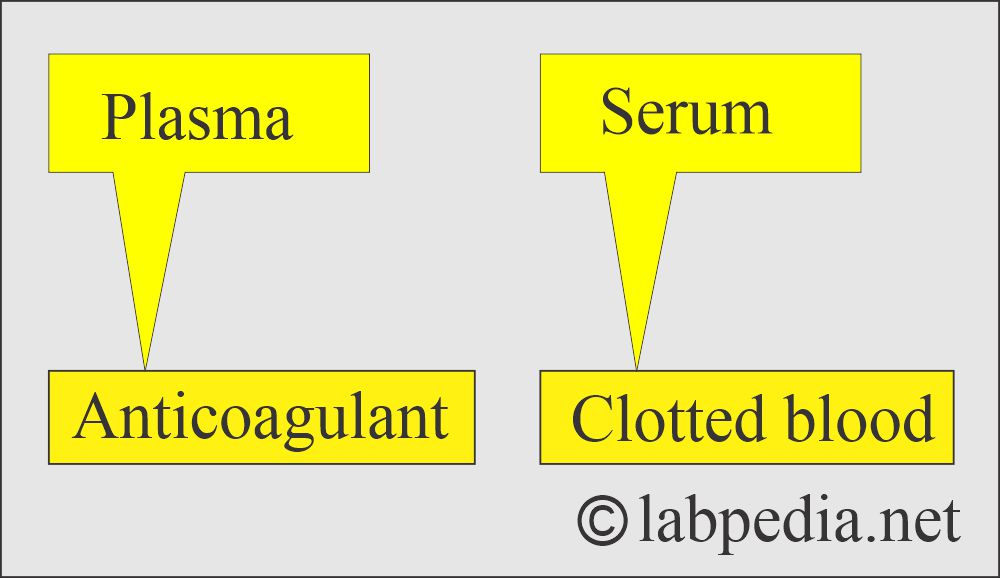
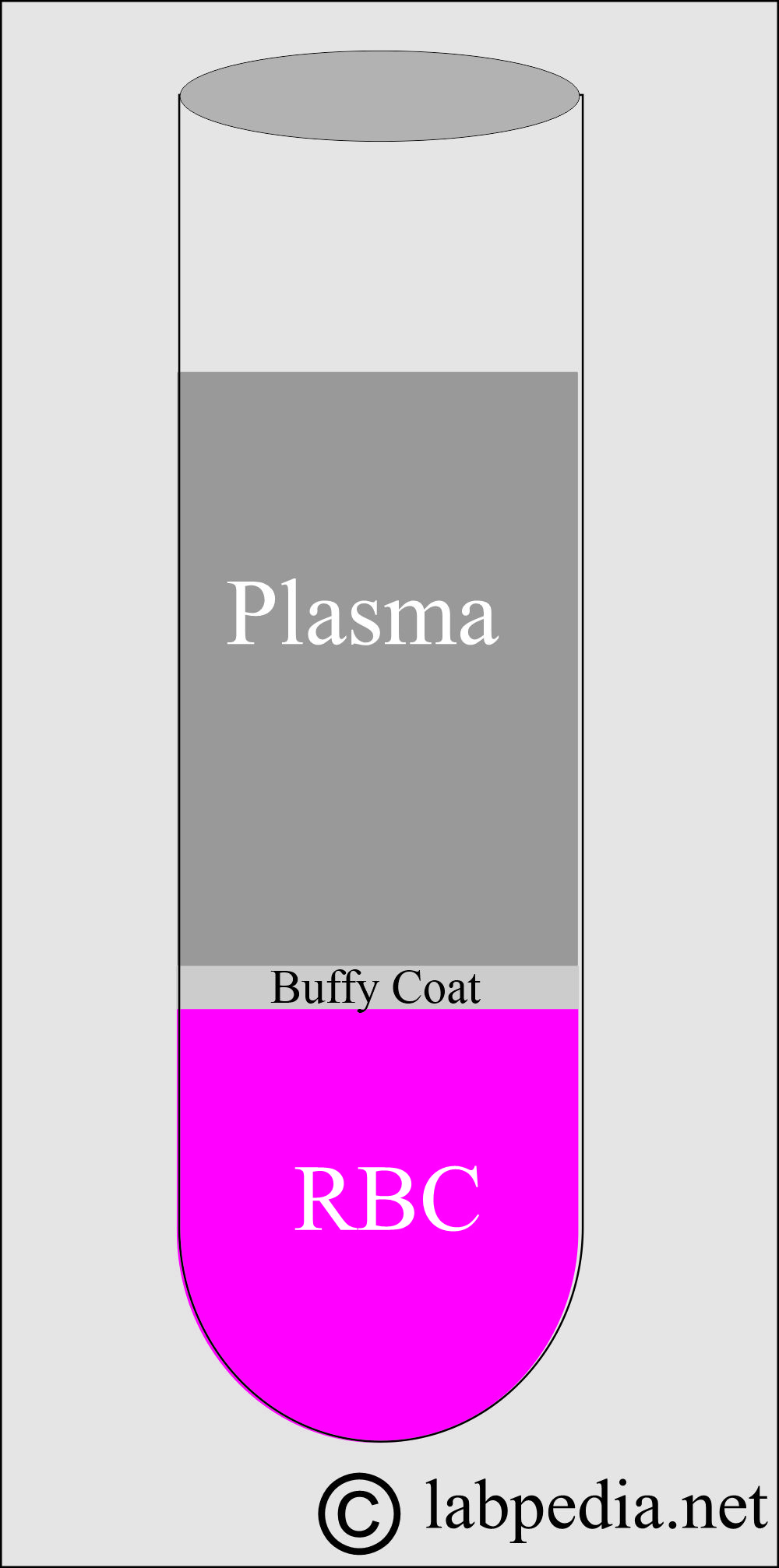
Plasma
How will you define plasma?
- Plasma is 5% of the total body volume.
- This pale yellow liquid contains RBCs, white cells, and platelets.
- Plasma forms with the help of anticoagulants, which will prevent clotting.
- There is the presence of fibrinogen in the plasma.
What are the causes of plasma colors?
- Plasma may have different colors due to the following:
- Total bilirubin will change color to yellow because of jaundice.
- Increased fats and lipemia change color.
- Plasma may be pink due to the presence of free hemoglobin.
- Plasma is green in color due to the presence of ceruloplasmin.
- Bacterial contamination also changed the color and appearance of the plasma.
- Excess drugs may alter the color of plasma.
- The orange-pink color is caused by carotenoids.
- Plasma color may change in various diseases.
What are the contents of the plasma?
| Substances in the plasma | Contents of the plasma |
|
|
| Cations | |
|
|
|
|
|
|
|
|
|
|
|
|
| Anions | |
|
|
|
|
|
|
|
|
|
|
|
|
|
|
Serum
How will you define serum?
- This is a clear fluid that is separated from the clotted blood. There are no RBCs, white cells, or platelets. There is no need for anticoagulants.
- It is a liquid portion of the blood that has been allowed to clot, or plasma without fibrinogen.
- Clotted blood is kept at 37 °C for at least 20 minutes and then centrifuged.
- The upper portion is called serum.
- There is no fibrinogen.
Buffy Coat
How will you define a Buffy coat?
- This is the middle layer between the plasma and RBCs.
- This will contain white cells and platelets.
What are the contents of plasma and serum?
| Contents of plasma and serum | Plasma | Serum |
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
What is the difference between plasma and serum?
Characteristics |
Plasma |
Serum |
|
|
|
|
|
|
|
|
|
How will you compare plasma and serum in terms of their values?
| Chemical substances | Plasma values >than serum | Plasma values are< than serum. | No difference in the value of serum and plasma |
| Calcium | 0.9% | ||
| Chloride | 0.2% | ||
| Total protein | 4% | ||
| LDH | 2.7% | ||
| Albumin | 1.3% | ||
| SGOT | 0.9% | ||
| Alkaline phosphatase | 1.6% | ||
| glucose | 5.1% | ||
| Bicarbonate | 1.8% | ||
| Sodium | 0.1% | ||
| Phosphate | 7% | ||
| Potassium | 8.4% | ||
| Urea | 0.6% | ||
| Uric acid | 0.2% | ||
| Bilirubin | |||
| Creatinine | |||
| Cholesterol |
How will you summarize the blood samples?
| Type of blood sample | Description | Where to use |
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
What is the purpose of anticoagulants?
- To prepare whole blood or plasma, anticoagulants are required.
- The anticoagulants are added to the container before collecting the blood sample.
- These are used to prepare whole blood or plasma.
What samples should be rejected?
- Sample with lipemia.
- Sample showing hemolysis.
- Specimens with contamination, such as those resulting from improper cleaning.
- The sample quantity is insufficient for the proper ratio required for the tests.
What are the Anticoagulants used in routine?
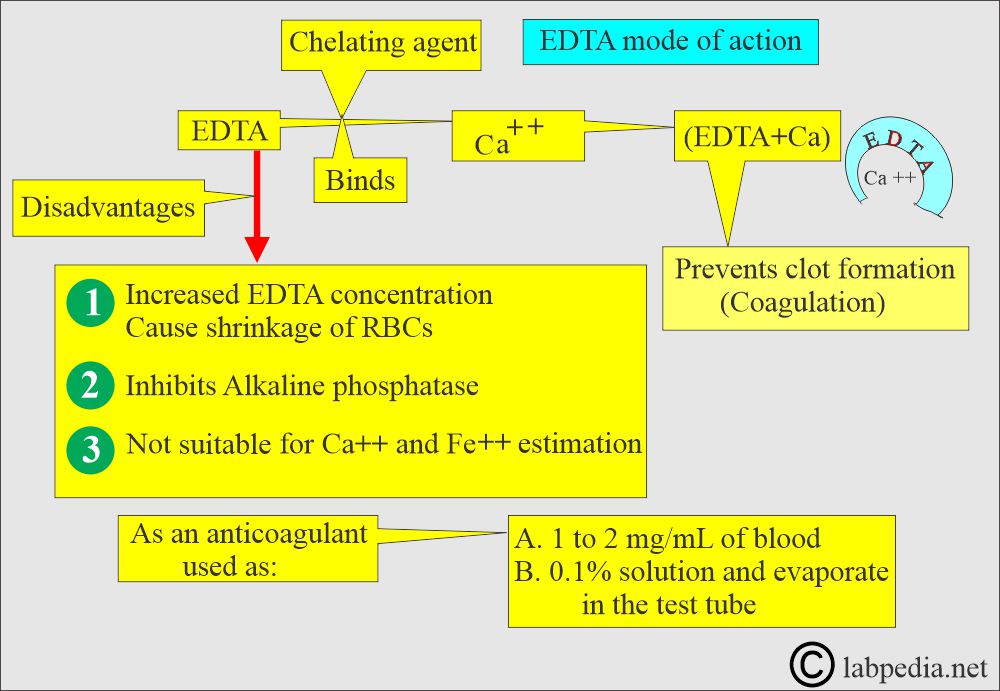
EDTA (Ethylenediaminetetraacetic acid)
How will you define EDTA?
- EDTA is a chelating agent that binds calcium.
What are the indications for EDTA?
- This is useful for the hematological examination.
- It is used for cell count, hematocrit, hemoglobin estimation, and differential cell count.
- EDTA is used as a disodium or dipotassium salt.
- Primarily, potassium EDTA is used as an anticoagulant, recommended for use in hematology studies.
- This is more soluble.
What is the Mechanism of action of EDTA?
- EDTA is a chelating agent that binds the calcium needed for coagulation. Chelation prevents coagulation.
- It is effective at a final blood concentration of 1 to 2 mg /mL.
- This can be used as a powder or solution and added to vials. Let it dry.
- It is used as disodium, dipotassium, or tripotassium salt.
How will you prepare a solution of EDTA?
- An EDTA solution of 0.1% can be prepared and used. Let it evaporate at room temperature.
- Or 1.5 mg/mL.
- More than 2 mg/mL causes cell shrinkage.
What are the advantages of EDTA?
- EDTA preserves the morphology of the blood cell structure.
- This is the anticoagulant of choice for hematocrit, Hb, and differential count.
- This is the best anticoagulant for peripheral blood smears and studies.
- It has little effect on the various tests.
- They produce less shrinkage of RBCs.
- There is a lesser increase in cell volume after keeping the blood.
What are the drawbacks of EDTA?
- It inhibits the activities of alkaline phosphatase, creatine kinase, and leucine aminopeptidase.
- EDTA is not suitable for Calcium and iron estimation.
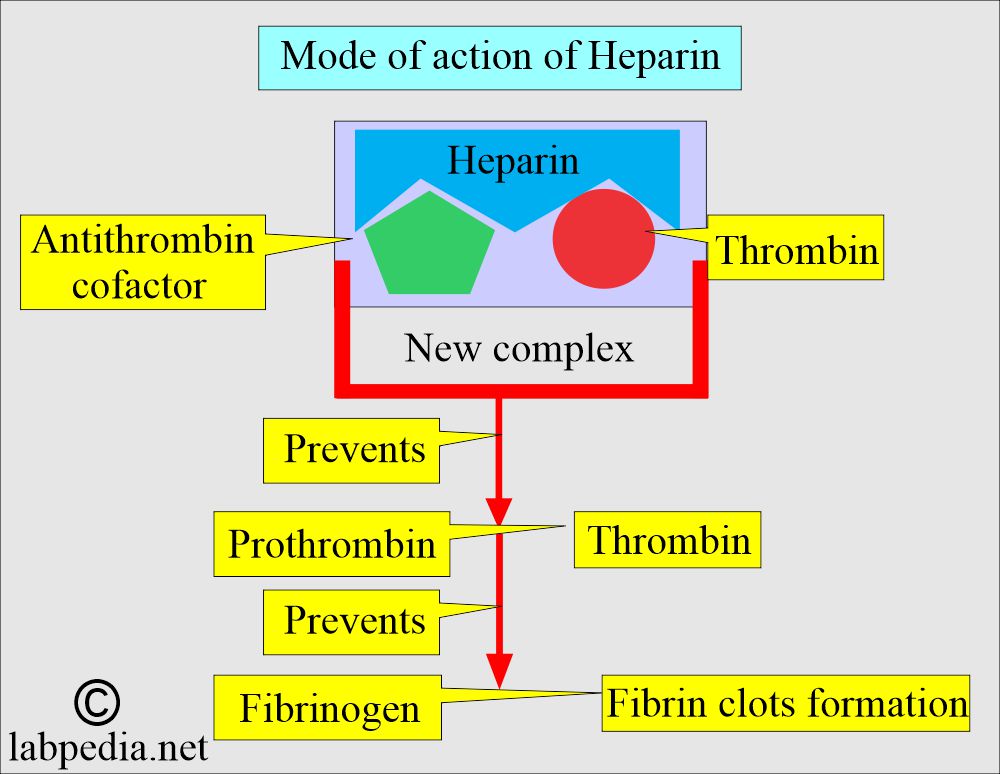
Heparin
What are the indications for Heparin?
- This is used in the treatment of DVT (deep vein thrombosis).
- It is used in pulmonary embolism.
- This is also used in unstable angina.
- This is used as a prophylactic drug in venous thrombosis.
- If needed in pregnancy, this is the drug of choice because it can not cross the placenta.
- This is used in cardiopulmonary bypass surgery. This will maintain the patency of the blood vessels.
- It can be used in DIC if there are predominantly vasoocclusive manifestations.
- Low-molecular-weight heparin is administered subcutaneously because it has a longer half-life than normal heparin.
- A prophylactic single dose is needed.
- Lastly, it is used as an anticoagulant and is primarily used in hematology.
What are the properties of Heparin?
- This is an anticoagulant and causes the least interference with the test.
- This is theoretically the best anticoagulant because it is a normal blood component and does not introduce any foreign contaminants to the blood specimen.
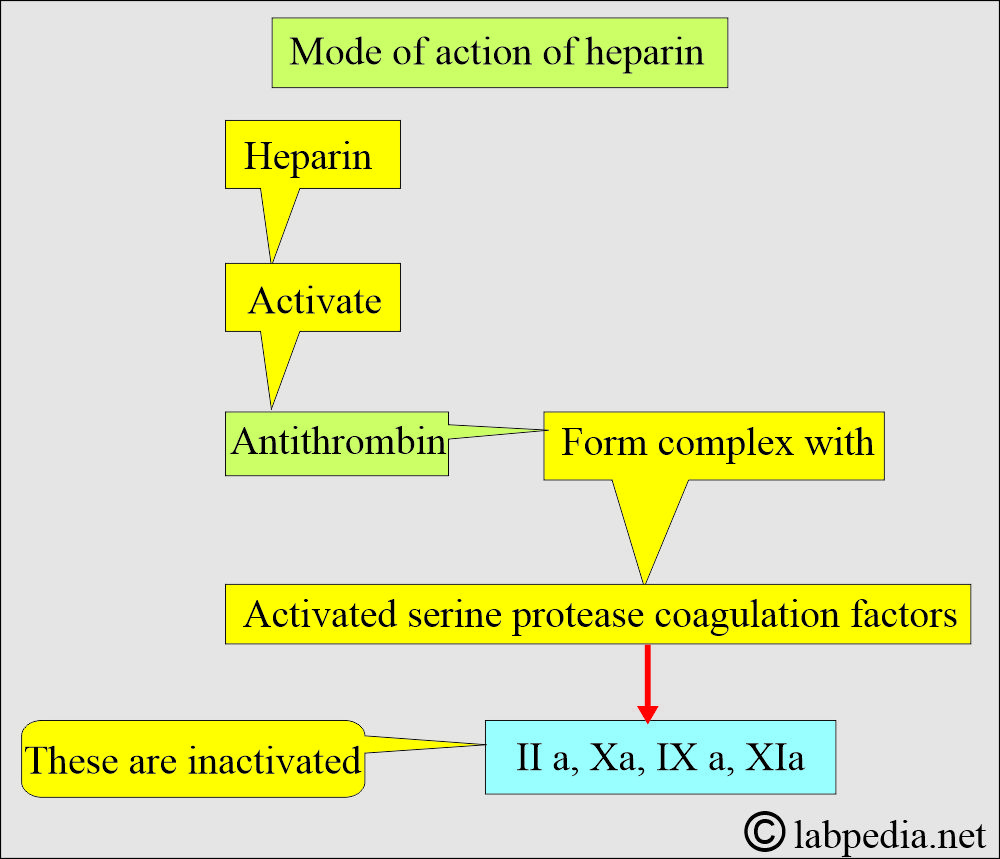
- This acidic mucopolysaccharide, with a molecular weight of 15,000 to 18,000, is a blood coagulation inhibitor that potentiates antithrombin activity.
- This is more costly than the others.
- It is present in powder form but is hygroscopic and dissolves rapidly.
- Mucoitin poly sulfuric acid is available as sodium, potassium, lithium, and ammonium salts.
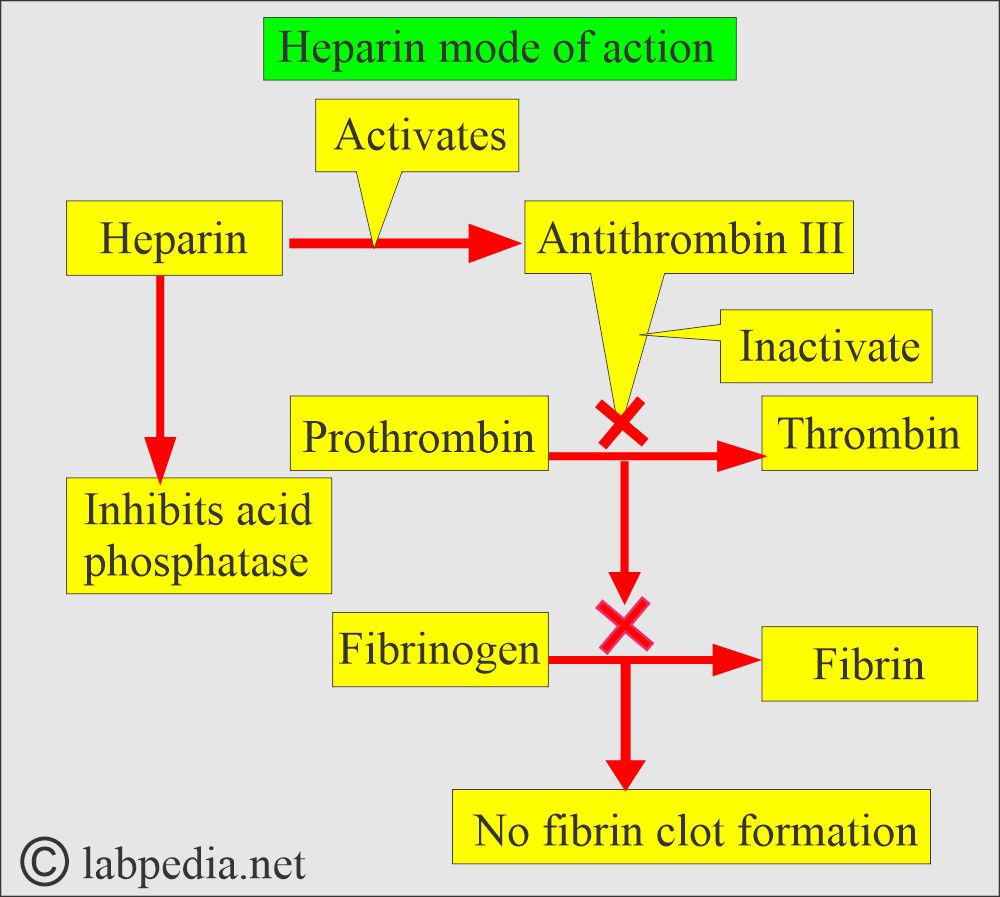
What is the mechanism of action of heparin?
- The GI tract does not absorb it, so it is administered by injection in the case of therapy.
- Heparin accelerates the action of antithrombin III, neutralizing thrombin and thereby preventing fibrin formation from fibrinogen.
- It forms the thrombin-antithrombin-heparin complex, preventing fibrin clot formation.
- It prevents coagulation for 24 hours by neutralizing the thrombin, thus preventing the formation of fibrin clots from the fibrinogen.
How will you collect the blood with heparin?
- Each test tube contains 0.2 mg/mL of heparin in the blood.
- Or 20 units of heparin for 1 mL of blood (in another reference, 15 U/mL).
- Or a drop of heparin is drawn into the syringe.
- Or simply coating the inside of the tubes or syringe is enough for the anticoagulant effect.
- After collecting the blood, invert the tubes 5 to 7 times to ensure proper mixing.
What are the advantages of heparin?
- This is the best anticoagulant to use when minimal hemolysis is desired, for example, when estimating sodium and potassium levels.
- This is the best anticoagulant to estimate pH, blood gases, electrolytes, and ionized calcium.
What are the drawbacks of heparin?
- It is costly.
- It inhibits the acid phosphatase activity.
- It provides a blue background for Wright’s stain smears, making it unsuitable for peripheral blood smear interpretation.
- It also affects the binding of triiodothyronine and thyroxine to their carrier protein and produces a higher free concentration of these hormones.
- It interferes with the binding of calcium to EDTA.
- It is not used for coagulation and hematology studies.
- Ammonium heparin affects the RBC volume.
Sodium Citrate
How will you define sodium citrate?
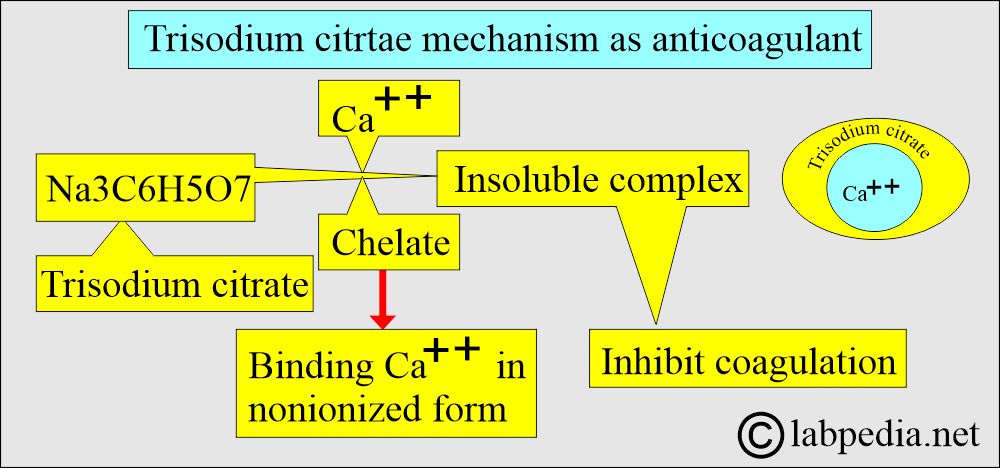
- Citrate is used as trisodium citrate salt.
- It is a white hygroscopic crystalline powder.
What are the indications of Sodium citrate?
- Sodium citrate is widely used for coagulation studies.
- For PT and PTT.
- The sample can be used for ESR by the Westergren method.
What is the mechanism of action of Sodium citrate?
- It is used in solution form.
- This will chelate calcium. Inactivates Ca++ ions.
- This will prevent the rapid deterioration of labile coagulation factors, such as factor V and factor VII.
How will you prepare a Sodium citrate solution, and what are its uses?
- Trisodium citrate 3.2 to 3.8 g/dL (3.2% solution).
- Mix well 3.8 grams of trisodium citrate in distilled water.
- This can be used as 0.109 mg/mL.
- In blood, the ratio is 1:9, where 9 parts are blood and 1 part is sodium citrate.
- PT and PTT Blood = Sodium citrate = 9 : 1 parts (blood nine parts: sodium citrate 1 part)
-
- ESR = Blood: Sodium citrate = 4:1 (1.6 mL of blood: o.4 mL Sodium citrate).
-
What are the drawbacks of sodium citrate?
- This is used in liquid form (liquid anticoagulant).
- This is not an ideal anticoagulant for a complete blood count examination.
- This is not suitable for estimating calcium.
- It inhibits aminotransferase and alkaline phosphatase.
- This will stimulate acid phosphatase when phenyl phosphate is used as the substrate.
- It has little value in clinical chemistry.
Potassium Oxalate:
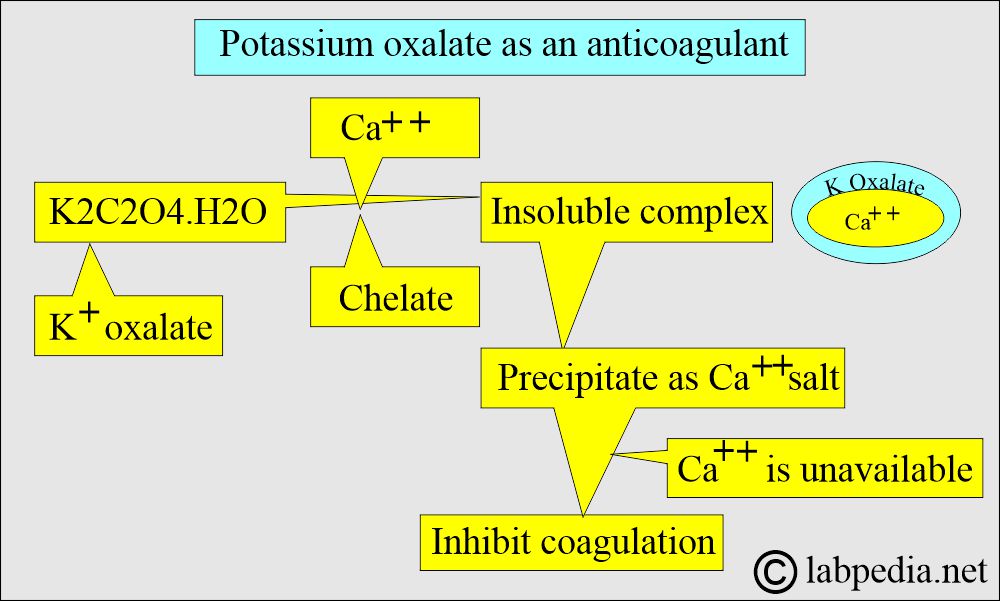
What is the mechanism of Potassium oxalate?
- This may be a sodium, potassium, ammonium, or lithium oxalate salt used as an anticoagulant.
- This forms an insoluble complex with calcium ions (precipitate with calcium as a salt).
- This is the most commonly used oxalate salt as an anticoagulant in powder form.
How to prepare K-oxalate Solution?
- Potassium oxalate is used at a concentration of 1 to 2 mg/mL of blood.
- Bulk solution: when you mix 30 grams per liter in distilled water.
- Now add a few drops to the test tube side and dry it in the oven at below 100 °C.
- The combination of ammonium/potassium oxalate does not lead to shrinkage of the RBCs.
- While other oxalates cause shrinkage.
What are the drawbacks of potassium oxalate?
- If the concentration is greater than 3 mg/mL, there is a chance of hemolysis.
- There is a 10% reduction in hematocrit.
- Oxalates inhibit enzymes like acid phosphatase, alkaline phosphatase, amylase, and LDH.
- It may cause the precipitation of calcium as oxalate salt.
Sodium Fluoride
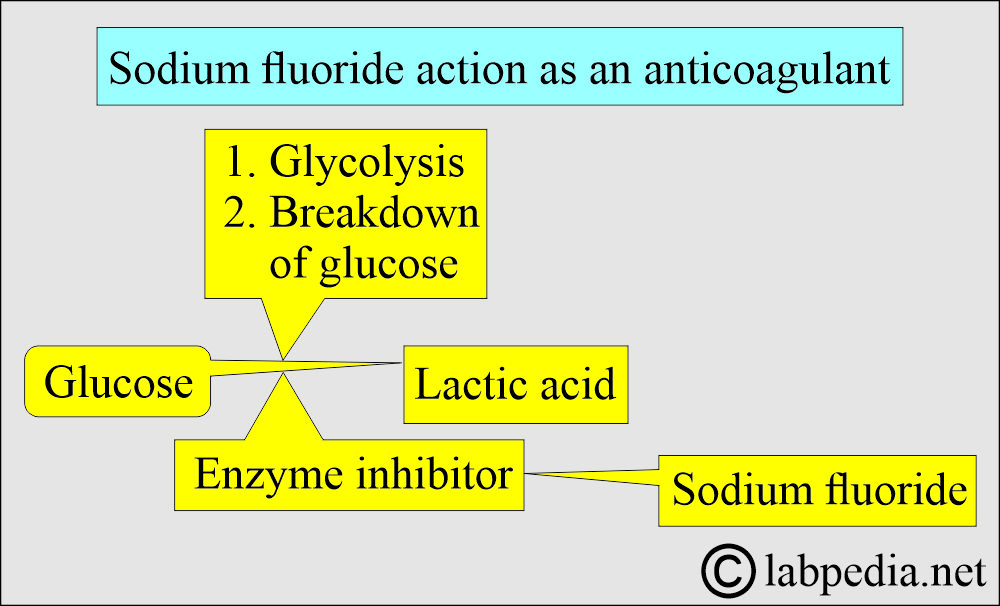
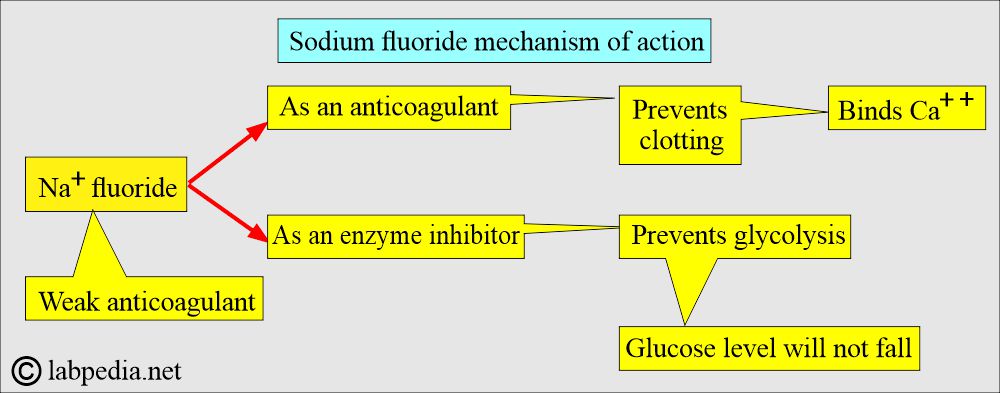
- This is a weak anticoagulant, but it utilizes an antiglycolytic agent to preserve glucose.
- This inhibits the system involved in glycolysis and preserves the glucose.
- This can be used as a dry additive.
What is the Mechanism of action of Sodium fluoride?
- It acts in two ways:
- As an anticoagulant, it binds calcium.
- As an enzyme inhibitor that prevents the glycolytic enzyme from destroying the glucose.
- Sodium fluoride acts after the enolase, so it will not be effective in the first 1 to 2 hours. It prevents glycolysis after this period.
- Glucose levels can drop during this period, typically by around 10 mg/dL.
- Transporting on ice and rapid serum separation within 30 minutes can prevent glycolysis. There is no need to add sodium fluoride.
- Not good for clinical chemistry tests.
How to prepare sodium fluoride Solution:
- This is effective at a blood concentration of 2 mg/mL, when used in combination with another anticoagulant, such as potassium oxalate.
- When used alone, a concentration greater than 2 mg/mL is required.
- This can be used in combination with oxalate as a fluoride-oxalate mixture.
- Most specimens are preserved at 25 °C for 24 hours and at 4 °C for 48 hours.
- Sodium fluoride is poorly soluble, so mix blood thoroughly before effective anti-glycolysis occurs.
- This is mainly used for glucose estimation.
- The rate of decrease is faster in newborns due to the increased metabolic activity of white blood cells.
What are the drawbacks of Sodium Fluoride?
- This is also an inhibitor of many enzymes.
- Also, use urease for the estimation of urea.
Sodium Iodoacetate
- This is an effective antiglycolytic agent and a substitute for sodium fluoride.
- This does not affect urease activity for glucose and blood urea levels; instead, sodium fluoride or a single sample is used.
How will you use Sodium Iodoacetate?
- It can be used at a concentration of 2 g/L and is an effective glycolytic agent.
- This may be substituted for sodium fluoride.
- This does not affect urease.
What are the drawbacks of Sodium Iodoacetate?
- It inhibits creatine kinase but does not affect other chemistry tests.
What are the various anticoagulants and types of blood samples?
| Type of the blood sample | Anticoagulant added | Mechanism of action | Use of the blood sample |
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
What are the adverse effects of the additives?
- The additive may contain the substance to be tested, like Na+oxalate, to estimate Na+.
- The additive may remove the component being tested, such as oxalate, which removes calcium.
- The additive may affect enzymes, such as those affected by Na+ fluoride. This may destroy many enzymes.
- A small amount of the anticoagulant gives rise to microclots, interfering with the cell count.
- The additive may distort the cells, such as oxalate, and alter cell morphology, as seen in RBCs, which become crenated. While WBCs show vacuoles. Lymphocytes and monocytes will have distorted shapes.
- If the excess quantity is used, it will dilute the substance being tested.
Questions and answers:
Question 1: Why is sodium fluoride a good anticoagulant for estimating glucose?
Question 2: What is the difference between plasma and serum?

Good
Thanks
Good explanation on the anticoagulations of analytes in the Clinical Chemistry lab
Thanks
I agree with you
Thanks.
It’s hard to say
Sir please provide pdf
Please you can do a PDF file yourself.
Really appreciate this sir, can you make it to PDF so that we can download it.. Thank you
Thanks for the appreciation. We are considering but don’t have many options at this time.
Thank you for this explanation. I am having trouble finding a good reference regarding depressed glucose results due to improper mixing in grey tops. The statement “Sodium fluoride is poorly soluble, so mix blood thoroughly before effective anti-glycolysis occurs” makes complete sense to explain why improper mixing could yield lower results. Do you have any further reference for this effect?
Sodium fluoride, according to one reference weak anticoagulant, so you can use it with another anticoagulant. Its main function is preservative by inhibiting the enzyme system involved in glycolysis. Its concentration is 2 mg/mL when mixed with another anticoagulant, but you need 3 to 5 times greater concentration when used alone than the usual 2 mg/mL. This higher concentration and inhibition of the glycolytic cycle is likely to cause a fluid shift. This can not be justified to use for other chemistry tests.
Thank you so much for this outline. It’s a wonderful explanation of anticoagulants & their mechanisms of action. I’ve saved it for my own references purposes. Perfect for new techs & phlebs or as a refresh for anyone who might need it.
Thanks.
Thanks you sir
Welcome.
Sir I am writing a book can I use some images of your labpedia.net
in my book because sir in a image you explain very well so sir pleas
Please see your email.
Thank you So much sir. You are very soft heart person.
well summarized notes, thank you
Thanks.
Hi sir,
I am writing a report on testing chloride in the body but I’m not sure of the method, sample types, the reagents or the preservatives involved.
Please see this link:
https://labpedia.net/chloride-blood-chloride-cl%c2%af-and-cystic-fibrosis/
Thanks for this good information .Sir i want to know the term what is true glucose?
True glucose is estimated by the enzymatic method. At the same time, Benedict’s reaction gives other reducing substances.
True glucose is measured by the enzymatic method. In comparison, Benedict’s solution estimates all reducing substances.
Hello doc Riaz. May I ask how can I preserve a serum?
You can keep serum for short period in the fridge. For a longer period freeze the serum. If you want to keep it for more than 6 months freeze it and keep it at -20C (or -70C).
Sir, I must really commend your work. I would love to make more research on this but I don’t seem to find the references you used for this work
This topic is covered in various books and my personal experience in my practice.
hello sir
Please let me know if I can be of any help.
hello sir ,i am manufacturer of blood collection tube, I need solution making formula for anticoagulants like EDTA,SODIYAM FLORIDE and CLOT activator with concentration for best result test.please help
https://labpedia.net/blood-sample-types-anticoagulants-preservatives-adverse-effect-of-additives/
Please read this article; most solution preparations are given in this article.
This is a good, educative and impressive website for medical laboratory student. It’s very easy to read and understand.
Thanks.
Thank you for this thread. It is very helpful for a pathology resident. I wish you had “advantages” for all the anticoagulants. This would make it easier to compare all of them.
Please read carefully; I have discussed the advantages and disadvantages of the anticoagulants.
Thank you sir for your valuable inputs.. Its really helpful.. Sir can you please guide us on clot activator reagents.. how can we prepare clot activator solution ??
I think there are ready made tubes with clot activator.
There are:
1. Silica-based clot activator.
2. Thrombin clot activators.
I will suggest ready-made test tubes.
¡Excelente trabajo! Soy Estudiante de Bacteriología y debo reconocer el fundamento de cada tubo. ¡Saludos desde Colombia, Dr. Riaz!
Thanks.
Whether sodium sodium fluoride with oxalate tubes can be used for haematology tests also?
Please see these comments about oxalate for hematology.
Oxalate is not good for hematology studies.
Drawbacks of potassium oxalate
If the concentration is >3 mg/mL, there are chances for hemolysis.
There is a reduction of 10% in hematocrit.
Oxalates inhibit enzymes like acid phosphatase, alkaline phosphatase, amylase, and LDH.
It may cause the precipitation of calcium as oxalate salt.
Hello sir,about peripheral blood and venous blood, do we need to use different proportions of heparin lithium anticoagulant tubes for biochemical testing? I see that the market has described the use of peripheral blood and venous blood, and their tube anticoagulant ratio is not the same
Peripheral blood smear is done on the venous blood. For biochemical testing the best sample is serum. Plasma is not preferred sample.
Sorry,I should describe Capillary blood and venous blood.
When you take capillary blood then you will make direct smear. No need to put into anticoagulant. Capillary blood is mostly used directly.
Please see this topic:
https://labpedia.net/blood-sample-types-anticoagulants-preservatives-adverse-effect-of-additives/