Blood Culture, its Procedure and Interpretations
Blood Culture
What sample is needed for Blood Culture?
- >10 ml of blood from the patient is required; the best time is during fever.
- This is collected in the culture bottle.
What are the recommendations for the blood culture?
- Inoculation of Blood <5 ml shows markedly reduced yield.
- One reference recommends 20 to 30 mL of blood/per culture.
- Some suspected organisms may need more blood.
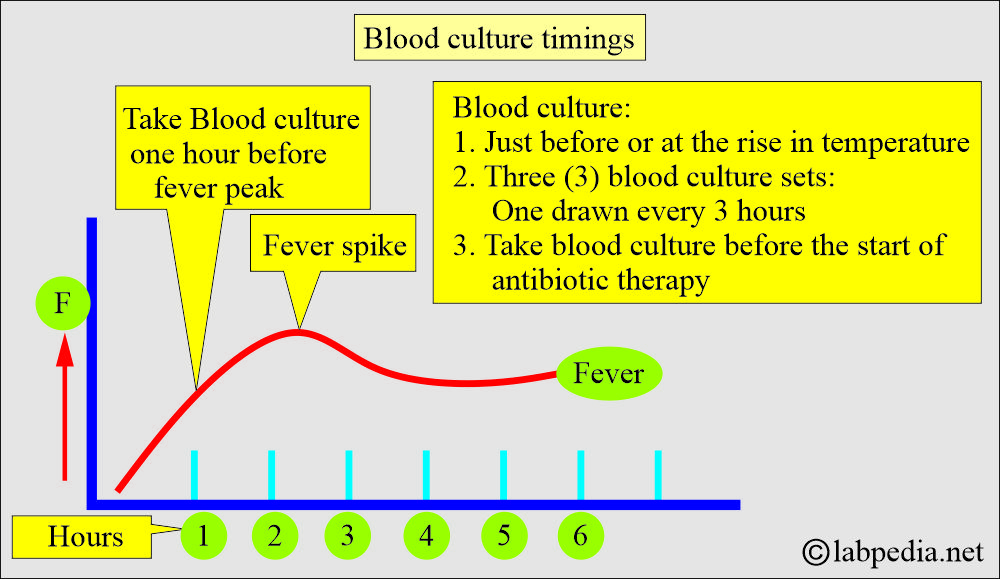
- Take the blood sample immediately after the onset of fever and chills.
- The best time to take a blood sample is one hour before the fever spike. This spike time occurs at approximately the same time every day.
- It is better to get three samples during the fever. These samples may be taken from both arms.
- Take 2 to 3 cultures per septic episode or per 24-hour period.
- In continuous bacteremia, such as endocarditis, the timing of the sample is unimportant.
- In the case of intermittent bacteremia, take a sample at the onset of fever and continue taking samples up to three times in 24 hours.
- Paired culture, aerobic and anaerobic samples are taken, ideally from the opposite arms.
- Clean the site to avoid contamination by 70% Alcohol. It needs at least 2 minutes to be effective.
- Then clean with the 2% iodine.
- If the patient is sensitive to iodine, then cleaning with alcohol is enough.
- For a fever of unknown origin, draw two blood samples.
- A quantity of less than one ml is insufficient to detect bacterial infection.
- The culture needs at least 72 hours for the report.
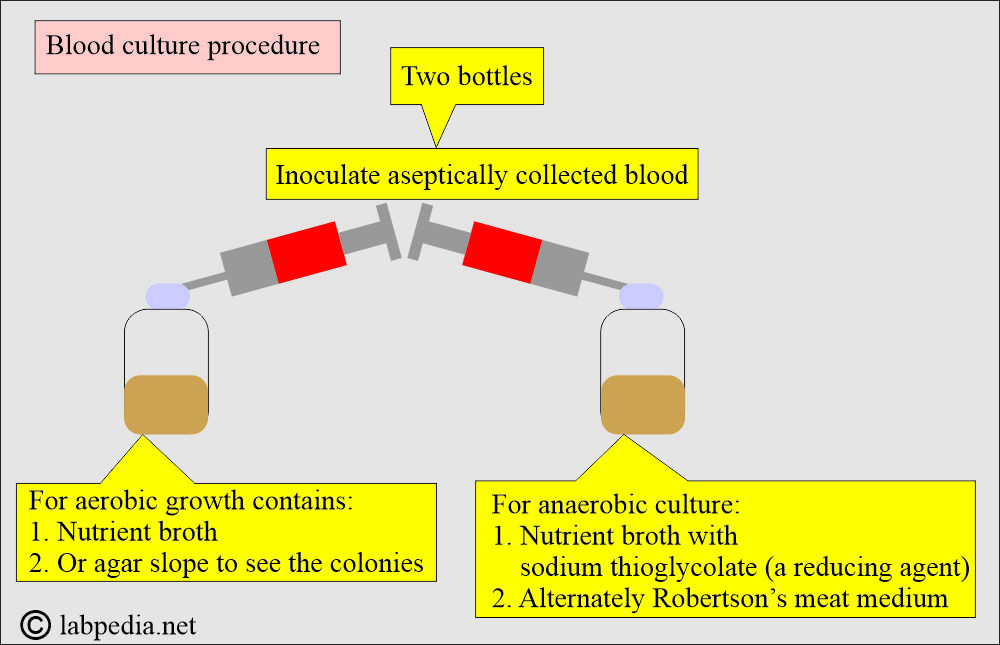
- Blood, with or without microorganisms, is collected into bottles for growth in either an aerobic or anaerobic environment.
What are the advantages of more blood samples?
- More culture samples increase the possibility of a positive blood culture.
- Positive cultures in 2 or 3 separate samples indicate continuous bacteremia that is typically found in bacterial endocarditis.
- Positive cultures in 2 or 3 samples indicate that there is no contamination. This is particularly important in prophylactic valve endocarditis, where S. epidermidis is commonly found.
What are the precautions for blood culture?
- A strict aseptic technique must be observed.
- Antimicrobial treatment before collecting the blood sample may result in a negative culture report. This may be negative even in bacteremia.
- Using inappropriate culture media or the container may interfere with aerobic growth.
- Inadequate time for the culture, temperature, or culture conditions may fail to provide an adequate amount of bacteria for its identification.
- If there is patient skin contamination for the culture.
- Don’t draw blood from the I/V catheter unless no veins are found.
- In infants, blood is taken from an umbilical artery catheter.
What are the indications for blood culture?
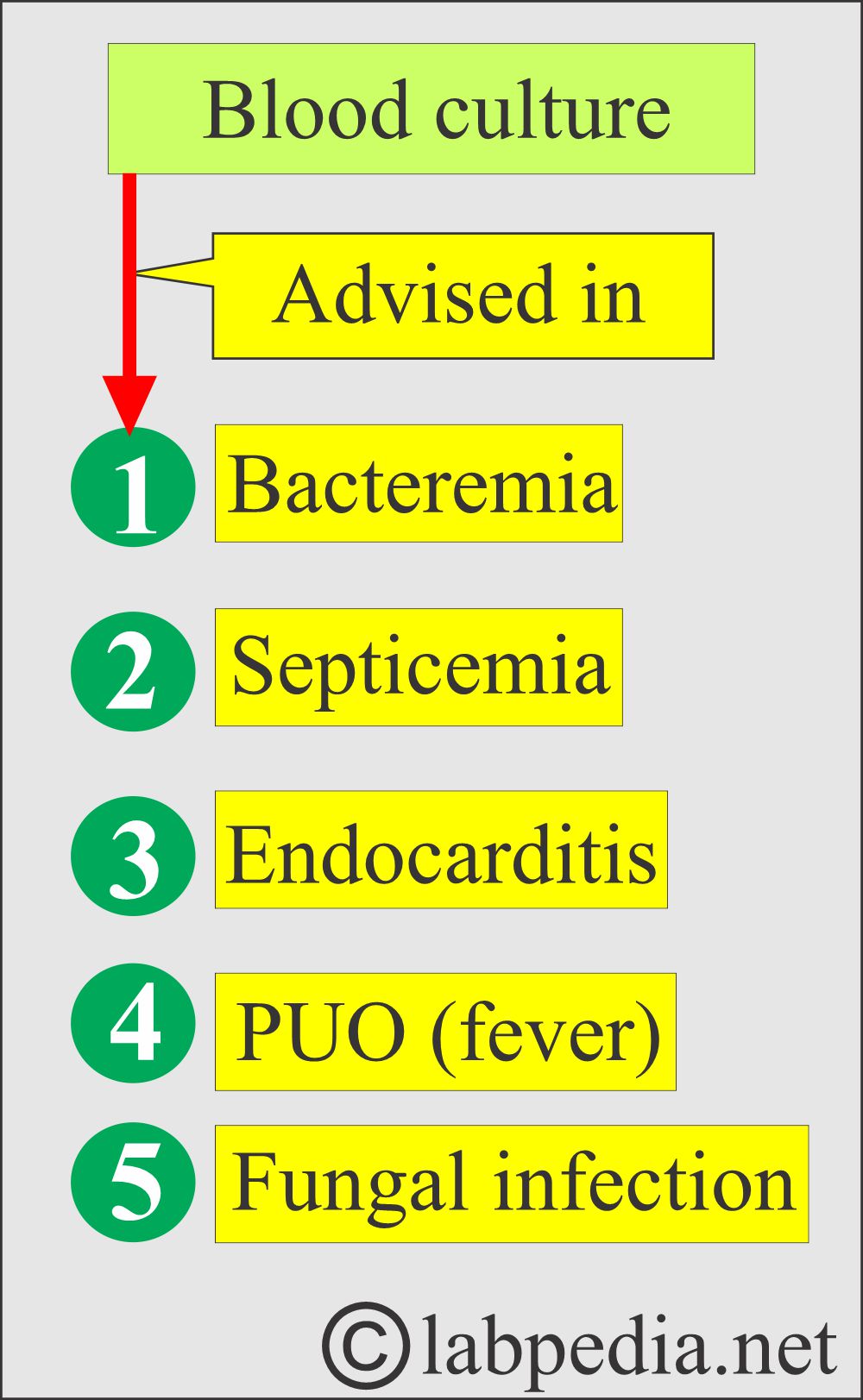
- Blood culture is advised when there is a suspicion of bacteremia or septicemia.
- Find a bacterial infection that has spread into the blood, such as meningitis, osteomyelitis, pneumonia, a kidney infection, or sepsis.
- To find the type of bacteria in a culture.
- Find a fungal infection, such as yeast, in the blood.
- Check for endocarditis, an infection caused by bacteria that live on the heart’s valves.
- Repeated blood cultures are needed in case of endocarditis.
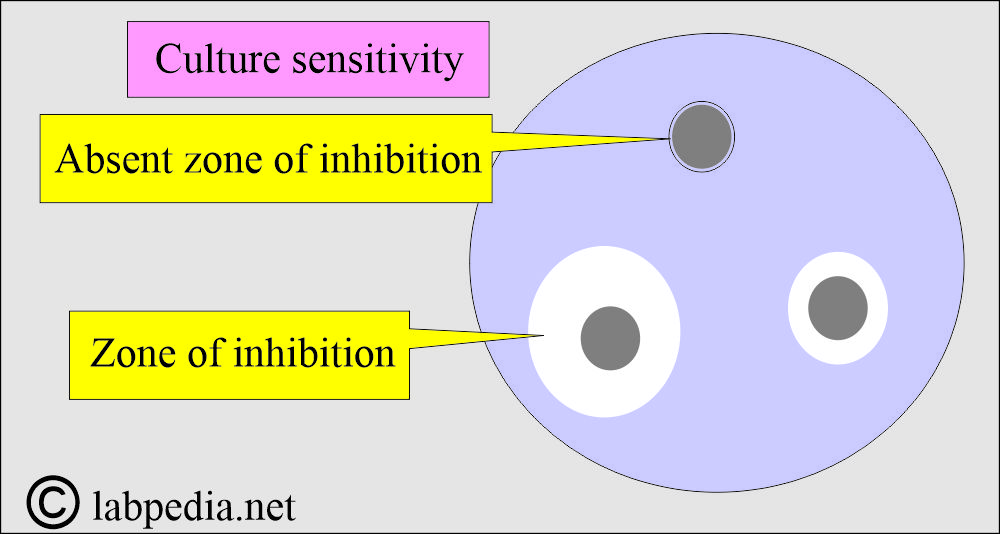
- Find the best antibiotics to kill the bacteria. This is called sensitivity testing.
- Find the cause of an unexplained fever or shock.
- In an unexplained fever (PUO) of several days duration.
- In patients with chills.
- Infected burn.
- Urinary tract infection.
- Postoperative wound sepsis.
- Indwelling venous or arterial catheter.
- If bacteria are found in the culture, another test is often performed to determine the most effective antibiotic for killing the bacteria. This is called sensitivity or susceptibility testing.
- Sensitivity testing is crucial for treating blood infections effectively. This also helps prevent bacteria from becoming resistant to antibiotics.
What are the factors about Blood culture?
- Blood culture reports, which often identify microorganisms, typically require at least 24 hours.
- 67% of the pathogens are identified in 24 hours.
- 90% of the pathogens were identified within 72 hours.
- Fungi and mycobacteria may need more time, maybe weeks.
- Vascular catheter-related infections (bacteremia) account for at least 20% to 40% of all infections in hospitalized patients.
- After the growth, the organism is tested with various drugs impregnated discs.
- Sensitivity will take another 24 hours or more.
- This test finds the bacteria in the blood (bacteremia).
How will you define Bacteremia?
- Bacteremia is the presence of bacteria in the blood and various organs. It may be:
- Intermittent: These are periodic and often from a localized infection.
- Transient: These are short-term and may be seen after teeth brushing.
- Persistent: This refers to the continuous presence of bacteria, such as in endocarditis.
- Except in endocarditis or suppurative thrombophlebitis.
What are the causes of Bacteremia in different procedures?
| Procedure | Incidence (occurrence) |
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
What are the sources and causative agents of infections?
- Approximately 50% of cases show growth of gram-negative bacilli, and most of these are E. Coli.
- Staphylococcus aureus is the second most common organism.
- The most common site of entry is often associated with previous urinary tract infections.
- Other portals of entry follow surgery due to the use of instrumentation.
- Fungal endocarditis is most commonly due to Candida spp, followed by Torulopsis glabrata and Aspergillus spp.
- The mortality rate in septicemia may be as high as 20% in immunocompromised and debilitated patients.
What are the Clinical signs and symptoms of bacteremia?
- An episode of bacteremia is followed by:
- Chills.
- Fever.
- This is the best time to take the blood sample.
- S/S are accompanied by high fever and leukocytosis.
- Septic patients may be afebrile in 10% (4% to 18%) of the cases.
- These patients exhibit leukocytosis in 60% to 65% (42% to 76%) of cases.
- The band form may be increased from 70% to 75% in some cases.
- Total WBC count increases in 75% (66% to 92%) of the cases.
- Some patients may exhibit leukopenia in 10% (4% to 18%) of cases.
How will you perform the blood culture Procedure?
- Prepare a fresh blood film to rule out parasites, such as malaria, Borrelia, and Trypanosoma.
- The technique for the collection of blood for culture:
- Clean the skin from where the blood is taken.
- Can clean the skin with Betadine and then with 70% ethanol.
- Let the skin dry.
- Clean the top of the culture bottle with Betadine.
- This may be followed by 70% alcohol and let it dry.
- Take 10 to 15 mL of the blood from different sites.
- Discard the needle and attach a new sterile needle to inject the blood into the culture bottle.
- Inoculate the anaerobic bottle first, then the aerobic bottle.
- Mix gently after the inoculation.
- Multiple blood samples are taken. Usually, two to three samples are adequate.
- Take the blood sample when the patient has a high fever or is shivering.
- If one sample is positive and the other is negative, it will indicate contamination.
- If both culture media show the same bacterial growth, it indicates bacteremia.
- If the patient takes antibiotics, it should be reported to the lab.
- In this case, take a blood sample in resin, which will inhibit the effect of the antibiotics on bacterial growth.
- Take the blood sample before the next dose of antibiotics.
- Culture from the I/V catheter is always contaminated and should be avoided.
- If catheter sepsis is suspected, then culture from the IV catheter alone can be performed.
- Some lab. Prefers multiple sites to collect the blood.
- They take blood at various intervals of 0, 30, and 90 minutes.
- Multiple sites rule out skin contamination.
- The three blood culture samples yield is 99.9%.
- A sample of more than 3 does not improve positivity.
- In adults, take 10 mL of blood per bottle.
- Some lab prefers 10 to 15 mL of blood from all sites.
- Less than a 5 ml blood sample shows a less positive culture yield.
- Discard the syringe needle and use a new sterile needle to transfer the blood into the blood culture bottle.
- Culture the blood aerobically and anaerobically.
- First, add the blood to the anaerobic media.
- Gently mix the blood with blood culture media.
- Subculture these samples for at least 72 hours.
- After the growth, a sensitivity test determines the sensitive drugs for that growth.
- Antibiotic sensitivity tests show zones of inhibition of the growth around the disc impregnated with antibiotics.
- Resistance is shown by the growth of the organism right up to the disc.
How will you report the Blood culture?
- Negative culture reports when all cultures, subcultures, and Gram stain smears are negative.
- The blood culture report may be reported negative after 5 to 7 days of incubation.
- Bacteria need at least 24 hours to grow in the lab.
- By then, a preliminary report can be given.
- 48 to 72 hours are needed to identify the organism.
- Anaerobic organisms take a longer time.
- The virus can not be detected by blood culture.
- A definitive diagnosis is made in:
- Subacute bacterial endocarditis.
- Salmonellosis (Typhoid fever). The second and third weeks of typhoid fever are the best times for blood culture.
- After this period, positivity declines rapidly.
- Brucellosis.
- Blood culture is positive in 30% to 50% of the cases.
- This organism needs CO2, and growth is very slow on ordinary media.
- There are special media that assist the growth.
- Gonococcal infection (Gonococcemia).
- Chronic meningococcemia.
- Tularemia.
- Form of rat-bite fever.
What is important in blood culture reporting?
- When the first tube shows growth and the second tube is negative, it is presumed that the first tube may be contaminated.
- When both tubes show growth, that indicates bacteremia.
- If the patient is taking antibiotics, then take the blood before the next dose of antibiotics.
What are the possibilities of a positive culture report?
- Bacteroides.
- Brucella
- Enterobacteriaceae.
- Pseudomonas aeruginosa.
- H. influenzae.
- Listeria monocytogenes.
- Enterococcus.
- Streptococcal pneumoniae.
- Candida albicans.
- Clostridium perfringens.
- Staphylococcus aureus.
- Staphylococcus epidermidis.
- Streptococcus species (Beta-hemolyticus).
When do you need a Positive blood culture for definitive diagnosis?
- Subacute bacterial endocarditis.
- Salmonellosis (typhoid fever).
- Blood cultures are the best means of diagnosis during the first and second weeks of the infection.
- After that, the positivity will decline rapidly.
- Brucellosis.
- Chronic meningococcemia.
- Gonococcal infection (gonococcemia).
- Tularemia.
What are the causes of false-negative blood cultures?
- History of recent antibiotic therapy.
- Insufficient blood is taken for the blood culture.
- Most people take a 1:10 ratio of the blood to culture media to be adequate.
- Use of unsuitable culture media for anaerobes.
- Slow-growing bacteria may be missed in the first 72 hours.
- A blood sample was not taken at the appropriate time.
What percentage will you see a blood culture report in bacteremia (one study)?
| Type of the organism | Percent positivity |
|
|
|
|
|
|
|
|
|
|
|
|
|
|
What signs and symptoms will you observe in a patient with sepsis?
- Fever and chills.
- Less frequent urination.
- Nausea.
- There may be rapid breathing and tachycardia.
- Confusion.
- There may be a drop in blood pressure.
- There may be a failure of one or more organs.
Questions and answers:
Question 1: What is the best time to get blood culture in case of bacteremia?
Question 2: How many samples are needed for blood culture?