Blood banking:- part 4 – Blood Transfusion Reactions in Donor and Recipient, Treatment of Blood Reactions
Blood Transfusion Reactions
How will you define a blood transfusion reaction?
- Most of the blood donations proceed without any complications.
- Occasionally, a donor may have adverse effects on the donation.
- Blood transfusion reactions are defined as any adverse events resulting from the transfusion of blood or blood components.
How will you summarize the blood transfusion reactions?
| Type of reaction | Clinical presentation of the reaction |
|
|
|
|
|
|
|
|
Types of reactions in the donors:
What are the types of reaction in the Donor (due to blood donation)?
- Most of the donations proceed without any reaction. The reactions are:
- Vasovagal reactions.
- Some may have a psychological influence on the sight of blood.
- Neurophysiological response to actual blood donation.
- These reactions are divided according to the severity:
- Mild reactions.
- Moderate reactions.
- Severe reactions.
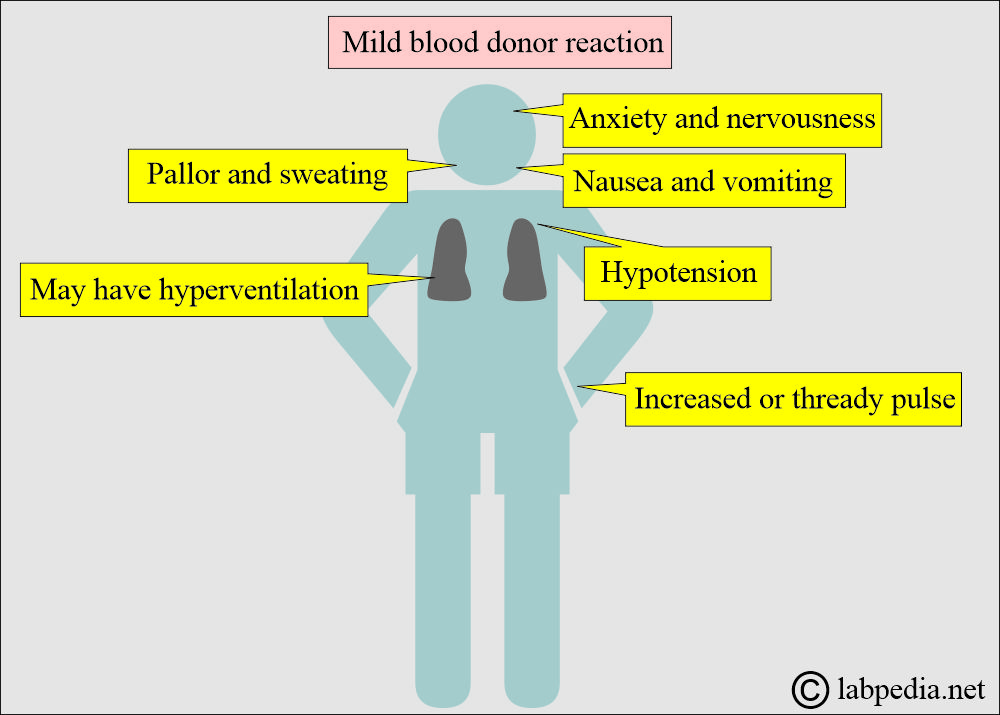
How will you discuss the mild reaction in the donor?
- Mild reactions are the most common reactions; most donors will have signs and symptoms of shock, but do not lose consciousness.
- Mostly, these are the following reactions that may be seen in donors.
- Donors may have anxiety and nervousness.
- There may be pallor and sweating.
- Some donors may feel a sense of warmth.
- Some donors may experience hyperventilation (increased respiratory rate).
- Some donors may have an increased or thready pulse.
- There may be hypotension.
- Some donors develop nausea and vomiting.
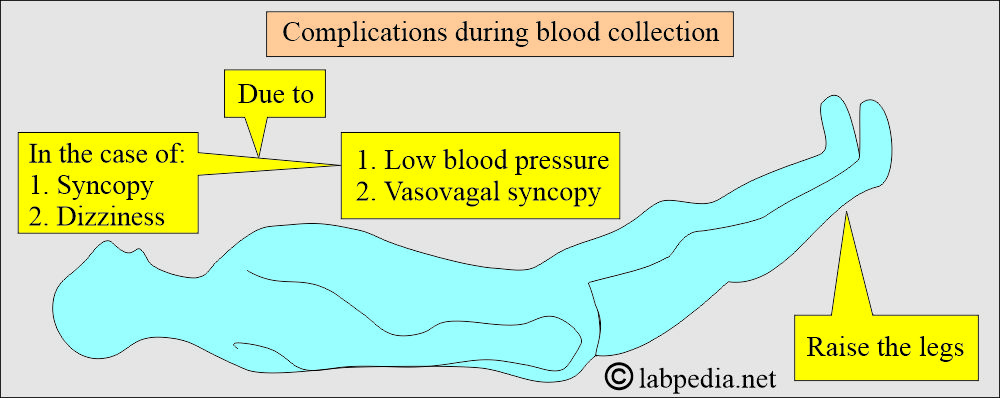
- How will you treat mild donor reactions?
- The best course of action is to stop the donation immediately.
- Remove the tourniquet and needle from the donor.
- In case of hyperventilation, ask the donor to breathe inside the bag, increasing the amount of CO2.
- Loosen the clothes, particularly the clothes around the neck like a necktie.
- Raise the legs of the donor (45 degrees at least).
-
- Reassure the donor and decrease his anxiety or stress.
- Keep an eye on the donor until they are fully recovered.
How will you discuss the moderate reaction in the donor?
- These signs and symptoms are like mild donor reactions, but the donor will lose consciousness.
- There will also be side effects of the mild reactions.
- Donors will have unconscious attacks.
- The pulse rate is low (decreased).
- There will be rapid, shallow respiration and hyperventilation.
- There will be hypotension, and the blood pressure may be as low as 60 mm Hg.
- How will you treat the moderate reactions?
- Take all the measures done in the mild reaction.
- Check BP, pulse, and respiration until these become normal.
- Give 95% oxygen and 5% CO2.
- Take the donor to a separate area so that other donors may not experience the same side effects.
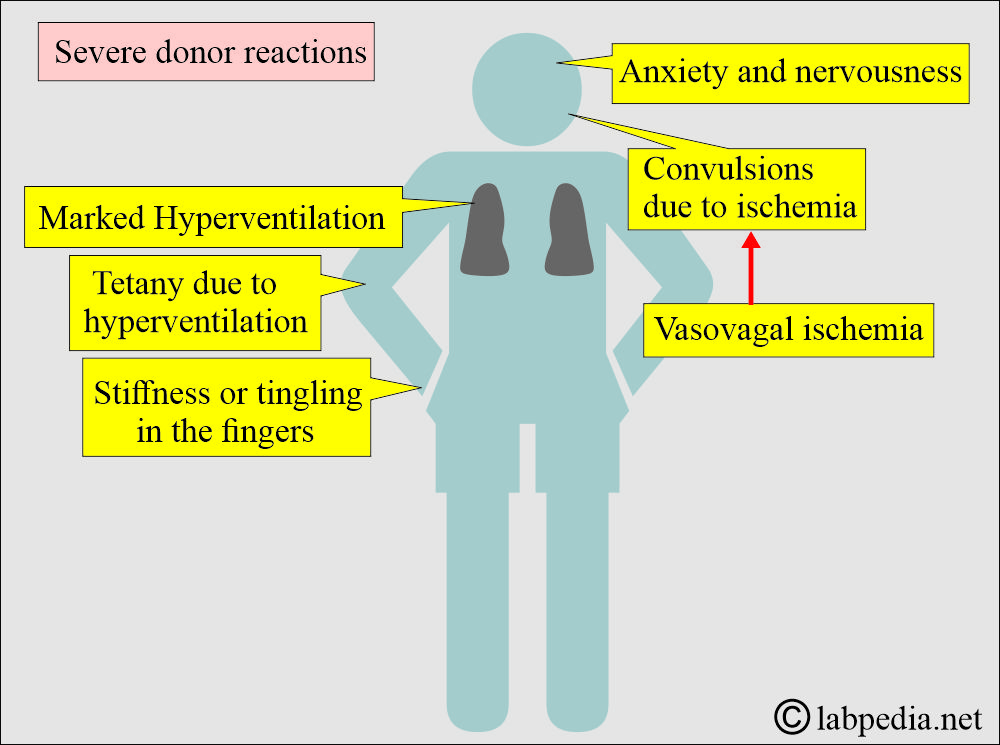
How will you discuss the severe reaction in the donor?
- These are different from the above due to the presence of convulsions. However, there will be the presence of mild and moderate symptoms and signs.
- The convulsions (seizures) are caused by cerebral ischemia associated with vasovagal syncope.
- Vasovagal ischemia is due to:
- Reduced blood flow to the brain due to deepening shock symptoms.
- Marked hyperventilation.
- Severe CO2 depletion can cause convulsions or tetany.
- Other severe signs and symptoms are:
- There is tetany due to hyperventilation.
- The donor may have stiffness or tingling in the fingers.
- The symptoms may increase and become pronounced convulsions if the CO2 intake increases.
- Fingers and thumbs may have spasms.
- Mild convulsions:
- The voice will fade out.
- There is a short lapse of consciousness.
- There will be involuntary movements of the arms and legs.
- Severe convulsions:
- Donors will have rigid bodies and tightly clenched teeth.
- There will be slight involuntary movements of the arms and the legs.
- The donor may experience temporary loss of breathing, followed by rapid breathing.
- How to treat the severe donor reactions?
- Ask the donor to breathe into the airbag.
- Try to prevent any injury to the donor during convulsions.
- Ensure adequate airways.
- Give 95% Oxygen and 5% CO2.
- Get a consultation from a medical doctor.
- If the donor develops cardiopulmonary problems, call for medical assistance immediately.
- In case of cardiac arrest, start cardiopulmonary resuscitation until medical help arrives.
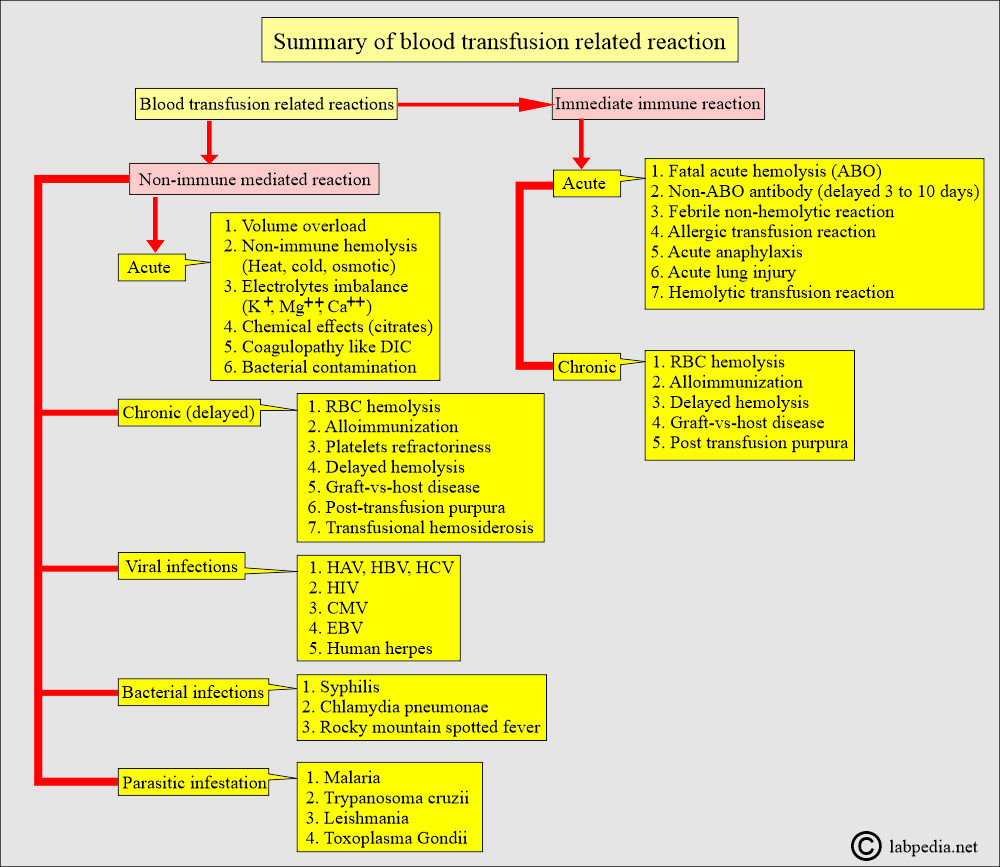
What are the Blood transfusion reactions in the recipient?
- Since no two individuals possess the same antigens on their RBCs, except in identical twins, there is always a risk of developing alloantibodies in the recipients.
- When alloimmunization occurs due to blood transfusion, it will have harmful consequences in future transfusions and pregnancy.
- The reactions of the recipient are:
- Urticaria is an allergic reaction.
- Anaphylactic type I hypersensitivity reaction.
- Febrile reactions.
- Hemolytic reactions.
- Infection due to a contaminated blood transfusion.
- Transmission of diseases like syphilis, malaria, viral hepatitis, and HIV.
Type of blood transfusion reaction in the recipient:
Acute reaction:
- This occurs within minutes to 24 hours of the transfusion.
Delayed reaction:
- These may develop in days to months to even years after the transfusion.
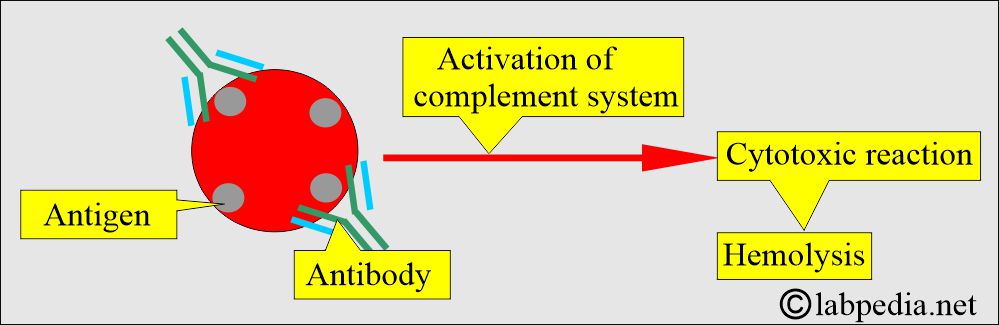
What is the basis of blood transfusion reactions in the recipient?
- These complications of blood transfusion reaction in the recipient may be due to various factors:
- Immune, Hemolytic transfusion reactions are due to RBCs in the recipient:
- These are quite uncommon due to advancements in serology. These are hardly 0.1% in the United States.
- These may be life-threatening complications.
- ABO incompatibility is a more common and fatal outcome than HIV and HCV.
- This usually occurs due to lab errors.
- This reaction is due to the presence of the Alloantigen on the RBCs and their reaction to the Alloantibody.
What are the signs and symptoms of a blood transfusion reaction in the recipient?
- Continuously monitor the recipient for any of the following signs and symptoms, which may indicate the onset of a blood reaction.
- An early sign may be allergic in the form of itching and hives.
- Fever. The patient’s temperature increases by 1°C, with only minor changes in other vital signs.
- Chills
- Nausea and vomiting.
- Chest, abdomen, or flank pain.
- Back pain.
- Hypotension or hypertension.
- The patient may go into shock.
- The feeling of heat along the vein where the blood is transfused.
- The feeling of constriction in the chest.
- Facial flushing.
- Hemoglobinuria.
- Oliguria.
- Dyspnea.
- Oozing blood from the wound.
- Anemia.
- Therefore, the patient may exhibit any of the above findings in the event of a blood transfusion reaction.
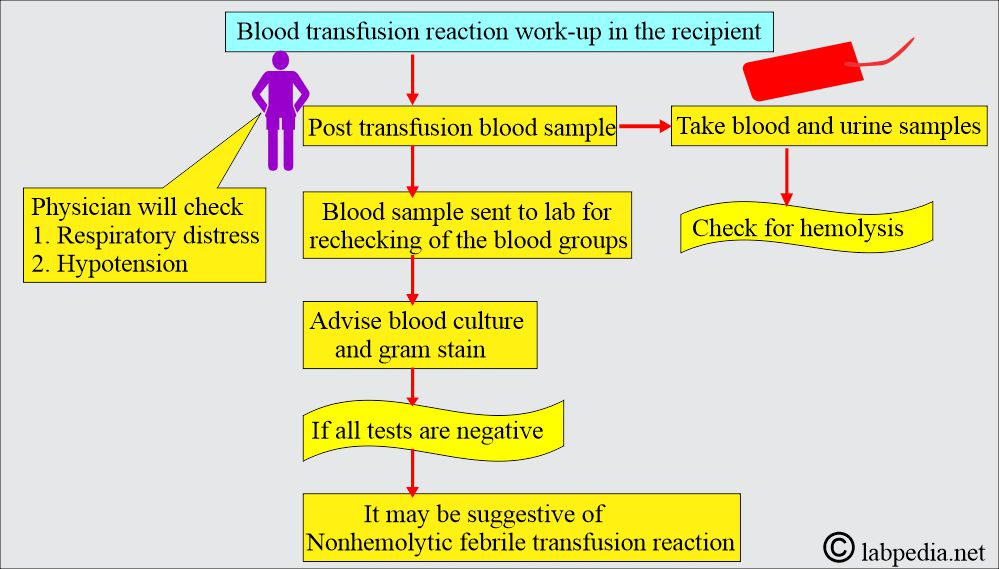
How will you work up the blood transfusion reaction in the recipient?
What are the types of blood transfusion reactions in the recipient?
- Acute blood transfusion reaction in the recipient:
- This reaction occurs within 24 hours.
- Acute reactions are more severe than delayed reactions.
- Acute reactions accompany a fever, nausea, vomiting, hypotension, back pain, and substernal pressure.
- There is hemolysis, and it is generally intravascular.
- Hemoglobin released from the RBCs may give rise to hemoglobinemia (red plasma rather than yellow plasma) and hemoglobinuria (red urine that remains red even after centrifugation).
- There is impaired renal function.
- A delayed blood transfusion reaction occurs in 5 to 7 days. This may vary from 3 to 21 days.
- This occurs in two conditions:
- A primary immune response, accompanied by an increase in antibody concentration, leads to hemolysis.
- When the patient is sensitized by exposure to the alloantigen in a previous blood transfusion or pregnancy.
- Antibodies to Kidd and Rh antigens are responsible.
- Hemolysis is typically extravascular; the only evidence is a decrease in hemoglobin and an increase in bilirubin.
- The patient may have a low fever and feel malaise.
- When no hemolysis is found in a delayed reaction, it is called a serologic reaction rather than hemolytic.
- This occurs in two conditions:
How would you describe a febrile non-hemolytictransfusion reaction in the recipient?
- These are common complications seen in patients with multiple blood transfusions.
- These are related to anti-leucocyte antibodies present in the recipient’s blood.
- These antibodies react with the WBC.
- Another possibility is the presence of cytokines released by the lymphocytes in the donated plasma during storage.
- There is an increase in body temperature of 1°C or more.
- This is accompanied by chills, rigors, and generalized discomfort.
- Some patients may have nausea and vomiting.
- This occurs shortly after the transfusion, usually within 1 to 2 hours.
- Mostly, these reactions are mild and persist for no more than 8 hours.
- Antipyretics and meperidine treat these for rigors.
How would you discuss the Transfusion-related acute lung injury in the recipient?
- This complication occurs during or within 6 hours after transfusion completion.
- The cause of this complication is the presence of anti-leucocyte antibodies in the donor’s plasma.
- The immune complexes are trapped in the pulmonary vasculature, leading to alveolar edema.
- This is characterized by:
- Acute respiratory distress.
- Hypoxia.
- Bilateral infiltrates on chest X-ray.
- There is a fever.
- There is hypotension.
- These patients recover through supportive measures.
- But overall mortality is 5%.
How would you discuss the transfusion-associated graft-versus-host reaction?
- Immunocompetent T-lymphocytes in the cellular components may elicit a reaction.
- These T-lymphocytes can react in the skin and gastrointestinal tract, as well as to cells in the bone marrow.
- This reaction is usually fatal.
- These T-lymphocytes in the blood components can be inactivated by exposure to gamma radiation. This treatment is very effective.
- The patients who are prone to these complications are:
- Hematopoietic stem cell transplantation.
- Hematological Malignancies.
- Infants born with hemolytic disease of the newborn.
- Infants with low birth weight.
- The fetus receives an intrauterine blood transfusion.
How would you discuss the post-transfusion purpura in the recipient?
- This rare complication occurs in patients who lack common platelet antigens.
- These patients develop antibodies from previous blood transfusions or pregnancy.
- These patients develop an anamnestic reaction and become severely thrombocytopenic.
- This reaction usually takes 7 to 10 days.
- The reaction is self-limiting, but it may sometimes be complicated by severe hemorrhage.
- It can be managed by steroids and immunoglobulins.
What is the Refractoriness to platelet transfusion?
- Patients may become sensitized to leucocytes and platelet antigens through previous blood transfusions or pregnancy.
- Platelets are cleared immediately from the circulation when preformed antibodies are present.
- The reaction is against the foreign platelets’ antigen or HLA-class 1 molecule (expressed on the platelets’ membranes).
- Evaluating the platelet count in these patients becomes challenging.
What is the reaction to plasma components?
- 1% to 3% of patients may have an allergic reaction to the blood products.
- This is the host’s reaction to the donor’s plasma proteins.
- The majority of these reactions show:
- Hives.
- Pruritis.
- Erythema.
- Steroids or antihistamines can treat it.
- Serious reactions are less frequent, like:
- Bronchospasm.
- Laryngeal edema.
- GIT symptoms like nausea, vomiting, abdominal cramps, and diarrhea.
- Hypotension due to type 1 anaphylaxis.
- Patients with IgA deficiency need components from the IgA-deficient donor, or can use their own components.
What are the etiological signs and symptoms of blood transfusion reactions in the recipient?
- Circulatory overload shows:
- Shortness of breath.
- Direct Coombs’ test is negative.
- There is no fever or chills.
- Acute hemolytic transfusion reaction shows:
- Fever and chills.
- There are fever and chills.
- Hemoglobin is low.
- There is hemoglobinuria.
- There may be hypotension and shock.
- Direct Coombs’ test is positive.
- Febrile non-hemolytic transfusion reaction:
- There are fever and chills.
- There are nausea and vomiting.
- There may be shortness of breath.
- Direct Coombs’ test is negative.
- Transfusion-related acute lung injury:
- There are fever and chills.
- There is shortness of breath.
- There are hypotension and shock.
- Direct Coombs’ test is negative.
- Bacterial contamination of the blood:
- There are fever and chills.
- Hemoglobin is low.
- There may be hemoglobinuria.
- There are hypotension and shock.
- Direct Coombs’ test is negative.
What are the non-immunologic reactions in the recipient?
- Hypothermia:
- It usually occurs when cold blood is transfused.
- There may be minor discomfort.
- This may also occur in a massive blood transfusion, where the blood is stored at 1°C to 10 °C.
- Hemostasis is affected when the circulating blood is below 37 °C.
- In extreme cases, cardiac dysrhythmias may occur and cause cardiac arrest.
- The use of a high-throughput blood warmer is needed.
- Transfusion-associated circulatory overload:
- Volume overload is a common and often overlooked complication of blood transfusion.
- The following group of patients is at risk:
- Patient with congestive heart failure.
- Patient with renal failure.
- Very young and old patients.
- These patients have signs and symptoms:
- There is dyspnea.
- There is orthopnea.
- Cough and chest pain.
- During or soon after the transfusion, there is hypoxia, rales, tachycardia, or hypertension.
- The patient can be treated with supplemental oxygen and diuresis.
- If another blood transfusion is required, administer the blood slowly and consider adding diuretics.
What are the Chemical complications in the recipient?
- Iron-overload:
- Each unit of blood contains around 200 mg of iron.
- Repeated blood transfusion leads to the deposition of iron in various tissues.
- In case a patient has received around 100 bottles or more of blood transfusions, then the patient may have complications like:
- Cardiac Arrhythmias.
- Pancreatic failure and bronze diabetes.
- Liver function abnormality.
- Iron overload can be treated by chelating agents such as desferrioxamine or deferasirox.
- This should be started in the early stage before the deposition of iron.
- Potassium – Toxicity:
- Potassium leaks out of the RBCs during storage due to a decrease in the ATP level.
- ATPase-dependent Na+/K+ pump activity decreases.
- Each blood RBC unit contains as much as 6 mmol of extracellular K+ when an outdated sample is used.
- Extra K+ may lead to cardiac arrhythmias.
- Washing the RBCs may remove extra K+.
- Citrate toxicity:
- Citrate is used as an anticoagulant.
- Citrate is present in the plasma.
- Citrate is metabolized by every nucleated cell of the body.
- In the case of massive blood transfusion, the rapid influx of citrate may not be metabolized by the body, leading to the accumulation of citrate in the patient’s plasma.
- The patient can receive up to one unit of fresh-frozen plasma every 6 minutes without evidence of citrate toxicity.
- Patients with liver diseases metabolize citrate slowly and are prone to develop citrate toxicity.
- The citrate chelates the calcium, causing the ionized calcium level to drop and leading to:
- Peri-oral tingling.
- Extremity paresthesia.
- There may be severe hypocalcemia (ionized calcium) leading to cardiac dysrhythmias.
- Depletion of 2, 3 Diphosphoglycerate:
- When blood is stored for a longer period, there is a decrease in the intracellular 2,3-diphosphoglycerate.
- This will result in a shift to the left of the oxygen-hemoglobin dissociation curve.
- When the stored unit is transfused, it restores the 2,3-DPG over 24 to 48 hours.
- It is recommended that transfused blood to the neonates should be kept for less than a week.
- Complications are found in the neonates if older blood units are transfused.
- In the case of stored blood deficient in 2,3-DGP, it impairs oxygen delivery, particularly in neonates.
What are the infectious complications in the recipient?
- Viral infections. There is a risk of infection by:
- Hepatitis B virus.
- Hepatitis C virus.
- HIV
- Because donor education and screening have reduced the incidence.
- The current significant pathogens, such as bacterial blood contamination, are a problem even in developed countries like the USA.
- The bacteria that are more frequently found are:
- Yersinia enterocolitis.
- Pseudomonas.
- Enterobacter spp.
- Serratia sp.
- Platelet units are reported to have an infection by:
- Gram-positive bacteria, cocci-like:
- Streptococcus.
- S.Epidermidis.
- Staphylococcus.
- Gram-negative bacteria reported are:
- Klebsiella spp.
- Serratia spp.
- Salmonella spp.
- Enterobacter spp.
- Gram-positive bacteria, cocci-like:
- The source of the infection may be contamination from the skin. The skin commensals are thought to be picked up and introduced into the bloodstream through venepuncture during blood donation.
- Cytomegalovirus (CMV) can be transmitted through the transfer of blood components containing leukocytes, such as packed red blood cells (RBCs) and platelets.
- It can produce systemic infection by CMV in immune-compromised patients who are seronegative.
- The following groups are more prone to getting CMV infection:
- Premature infants with low birth weight (<1200 g).
- CMV-negative pregnant women receiving an intrauterine transfusion.
- CMV-negative, HIV-infected patients.
- CMV-negative recipient of or candidate for hematopoietic organ transplantation.
- To reduce the risk of CMV, recommend screening donors.
- Remove the leukocytes that contain latent CMV by filtration with leukocyte reduction filters.
How will you summarize blood transfusion-related reactions?
What is the risk of the various viruses’ transmission from the blood components?
| Viruses | The estimated risk of transmission from the blood components |
| HIV | 1:493,000 |
| HTLV | 1:641,000 |
| HBV | 1:63,000 |
| HCV | 1:103,000 |
| HAV | Rarely reported in some cases |
| West Nile virus | It may spread through the blood |
| Transmission during pregnancy: | |
| HBV, HCV, HIV, CMV, HPV-B19 | Rates vary from country to country |
| Dengue fever |
In tropical and subtropical countries |
| Zika virus | May be transmitted to the fetus |
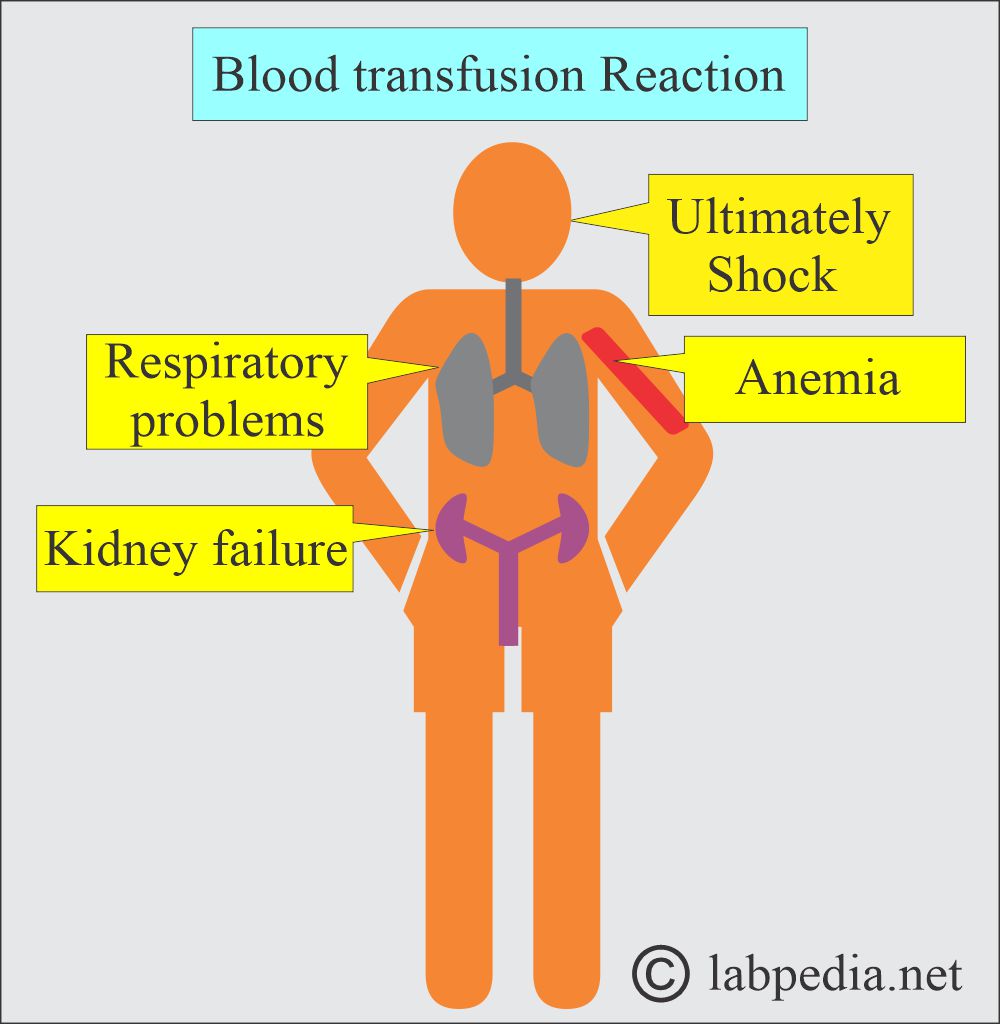
What are the complications of blood transfusion reactions?
- Anemia
- Kidney failure.
- Respiratory problems.
- Ultimately shock.
What are the Common Causes of blood transfusion reactions?
- The most common cause is faulty matching.
- Improper identification or labeling of the donor and recipient may cause a transfusion reaction.
What are the problems seen in the ABO Blood Typing?
- There may be abnormal, weak agglutination. Normally, there are 3+ to 4+ agglutinations.
- Mixed-field agglutination occurs when some of the patient’s RBCs agglutinate, while others do not.
- Rouleaux formation by RBCs should be differentiated from agglutination. In comparison, Rouleaux formation refers to the stacking of red blood cells (RBCs).
- Clumping due to blood micro-clots in the procedure.
- No agglutination when all cells and serum ABO is nonreactive.
What are the common mistakes in the ABO blood group typing?
- If there are incorrect blood reagents,
- If there is contamination of the reagents.
- If incorrect or outdated reagents are used.
- If you miss adding the reagents, the patient’s serum, or the patient’s cells.
- Fail to follow the manufacturer’s instructions.
- Over-centrifugation can lead to false-negative results.
- If there is an incorrect incubation temperature.
- If there is an improper ratio of the antisera or RBCs.
- The clerical mistake of typing the result.
- If there is contaminated glassware or supplies.
- If there is a failure to identify the signs of hemolysis.
- If there is weak agglutination.
Summary of the adverse effects of blood and blood products reactions:
What is the recipient’s reaction to donor antigens (donor RBCs)?
- The recipient may have a reaction to the donor RBCs’ antigens, e.g.:
- Anaphylactic reaction (type 1 hypersensitivity reaction).
- Hemolytic reactions.
- Allergic reactions.
- Nonhemolytic febrile reactions.
- Cytopenic reactions.
- Tissue-immunologic reaction
- What are the antigens that lead to reactions?
- Blood group ABO system.
- Blood group Rh system.
- HLA antigen (histocompatibility leukocyte antigen).
- Minor blood groups.
- Platelet antigens.
- What are the possible Infectious organisms?
- Hepatitis B virus.
- Hepatitis C virus.
- HIV infection.
- Cytomegalovirus (CMV).
- Epstein-Barr virus.
- Malarial infection.
- Syphilis.
- What are the side effects of the blood preservatives?
- Overload due to citrate.
- Depletion of coagulation factors.
- Hyperkalemia.
- Donor medications.
- Depletion of platelets.
- The temperature of the transfused blood.
- Tissue-organ immunologic reaction:
- Graft-vs-host disease.
How will you treat blood transfusion reactions?
- This is just like the type I Hypersensitivity reaction.
- Give epinephrine subcutaneously, 0.3 to 0.5 mL of a 1:1000 solution.
- Epinephrine can be repeated in 20 to 30 minutes.
- Start O2 therapy.
- Administer Diphenhydramine 50 mg IM; if needed, administer IV.
- Start I/V saline to maintain blood volume and pressure.
- If hypotension persists, administer Epinephrine IV 10 mL of 1:1000 solution.
- For bronchospasm, administer Aminophylline 6 mg/Kg body weight initially, followed by 0.5 to 1 mg/Kg body weight.
- If there is severe respiratory distress, then intubate the patient.
- In cases of severe laryngeal edema, a tracheostomy may be performed.
- In a prolonged reaction, consider Hydrocortisone up to 500 mg I/V every 6 hours.
Questions and answers:
Question 1: What is the end result of blood transfusion reaction in the recipient?
Patient due to blood transfusion may go into shock and death”]
Question 2: Is there a possibility of iron overload in repeated blood transfusion?