Antidiuretic Hormone (ADH, Vasopressin, Arginine Vasopressin), Diabetes Insipidus
Antidiuretic Hormone (ADH)
What sample is needed for Antidiuretic Hormone (ADH)?
- This test is performed on a prechilled venous blood sample (in a tube).
- Plasma with EDTA is needed.
- Take the blood when a patient is in a sitting position and calm.
- Put the sample on ice.
- Or collect the sample in prechilled vials.
- Separate plasma immediately in the refrigerated centrifuge and freeze at -20 °C.
What are the Indications for Antidiuretic Hormone (ADH)?
- ADH is done in patients with diabetes insipidus.
- Advised a patient with polyuria or polydipsia.
- This is also advised in hyponatremia.
- For the diagnosis of ectopic ADH production.
- This is advised in SIADH (syndrome of inappropriate antidiuretic hormone secretion).
- This is also advised in psychogenic water intoxication.
What are the precautions for Antidiuretic Hormone (ADH)?
- Avoid glass syringes or collection tubes, which cause degradation of the ADH.
- Avoid dehydration, hypovolemia, and stress, which may lead to increased ADH levels.
- Avoid overhydration and hypervolemia, which may decrease the ADH level.
- The use of a glass syringe or collection tube causes degradation of the ADH.
- Drugs like acetaminophen, cholinergic drugs, barbiturates, nicotine, estrogen, oral hypoglycemic agents, diuretics (thiazide), narcotics, and tricyclic antidepressants will increase ADH.
- Drugs like alcohol, morphine antagonists, Dilantin, and beta-adrenergic agents will decrease the ADH level.
- The recent history of radioisotopes gives the wrong result.
How will you define Antidiuretic Hormone (ADH)?
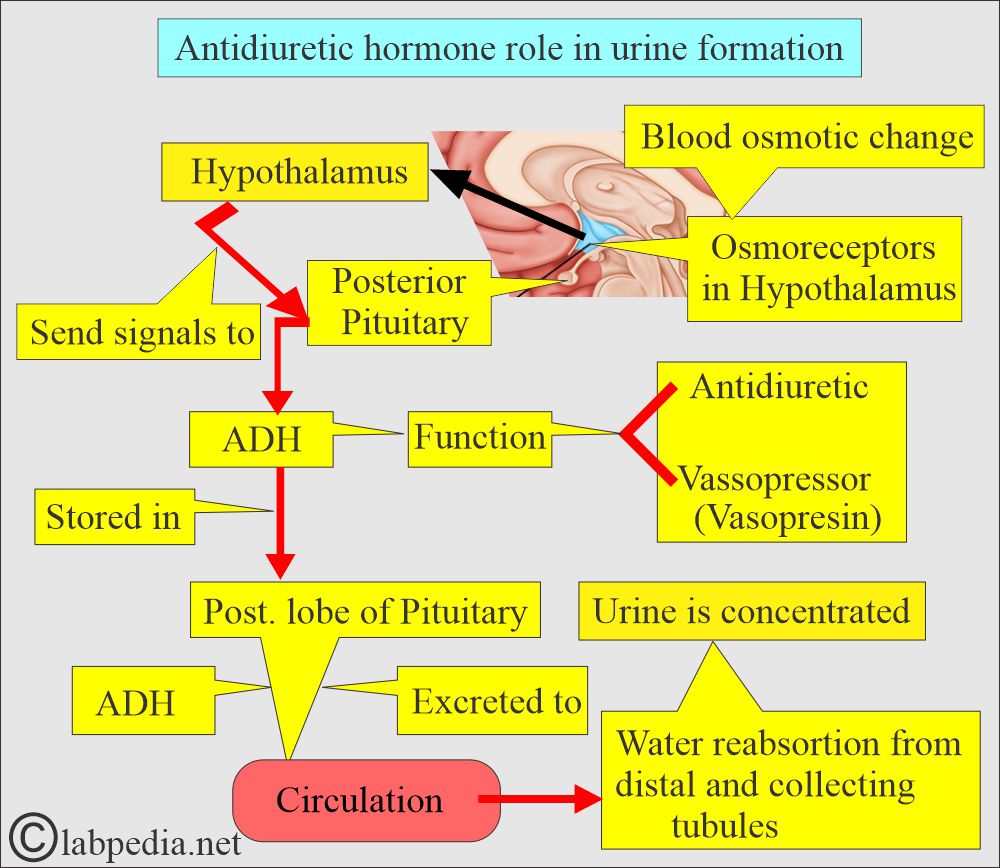
- ADH, also called Vasopressin (or arginine Vasopressin), is produced under the center’s influence in the anterior hypothalamus and stored in the posterior pituitary gland. It is excreted into the blood circulation.
- ADH is considered one of the plasma volume regulators due to its ability to concentrate the urine via its action on the renal distal and collecting tubules by water reabsorption.
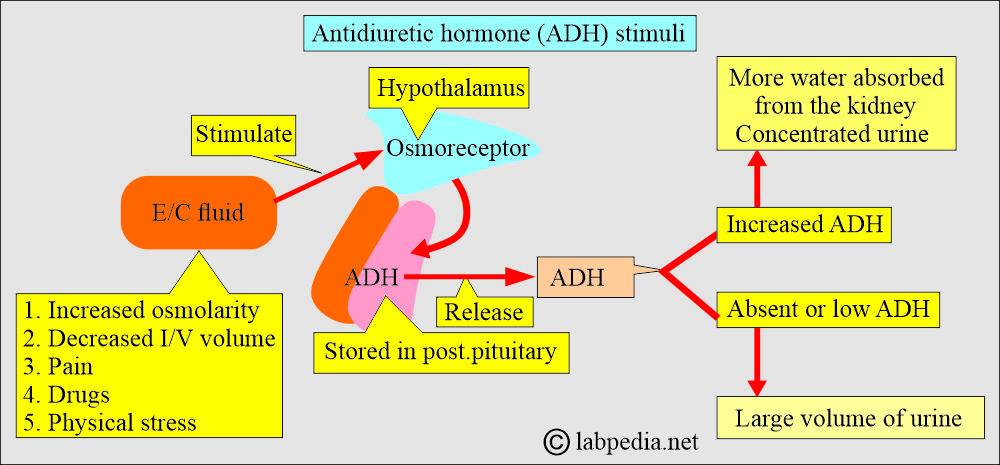
- The osmolarity of the extracellular fluid controls ADH release.
- Increased osmolarity stimulates the osmoreceptors in the hypothalamus, which stimulates the release of ADH.
What are the major functions of Antidiuretic hormone (ADH)?
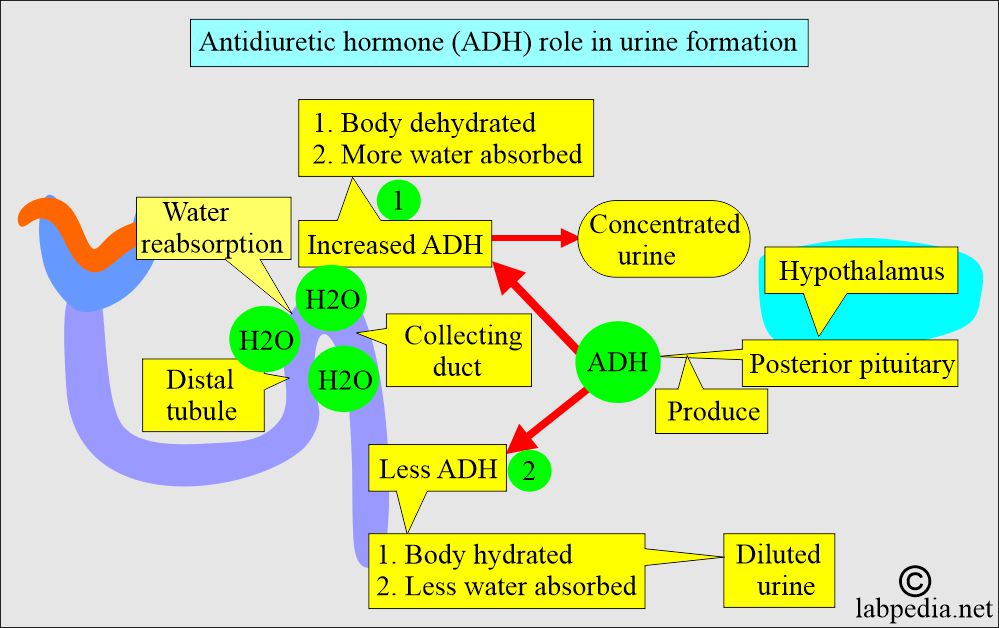
- When ADH activity is present, then a small volume of concentrated urine is excreted.
- When ADH is absent, then a large volume of dilute urine is excreted.
- ADH maintains water homeostasis.
- The kidneys do water reabsorption, and urine is concentrated.
- ADH in sufficient quantity induces generalized vasoconstriction that leads to an increase in arterial blood pressure.
- ADH releases more water reabsorbed from the distal and collecting tubules, increasing water reabsorption and leading to concentrated urine and more water in the blood circulation.
- ADH decreased level, and less water was reabsorbed (water was allowed to be excreted), leading to dilute urine and hemoconcentration.
What are the stimulants for the release of antidiuretic hormone (ADH)?
- The increase in serum osmolality.
- Blood osmotic changes, like concentration and dilution, act on osmoreceptors in the hypothalamus.
- The decrease in intravascular blood volume (blood volume changes).
- Higher secretion occurs at night, with erect posture, and with exercise.
- Physical Stress, surgery, and even anxiety.
- Neural influences like pain.
- Certain drugs, like morphine and alcohol.
What are the syndromes associated with ADH?
- Diabetes inspidus.
- Inappropriate ADH syndrome.
Syndrome of inappropriate ADH secretion(SIADH):
- It is associated with high serum ADH levels.
- Water retention is due to the secretion of ADH when it is not secreted in normal conditions.
- The Criteria for SIADH are the secretion of ADH despite hemodilution, decreased serum osmolality, or both.
- Mostly, these patients have no edema.
How will you diagnose SIADH and its characteristic features?
- Hyponatremia.
- Continued renal excretion of the Na+ despite the hyponatremia.
- Serum hypoosmolarity.
- Urine osmolality shows a significant degree of concentration instead of what one would expect to have dilute urine.
- No evidence of blood volume depletion.
- There is a normal renal and adrenal function that will differentiate from other causes.
- These criteria will demonstrate that ADH is secreted despite the hemodilution, decreased serum osmolality, or both.
- Most of these patients do not have edema because interstitial fluid expansion is usually moderate in degree.
- The water load test means ADH suppression differentiates the SIADH from the other causes of hyponatremia and/or edematous conditions.
- Measure urine and serum osmolarity.
- Patients with SIADH secrete very little or no water.
- Urine osmolarity will never be <100 mmol/kg
- The urine/serum ratio is >100.
- Measure urine and serum osmolarity.
- The treatment of choice for SIADH is the restriction of fluid intake, which may provide some evidence of this syndrome.
Paraneoplastic syndrome:
- It is seen in ectopic production of the ADH, like carcinoma of the lung, thymus, lymphoma, carcinoma of the pancreas, leukemia, urinary system, and intestine.
- This condition may also be seen in pulmonary tuberculosis and pneumonia.
- Other conditions are CNS tumors, infection, and trauma.
Diabetes Insipidus:
How will you define diabetes inspidus?
- This is a syndrome characterized by hypotonic polyuria.
- Diabetes insipidus is a chronic condition accompanied by a large volume of hypotonic urine caused by an inability to concentrate the urine due to a lack of ADH secretion or production.
What are the signs and symptoms of Diabetes Inspidus?
- Diabetes insipidus is characterized by:
- Abnormally increased urine output.
- Increased fluid intake.
- Often accompanied by thirst.
- This is because of the absence of the ADH effect, either due to:
- Impaired or failed secretion from the pituitary gland (neurogenic).
- Or no response by the end organ or kidneys (nephrogenic).
- This may be seen in a person with psychogenic polydipsia, or compulsive water intake, which may present as diabetes insipidus.
- This is not related to diabetes mellitus, in which polyuria is hypertonic due to the overexcretion of glucose in the urine.
How will you classify diabetes insipidus?
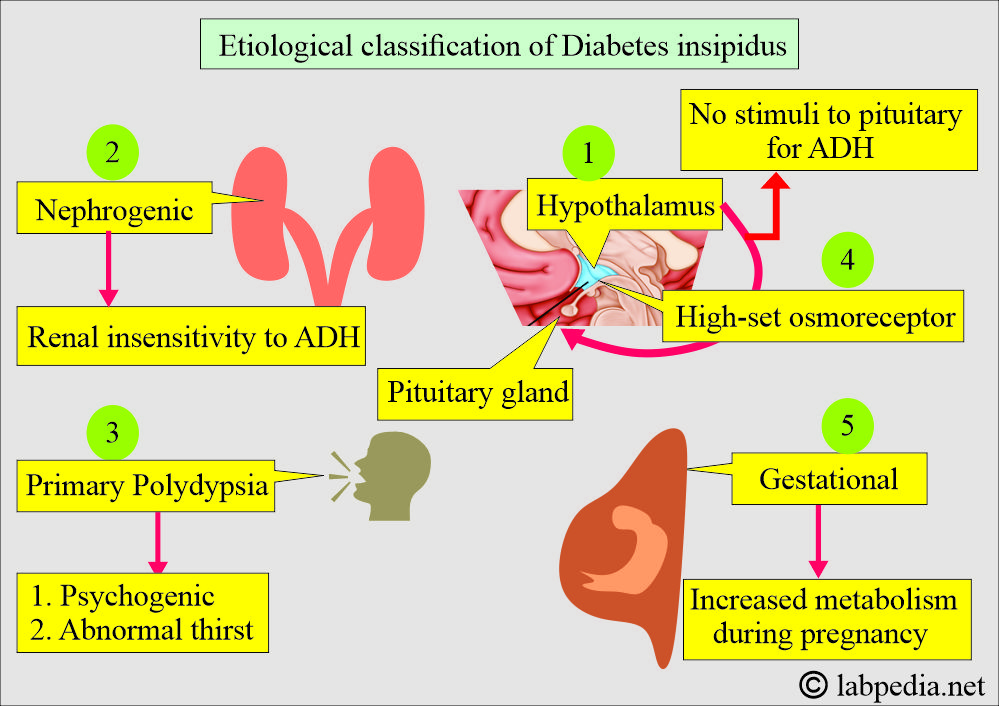
- The possible etiological classification is as follows:
- Neurogenic, where the hypothalamus cannot produce ADH from the pituitary gland.
- The renal is where the end-organ’s inability to respond normally to ADH.
- Primary polydipsia may be psychogenic or an abnormal thirst mechanism.
- Temporary overpowering of the vasopressin system. A large quantity of water is ingested, sometimes referred to as primary diabetes insipidus.
- Gestational Diabetes inspidus, where there is increased metabolism of ADH.
- High-set osmoreceptors.
- ADH is inadequate OR
- When the kidneys are not responsive to ADH stimulation.
- The patient excretes a large volume of water in the urine.
- There is hemoconcentration, and patients feel thirsty.
What is another Classification of Diabetes Insipidus?
- Neurogenic Diabetes Insipidus. It is caused by:
- Trauma, tumor, or inflammation of the brain (Hypothalamus).
- ADH level is low.
- Surgical ablation of the pituitary gland or mass lesion.
- X-linked recessive familial form.
- Nephrogenic diabetes insipidus. It is caused by:
- The renal collecting system’s unresponsiveness to ADH.
- ADH level is raised.
- Hypercalcemia.
- Hypokalemia.
- A very low protein diet.
- Lithium therapy.
- The release of a long-standing obstruction.
- Aging may be associated with partial nephrogenic diabetes inspidus.
- The renal collecting system’s unresponsiveness to ADH.
What are the criteria for Diabetes insipidus?
- There are polyuria and polydipsia.
- Low urine osmolarity.
- Hypernatremia.
How will you diagnose Diabetes inspidus?
- Before starting the test for diabetes insipidus, advise the following tests with unrestricted diet and water intake:
- Urine output >2000 mL/day.
- Urine is hypotonic with osmolality <300 mosm/kg body weight/day (range is 200 to 300 mosm/kg).
- The above findings favor the diagnosis of diabetes insipidus.
- In that case, measure solute contents /day.
- If the solute excretion is <20 mosm/kg/day, it indicates diabetes insipidus.
- The D/D of polyuria excludes:
- Osmotic diuretics like glucose, mannitol, and sodium chloride.
- Diuretic therapy.
- Severe chronic renal disease.
- After acute tubular necrosis.
- After renal transplantation.
- Pregnancy-induced.
- Hypercalcemia.
- Hypokalemia.
- Drugs like lithium, chlorpromazine, and thiazide.
- Sickle cell disease.
- Water deprivation or dehydration test:
- Before starting the test to find the etiology, it is recommended to note the following:
- 24-hour urine volume.
- The osmolality of urine.
- Amount of solute excreted in the urine.
- Serum sodium, potassium, calcium, and osmolality without any restriction of the diet or water are recorded.
- When the Results show the following value, then think about Diabetes Inspidus:
- Excess urine output.
- Urine is hypotonic.
- Stop all medications that can influence the release of ADH before 24 hours and during the test, like:
- Alcohol.
- Tobacco.
- All caffeine-containing drinks.
- This test is done by overnight deprivation of water.
- Record the serum osmolality and sodium levels before and after the administration of vasopressin.
- This is followed by the administration of ADH (Vasopressin). Inject subcutaneously either 1 µg of desmopressin (a synthetic analog of ADH) or 5 IU of ADH (vasopressin).
- Collect urine samples for 30, 60, and 120 minutes.
- Result:
- Urine osmolality after the injection of ADH is less than 50% higher than the baseline urine osmolality, which favors diabetes insipidus (nephrogenic type).
- If there is an increase equal to or greater than 50%, consider a diagnosis of neurogenic diabetes insipidus.
- In a healthy person, urine osmolarity increases during water deprivation.
- Administration of vasopressin has an additional effect on urine concentration.
- In the case of neurogenic diabetes inspidus:
- No urine concentration in response to water deprivation.
- When vasopressin is given, urine osmolarity increases.
- The Serum ADH level is low.
- While in the case of nephrogenic diabetes inspidus:
- Urine cannot be concentrated in either case.
- There is no increase in urine osmolality after water deprivation or after administration of vasopressin.
- The Serum ADH level is high.
- The standard diagnostic test for Diabetes Insipidus is the water deprivation test.
- ADH presence leads to a small volume of concentrated urine.
- ADH absence leads to a large volume of diluted urine.
What causes the stimulation of Anti-diuretic hormone (ADH)?
- Increase in serum osmolality.
- A decrease in intravascular blood volume.
- Sleep
- At night.
- In an erect position.
- With pain.
- In surgery.
- Physical Stress.
- High level of anxiety.
- Exercise.
- Chemical agents like catecholamine, opiates, nicotine, anesthesia drugs, barbiturates, and angiotensin ii.
What causes inhibition of Antidiuretic hormone (ADH)?
- The increase in plasma volume.
- The decrease in plasma osmolality.
- Alcohol.
- Phenytoin.
- Glucocorticoids
What is the normal Antidiuretic Hormone (ADH)?
Source 2
- 1 to 5 pg/ mL or <1.5 ng/L.
- Or < 2.5 pg/mL.
How will you discuss the ADH suppression test, also known as the water load test?
- 65% of the water load is excreted in 4 hours.
- 80% of the water load is excreted in 5 hours.
- Urine osmolality in the second hour = ≤100 mmol/kg
- Urine to serum (U/S) osmolality ratio = >100
- Urine specific gravity = <1.003
Another source
- 2 to 8 pg/mL
Source 4
- <2.5 pg/mL or <2.3 mmol/L
What are the causes of increased Antidiuretic Hormone (ADH) levels?
- Hyperfunction of the ADH state gives rise to the Syndrome of inappropriate antidiuretic hormone secretion (SIADH).
- There is a sustained release of ADH in the absence of a known cause.
- Central nervous system diseases, such as tumors or infections.
- Pulmonary tuberculosis or pneumonia.
- Lung cancer (ectopic ADH).
- Nephrogenic diabetes insipidus due to renal diseases.
- Myxedema.
- Physical stress, such as pain and trauma.
- Hypovolemia.
- Dehydration.
- Acute and intermittent porphyria.
- Guillain-barre syndrome.
What are the causes of decreased Antidiuretic Hormone (ADH) level?
- Hypofunction of ADH results in a polyuric state.
- Urine output is more than 2.5 L/day.
- Nephrogenic diabetes insipidus.
- Nephrotic syndrome.
- Water intoxication (psychogenic polydipsia).
- Surgical ablation of the pituitary gland.
- Hypervolemia.
- Decreased serum osmolality.
- This polyuric state is divided into:
- Hypothalamic diabetes inspidus.
- Nephrogenic diabetes inspidus.
- Psychogenic polydipsia.
Questions and answers:
Question 1: What will be sodium in diabetes insipidus?
Question 2: What are the types of diabetes insipidus?