Bleeding Time (BT)
Bleeding Time (BT)
What sample is needed for Bleeding Time (BT)?
- This test is performed on the patient while they are in the lab.
- No preparation is necessary.
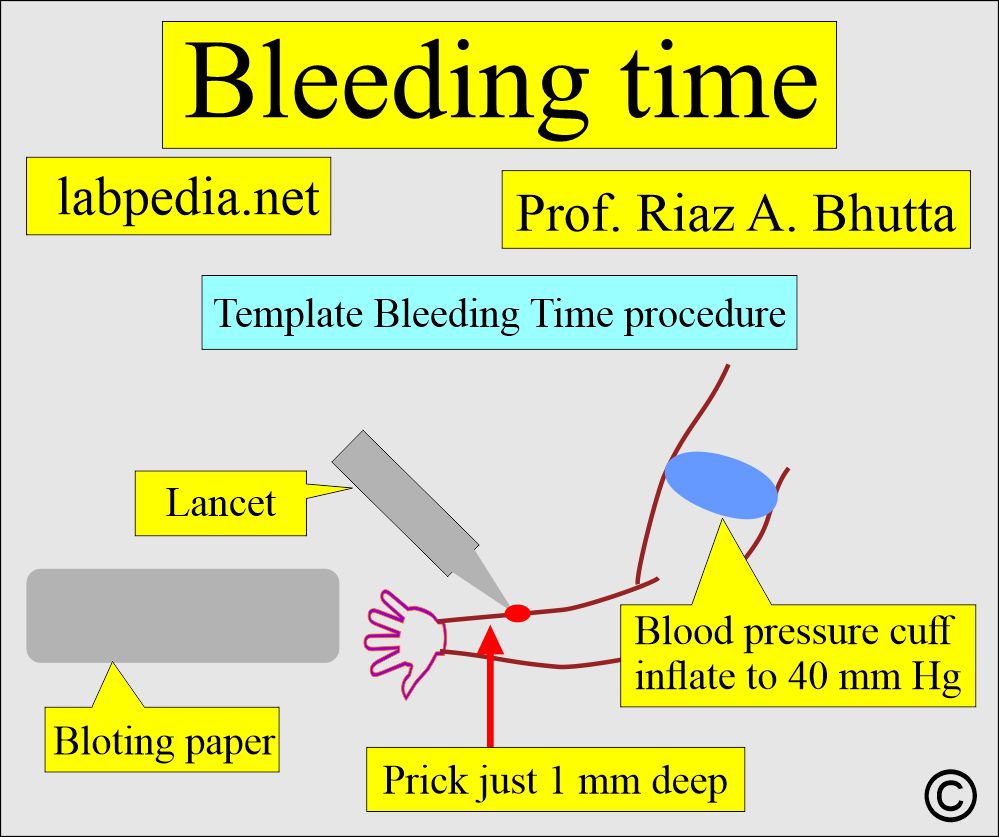
- The template (Meilke) method is the most common and considered the most accurate.
- This template is a modified version of the Ivy method.
- The template method gives 1 mm deep incisions.
- A small, disposable, spring-driven lancet produces a 5 mm long and 1 mm deep incision, resulting in minimal pain and no scar formation.
- Ivy and Duke’s methods were used in old times.
What are the precautions for bleeding time (BT)?
- This test should be avoided in a patient with a low platelet count.
- A patient with aspirin may have a false positive (raised value).
- Avoid in patients with keloid formation or senile skin changes.
- Avoid in patients who have undergone mastectomy or axillary lymph node dissection.
- Avoid uncooperative patients.
- Extreme body temperature gives false results.
- High body temperature prolonged the result.
- Low body temperature lowers the result.
- Avoid and take the history of drugs that may prolong the result, like patients on anticoagulant therapy, use of salicylates, antibiotics, streptokinase, nonsteroidal anti-inflammatory drugs, and warfarin.
What are the indications for Bleeding Time (BT)?
- Bleeding time (BT) is the best test to evaluate the platelets’ function and structural abnormalities.
- This test is done to evaluate vascular and platelet factors.
- Bleeding time gives a better idea of platelet function, such as the platelet count.
- This may be done preoperatively to rule out the possibility of bleeding, for example, in patients undergoing tonsillectomy.
- But this may not be a routine presurgical procedure.
- This test is used to evaluate the stability of the patient’s hemostatic mechanism.
- A bleeding test may be done to detect the presence of various coagulation disorders.
- This may be advised to monitor the treatment of active hemorrhage in patients with prolonged bleeding time due to von Willebrand disease, severe anemia, and congenital platelet functional abnormalities.
- Bleeding time (BT) is the best test for screening uremic patients.
- It is advised in a history of excessive bleeding and normal bleeding time (BT) before:
- Extraction of the tooth.
- Circumcision.
- Childbirth.
- Tonsillectomy.
- Summary of bleeding time indications:
- Platelet function disorders.
- Vascular defects.
- Effects of drugs.
- Von Willebrand disease.
What are the advantages of Bleeding Time (BT)?
- This test is used to differentiate Von Willebrand’s disease from mild hemophilia.
- This test is useful as a part of the workup for coagulation disorders in patients with H/O excessive bleeding during dental extraction, tonsillectomy, circumcision, and childbirth, even with a normal platelet count.
- The bleeding time (BT) is used to detect any abnormalities in platelet number or function.
What are the disadvantages of Bleeding Time (BT)?
- No use in doing bleeding time (BT) in case of decreased platelets (<100,000/cmm), as bleeding time (BT) is usually prolonged.
- Normal bleeding time (BT) does not rule out significant platelet abnormalities in cases of clinical suspicion. In such cases, a platelets aggregation test should be performed, and check the fibrinogen level.
- This test is unable to predict excessive surgical bleeding.
- Bleeding time is a crude and not a good screening test for bleeding during surgery.
- The bleeding test will neither predict the likelihood of bleeding nor the possibility of not bleeding.
- The bleeding time prick is 9 mm long and 1 mm deep, which may lead to scar formation.
- This test is not recommended to predict bleeding in myeloproliferative disorders and neonates receiving nonsteroidal anti-inflammatory drugs.
- Prolonged bleeding time may not necessarily lead to prolonged bleeding.
- Not recommended for predicting bleeding in case of myeloproliferative diseases or neonates receiving NSAIDs (Non-steroidal anti-inflammatory drugs).
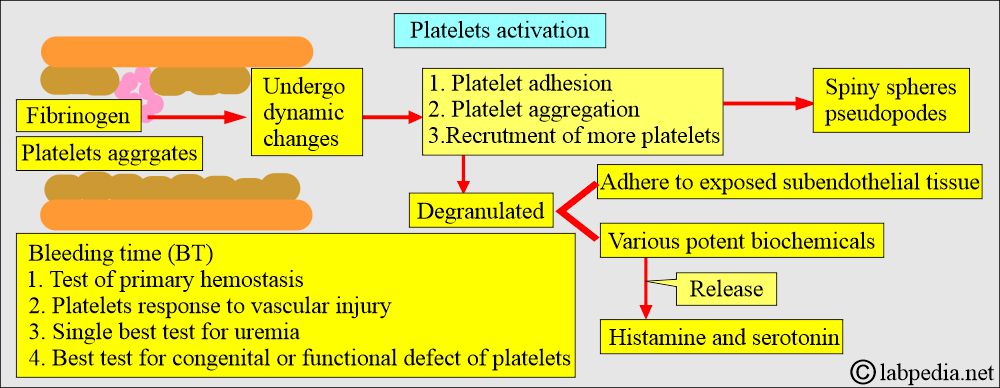
How will you define Bleeding Time (BT)?
- Bleeding time is the functional test of primary hemostasis.
- This test diagnoses bleeding problems related to the abnormalities of:
- Platelet functions. Platelets respond to vascular injury.
- Vascular response to injury.
- Blood vessel elasticity also influences the bleeding time.
- The ability of the blood vessels to constrict.
- Bleeding time is the best single screening test for acquired causes, like uremia or congenital functional or structural disorders of platelets.
- Bleeding time depends upon:
- Platelet functions.
- Platelet count.
- Vascular ability to stop bleeding.
What are the important facts about Bleeding time (BT)?
- In the case of platelets 100,000/cmm, the bleeding time is usually normal, but when it is <100,000/cmm, the bleeding time is prolonged, and there may be a correlation between the count and severity of thrombocytopenia.
- It measures the length of time bleeding continues after the standardized incision is made in the skin.
- The bleeding time is usually abnormal in congenital defects, such as Glanzmann’s thrombasthenia.
- Bleeding time is also abnormal in uremia, and the myeloproliferative syndrome is an acquired functional abnormality.
- 50% of uremic patients show thrombocytopenia.
- Bleeding in uremia is not usually seen unless the bleeding time is elevated, but some studies don’t agree with this hypothesis.
- Uremic bleeding can be treated by fresh frozen plasma, cryoprecipitate, or desmopressin (DDAVP = 1-deamino-8-arginine-vasopressin).
- Some drugs, like aspirin, also interfere with platelet functions and prolong the bleeding time.
- After a single dose of aspirin, prolonged bleeding time is observed even within 2 hours, with maximum effect typically occurring after about 24 hours.
- Aspirin permanently affects the function of platelets in circulation.
- Platelets’ lifespan is 7 to 10 days, and approximately 10% of the platelets are replaced daily.
- After stopping the aspirin, it takes 2 to 3 days, and the range is 1 to 8 days to produce a sufficient number of unaffected platelets, bringing the elevated bleeding time back into the normal range.
- Bleeding time may be abnormal in cases of capillary fragility.
- Bleeding time is typically normal in cases of hemophilia and vitamin K or fibrinogen deficiencies, but it is abnormal in severe cases.
- Generally, if the bleeding time exceeds 1.5 times the normal limit, the risk of excessive bleeding during surgery increases.
- Bleeding time is basically a screening test for:
- Disorders of platelet function and numbers.
- The integrity of the vascular wall.
What is the value of the effect of various blood coagulation factors on bleeding?
| Coagulation test | Abnormality of platelets | Abnormality in the intrinsic pathway | Abnormality of prothrombin | Abnormality of fibrinogen or fibrin |
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
What is the importance of platelets?
Platelets:
- Platelet abnormalities are divided into two groups:
- Quantitative when there is an abnormal platelet count.
- Qualitative, where the platelets’ functions are abnormal.
How will you predict bleeding due to the function of platelets?
- How to predict whether a patient may bleed because of platelet abnormalities:
- If there is a history of aspirin intake or other drugs, it will give rise to thrombocytopenia.
- History of oozing or blood loss due to minor oral or dental surgery, during menses, or easy bruising.
- In case of a low platelet count.
What are the Quantitative platelet abnormalities?
| Diseases leading to thrombocytopenia | Causative diseases |
|
|
|
|
|
Pooling:
Dilution:
|
|
Coagulative consumption:
Immune destruction:
Isolated consumption:
|
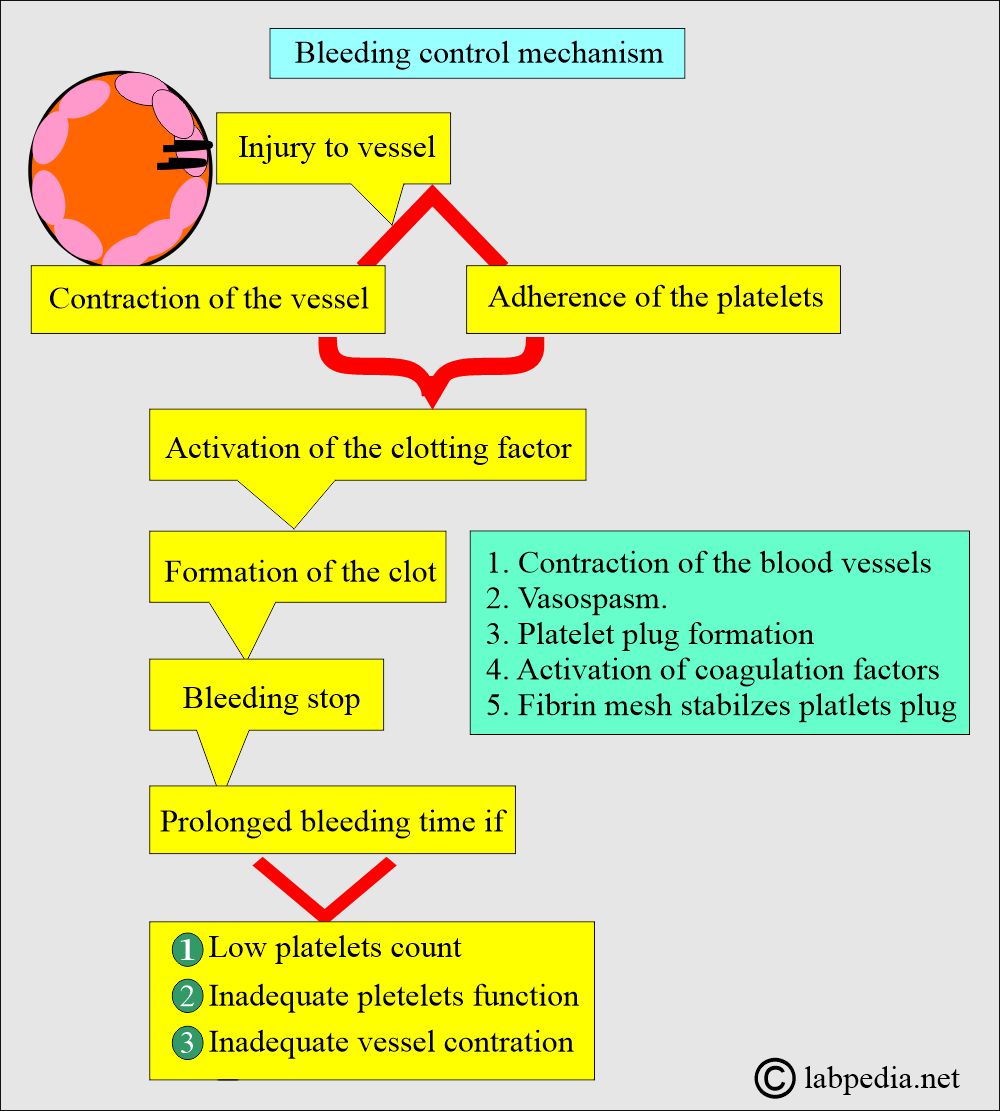
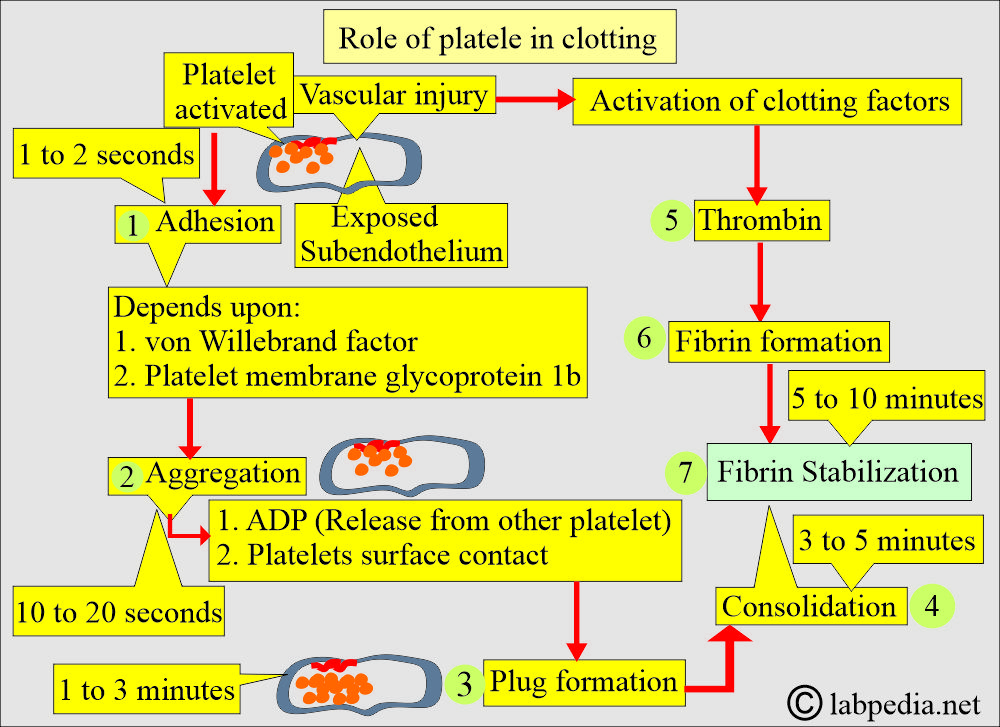
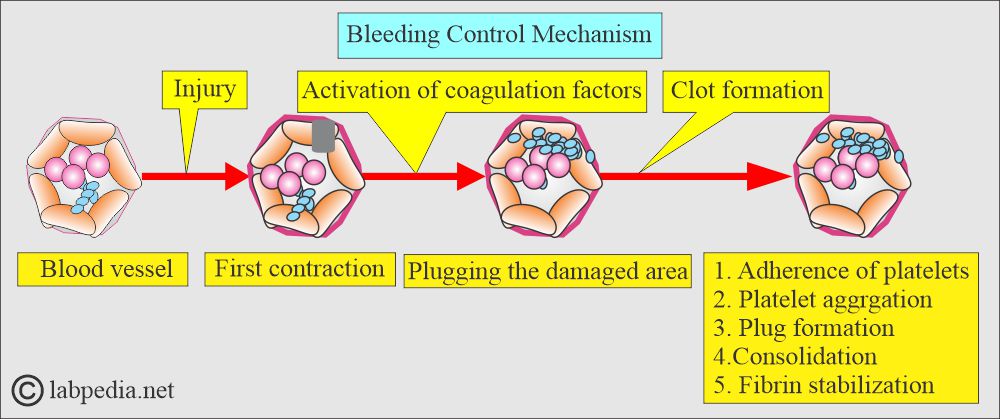
What are the stages in the blood coagulation phenomenon?
- First hemostatic response:
- For vascular injury, the initial hemostatic response involves the contraction of blood vessels.
- The next phase is the adherence of platelets to the injured vessel and the formation of plugs in the damaged area.
- Vasospasm:
- Vasoconstriction (vasospasm). This is controlled by local, humoral, and neuronal factors.
- Initially, there is vasoconstriction, followed by vasodilation, which facilitates the influx of inflammatory cells.
- Formation of platelet plug:
- There are granules discharged from the platelets.
- The platelets aggregate into clumps or plugs.
- Then release chemical mediators.
- Platelets are attracted to the site of endothelial injury within 15 to 20 seconds.
- Platelets make plug formation.
- Blood coagulation factors:
- These coagulation factors are activated, helping to facilitate the coagulation process.
- Vasculature: There is vasoconstriction (vasospasm).
What are the functions of the platelets?
- The platelet membrane is composed of glycoproteins that determine the interaction between platelets and their external environment.
- The binding of fibrinogen to the platelets leads to platelet aggregation.
- Adherent platelets produce histamine, and serotonin will lead to vasoconstriction.
What are the steps in the bleeding control mechanism?
- Activation of coagulation factors.
- Formation of a clot.
- Clot retraction.
- Clot dissolution (fibrinolysis).
- Failure of any of the above factors leads to prolonged bleeding.
- If the blood vessels have increased fragility, it will also lead to a prolonged bleeding time, as seen in old age or a patient with a capillary defect.
- The coagulation system does not affect blood vessel constriction and platelet adherence (Intrinsic and extrinsic pathways).
- This test is a sensitive measure of platelet function and the elasticity of blood vessels.
What is the normal platelet count?
- Normal platelet count is 140,000 to 340,000/cmm.
- Platelets around 20,000/cmm may have a major episode of hemorrhage.
- It is a crude bio-assay but has become a reliable and sensitive platelet function test by careful standardization.
What are the critical values?
- Platelet counts less than 50,000/cmm may lead to prolonged bleeding times.
- Platelets may be roughly estimated from the peripheral smear, where you will find 10 to 20 platelets /high-power field or 1 platelet/20 RBCs in the normal range.
- A bleeding time of more than 10 minutes carries a risk of excessive bleeding; when it is 15 to 20 minutes, the risk of bleeding may increase.
What are the normal values of bleeding time (BT)?
- Bleeding time normal: 2 to 7 minutes
- Borderline: 7 to 11 minutes.
- Abnormal value: 10 to 15 minutes
- Duke ear lobe method = 1 to 3 minutes
Source 2
- Ivy method = 1 to 9 minutes
- Prolonged bleeding time may be repeated to confirm it. Because if sometimes the large-caliber blood vessel is punctured, then the bleeding time will be prolonged.
Another source
- Adult, elderly, and pregnant = Template method = 2.0 to 8.5 minutes
-
- = Ivy method = 1 to 10 minutes
- = Duke method = 1 to 3 method
-
- Newborn = Ivy method = 1 to 5 minutes
- Child = Ivy method = 1 to 6 minutes
What are the methods for measuring bleeding time?
How will you describe the IVY method?
- It is the most common method where the lancet is used, ensuring a precise surgical incision with a depth of 1 mm. This will give reproducible results.
- The Bleeding Time is determined by making a superficial skin incision and timing the duration of blood flow from the wounded area until it stops.
How will you describe the Template method?
- A puncture of the forearm after having pressure in the upper arm at 40 mm Hg by a blood pressure instrument.
- Clean the volar surface of the forearm.
- Make an incision using the template, up to a depth of 1 mm. If possible, give two pricks.
- Avoid any visible vein.
- Now blot the blood till it stops.
- Bleeding time is usually normal in coagulation disorders.
- Bleeding time has limited precision, accuracy, and reproducibility.
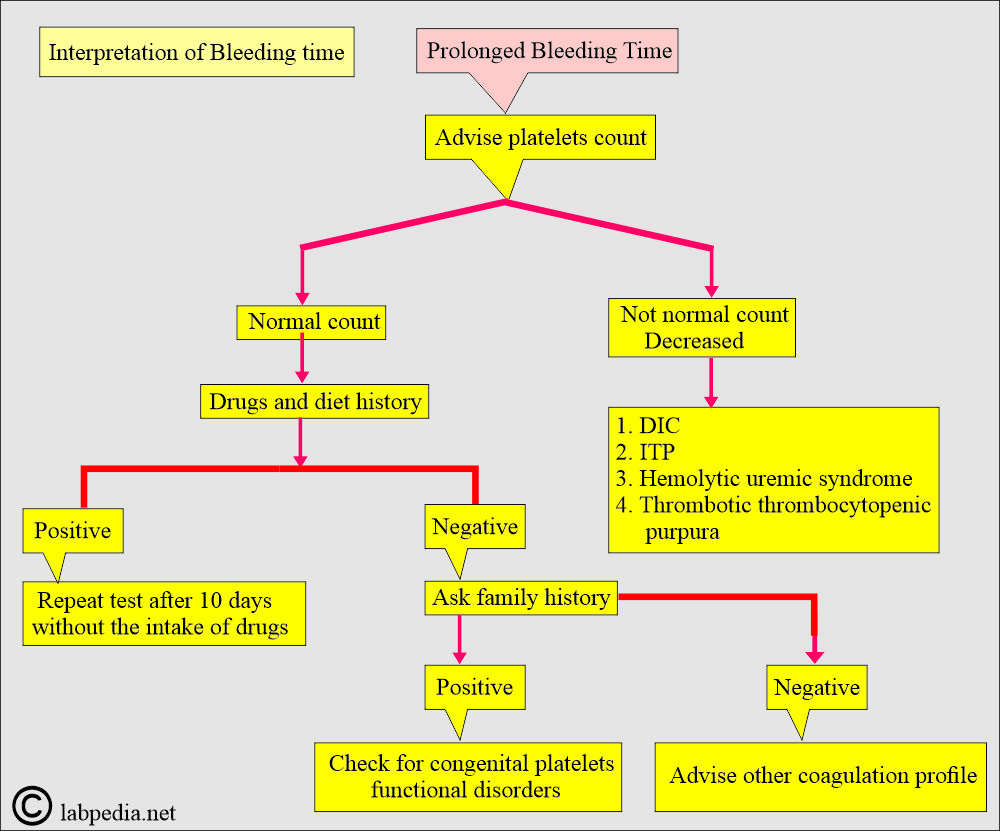
What are the causes of longer-than-normal bleeding time?
- Blood vessel defect.
- Platelet count may be decreased, or there may be a defect in their function.
- Thrombocytopenia. The count is <100,000/cmm and usually <80,000/cmm before bleeding becomes abnormal.
- Bleeding time is always abnormal when the platelet count is <60,000/cmm.
- Platelet count <80,000/cmm = BT is ∼10 minutes.
- Platelet count <40,000/cmm = BT is ∼20 minutes.
- Platelet count <10,000/cmm = BT is >30 minutes.
- Disseminated intravascular coagulation (DIC), where the platelets are consumed.
- Acute Leukemia.
- Coagulation factor deficiencies, such as Factor I, II, V, VIII, IX, and XI, may show some increase.
- Hodgkin’s disease.
- Severe hepatic disease.
- Hemolytic disease of the newborn.
- Patients with uremia have a decrease and dysfunction of platelets.
- Patients with anti-inflammatory drugs like aspirin and indomethacin.
- In von Willebrand’s disease, the bleeding time is variable. BT is increased out of proportion to platelets, suggesting von Willebrand disease or a platelet functional defect.
When will you see normal bleeding time (BT)?
- Hemophilia.
- Severe hereditary hypofibrinogenemia.
- Severe hereditary hypoprothrombinemia.
- What are the Critical values of the bleeding time?
- The bleeding time is usually greater than 15 minutes.
Questions and answers:
Question 1: Any relation of bleeding time (BT) with platelets count?
Question 2: What is the critical value of platelets?

So useful information …. Thank you so much 🥰❤️
Thanks.