Anemia:- Part 9 – Sideroblastic Anemia, and Anemia Due To Chronic Diseases
Sideroblastic anemia:
Sample for Sideroblastic Anemia
- EDTA blood is needed.
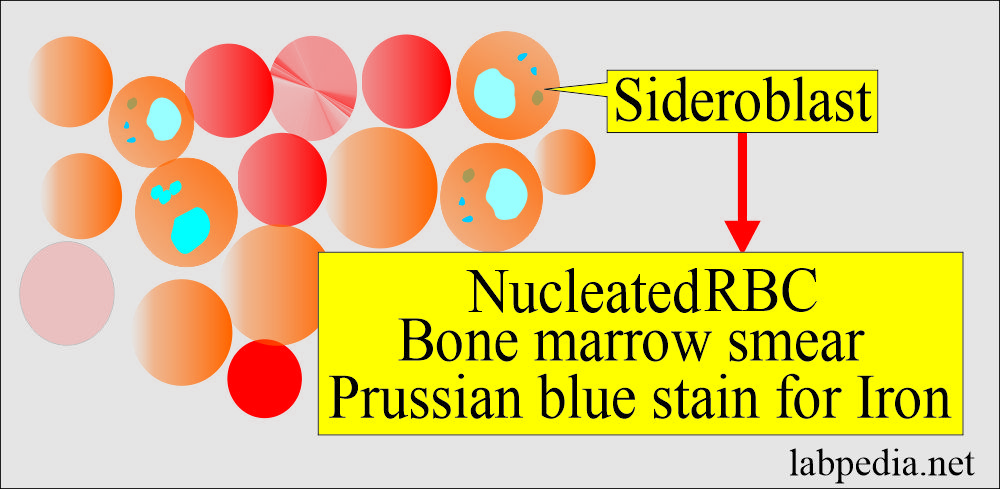
- Bone marrow smear for iron stain.
Definition of sideroblastic anemia:
- Sideroblastic anemia indicates a group of disorders with the presentation of:
- Anemia.
- Ineffective erythropoiesis.
- Increased serum and tissue iron.
- Increased number of ringed sideroblastic RBCs in the bone marrow aspirate (at least 20%).
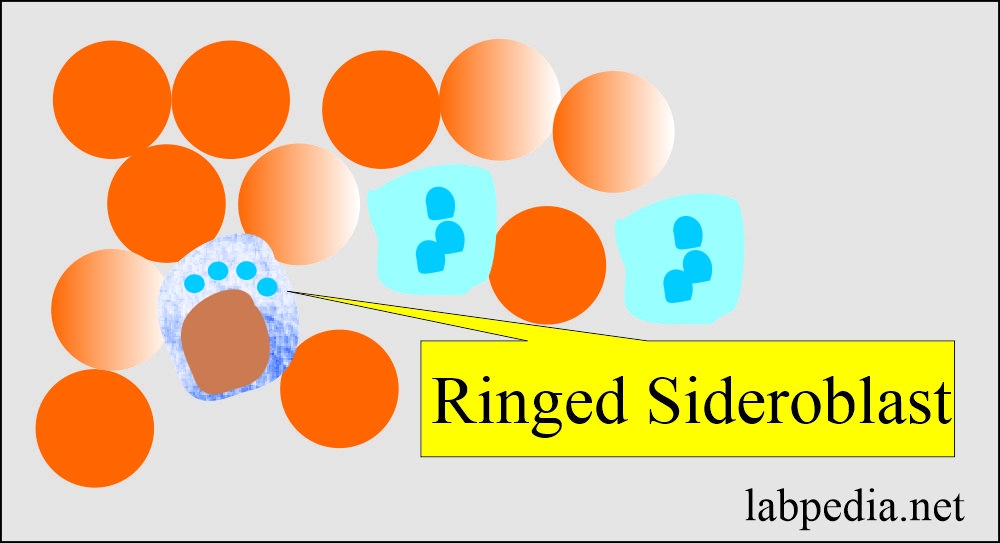
- Sideroblasts are normoblasts with abnormal stainable iron in the cytoplasm that form a ring around the nucleus.
- Normoblast contains ferritin. These cells are absent in iron deficiency anemia and anemia due to chronic infection.
- Siderocytes are normal reticulocytes that contain iron in the form of ferritin or hemosiderin in the mitochondria. These cells have no diagnostic importance.
- These anemias are due to abnormalities of heme synthesis.
- To qualify the sideroblastic anemia, >15% of ringed sideroblasts are to be found in the following:
- Congenital (inherited):
- This includes sex-linked congenital sideroblastic anemia.
- Autosommal recessive sideroblastic anemia.
- Acquired (drug-induced):
- Primary or idiopathic.
- Myelodysplasia.
- Secondary.
- Lead.
- Alcoholism.
- Thalassemia.
- Drugs include isoniazid and chloramphenicol.
- This may be seen in malignancies or malabsorption.
- Primary or idiopathic.
Pathophysiology of sideroblastic anemia:
- The pathogenesis is incompletely understood.
- It is due to abnormalities of heme metabolism.
- Several investigators found enzyme deficiency, including the deficiency of ALA synthase and uroporphyrinogen decarboxylase in these patients.
- Irrespective of the etiology, there is an abnormal deposition of iron or siderotic granules in normoblast mitochondria. The mitochondria are present around the nucleus.
- The body has an adequate amount of iron, but it cannot incorporate into hemoglobin.
- The iron (Fe) enters the developing RBCs but accumulates in the normoblast’s perinuclear mitochondria in primary sideroblastic anemia.
Classification of sideroblastic anemia:
A. Inherited type:
- This is rare and is sex-linked.
- Sex-linked (X-linked) anemia is more common than Autosomal recessive sideroblastic anemia.
- The responsible gene is ALAS2, found on the sex chromosome X.
- Pyridoxine-responsive.
- Pyridoxine-refractory.
- Autosomal, pyridoxine-refractory.
- These sideroblastic anemias are usually present in childhood.
- MCV is usually low, and RDW is usually high.
B. Acquired type:
- Primary (idiopathic).
- Myelodysplasia.
- Secondary:
- Associated with myeloproliferative disorders like leukemia and polycythemia vera.
- Pyridoxine deficiency (responsive anemia):
- Alcoholism.
- Drugs induced like INH, cycloserine, chloramphenicol, and chemotherapy.
- Vitamin B12 deficiency.
- Hemoglobin synthesis defects:
- Deficiency of vitamin B12 and folic acid.
- Erythropoietic porphyria.
- Lead poisoning.
- Radiation.
- Other diseases are e.g., rheumatoid arthritis, carcinoma, megaloblastic, hemolytic anemia, hemolytic anemia, and malabsorption.
- A specially acquired rare form of Pearson syndrome has sideroblastic anemia, pancreatic insufficiency, and copper deficiency.
- Pyridoxine-responsive anemia:
- Classical type.
- Variant forms.
Signs and symptoms of sideroblastic anemia:
- Typically anemia appears early, usually within the first few months or years of life.
- The patients will show pallor and splenomegaly in the sideroblastic anemia.
Lab findings of sideroblastic anemia are:
- The diagnostic feature is nucleated RBCs with iron granules called ringed sideroblasts, present in the bone marrow and dimorphic picture in the peripheral blood smear.
- Hemoglobin is low.
- MCV is variable and may be low, normal, or increased.
- MCH and MCHC are often low but may be normal.
- White blood cells may show abnormality.
- RDW is increased.
- Serum iron is usually more than normal. There may be increased or normal iron stores.
- Ferritin level is also increased.
- Transferrin% saturation is high.
- The serum ferritin level is markedly raised.
- The serum B12 and folic acid levels are normal.
- Raised bilirubin level.
- LDH is raised.
- Decreased serum haptoglobin.
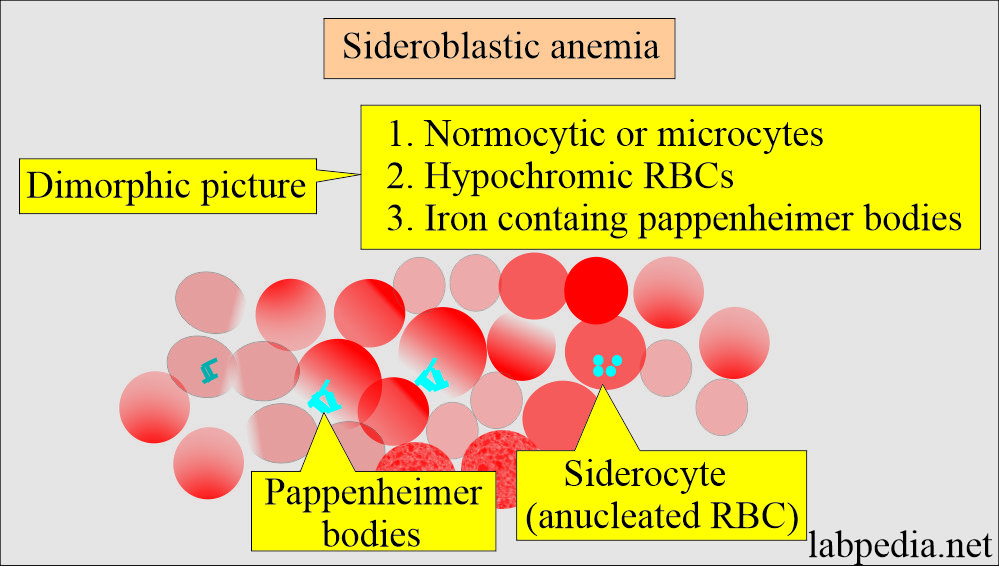
- Peripheral blood smears:
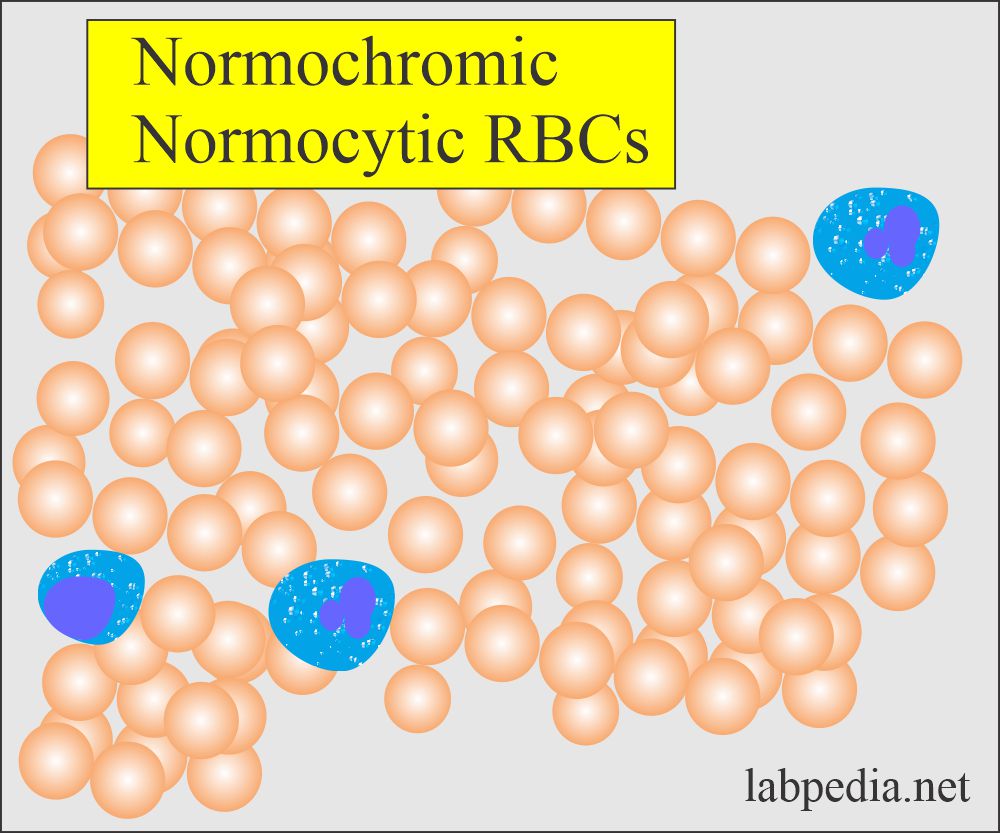
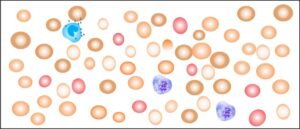
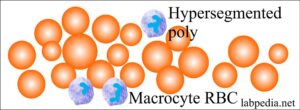
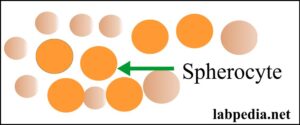
- It shows a dimorphic picture with the presence of normocytic (normal RBCs) and microcytic and hypochromic RBCs (small-size RBCs). Occasional macrocytes are seen.
- Microcytosis is more common in the inherited form of sideroblastic anemia.
- Peripheral blood smears show hypochromic anemia, which is microcytic, normochromic, or macrocytic (dimorphic picture).
- The dimorphic picture is seen in the primary type. It is prominent anisopoikilocytosis.
- The microcytic form is seen mostly in the inherited form of sideroblastic anemia. In comparison, the macrocytic form is seen in the acquired form.
- There may be seen iron-containing Papenheimer bodies, and may look like basophilic stippling.
- Bone marrow:
- It shows erythroid hyperplasia, but circulating reticulocytes are not increased (ineffective erythropoiesis).
- There are sideroblasts in the bone marrow aspirate. and these are >15%.
- Cytogenetics study shows a chromosomal anomaly in 25% to 50% of the cases.
- There are increased or normal iron stores.
Treatment of sideroblastic anemia:
- Treat the cause. Some patients respond when alcohol and drugs are stopped.
- In the primary type, these are unresponsive to various vitamins, especially pyridoxine (another reference says some patient responds to pyridoxine).
- Folic acid may be given in case of folate deficiency.
Anemia due to chronic diseases
Definition of anemia due to chronic diseases:
- This anemia occurs mostly in chronic inflammatory and malignant diseases.
- The anemia is present for several months following chronic diseases (which is present for several months).
- These are commonly associated with infections, malignant neoplasms, and autoimmune disorders.
- It is usually normocytic and either normocytic or hypochromic anemia.
Pathogenesis of anemia due to chronic diseases:
- The mechanism of this anemia is not clearly understood.
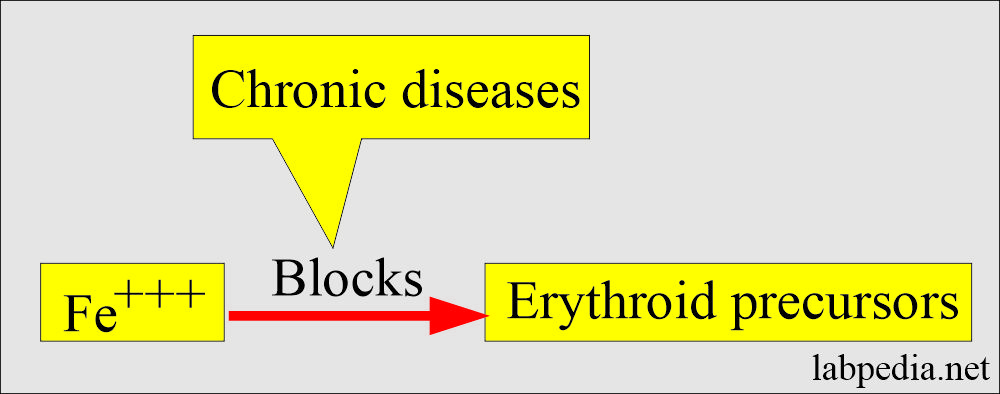
- The basic defect is in the iron utilization for erythropoiesis.
- It looks like there is a block of iron delivery from the reticuloendothelial system to RBCs.
- A chronic disease state blocks the transfer of stored iron to maturing erythroid precursors within the bone marrow.
- This will lead to iron deficiency in RBCs while the stores have abundant iron.
- There is a decreased release of iron from the macrophages to plasma.
- RBCs’ life span is reduced.
- Inadequate erythropoietin response to anemia is caused by the effect of cytokines like IL-1 and tumor necrosis factor (TNF) on erythropoiesis.
- Hepcidin, released by the liver in response to inflammation, will inhibit macrophages’ iron release and absorption.
- The anemia will respond to successful treatment of the cause but no response to iron therapy.
- Anemia due to chronic diseases may be due to:
- Decreased Erythropoietin response by the RBCs.
- Decreased RBCs survival.
- Defective iron absorption.
- Cytokines block the release of iron from the reticuloendothelial system for the development of RBCs.
Causes of anemia due to chronic diseases:
- This is seen in collagen diseases (autoimmune diseases).
- Systemic lupus erythematosus.
- Rheumatoid arthritis.
- Sarcoidosis.
- Inflammatory chronic conditions.
- Tuberculosis.
- Chronic osteomyelitis.
- Fungal infection.
- Malignancies.
- Carcinoma.
- Lymphomas.
- Multiple myeloma.
Causes of anemia due to chronic diseases:
| Group of the anemia | Causes of the chronic diseases |
|
|
|
|
|
|
|
|
Signs and symptoms of anemia due to chronic diseases:
- Anemia appears for several months after the chronic disease.
- Anemia usually presents 1 to 3 months following the onset of chronic disease.
Lab findings of anemia due to chronic diseases:
- There is Low hemoglobin (7 to 11 g/dL).
- MCV is normal.
- RBCs may be normal or microcytic and hypochromic RBCs. This microcytosis is not as severe as iron deficiency anemia.
- Usually normocytic RBCs with normal MCV, rarely MCV is <75 fl.
- In some cases, we may see hypochromic or normochromic RBCs.
- Decreased Serum iron.
- TIBC is normal or decreased.
- The serum ferritin is normal or increased.
- There is a decreased % saturation.
- Normal to increased serum ferritin level.
- It needs to differentiate from iron deficiency anemia.
- Decreased sideroblastic cells (rare to absent ringed sideroblast).
Lab findings of the anemia due to chronic diseases:
| Lab test | Clinical parameters |
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
Table showing findings in various anemias:
| Type of anemia | Hb | MCV | MCH | MCHC |
|---|---|---|---|---|
| Iron deficiency | low | low | low | low |
| Megaloblastic | low | high | high | normal |
| Thalassemia | low | low | low | low |
| Chronic illness | low | low | low | low |
Characteristic Findings in Various Anemias:
Anemia type |
HB |
MCV |
MCH |
MCHC |
Ferritin |
Iron binding capacity |
serum iron |
RDW |
| Iron deficiency | low | low <76 fl | low | low/normal | decreased | increased | decreased | increased |
| Megaloblastic | low | high >100 fl/cell |
increased >32 pg |
low 32 to 36 g/dL | raised/normal | increased | ||
| Chronic illness | low | low/normal | low | low | normal/ increased | normal / decreased | decreased | normal |
| Alpha Thalassemia | low or normal | low | low | low | normal /increased | normal |
normal or increased |
increased |
| Beta Thalassemia | low | low | low | low | increased/normal | normal | increased/normal | increased |
| Aplastic anemia | low | increased | normal | normal | normal |
Classification of anemia based on RDW:
| Cell size | Normal RDW | High RDW |
| Microcytosis |
|
|
| Normocytic |
|
|
| Macrocytosis |
|
|
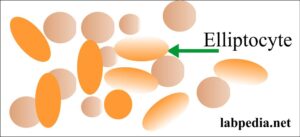
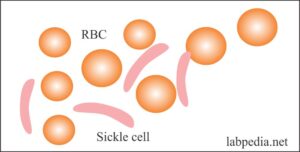
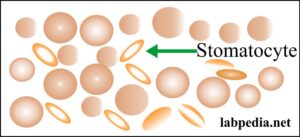
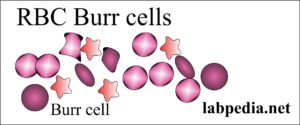
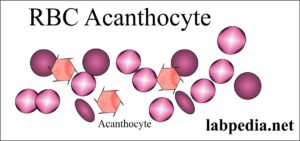
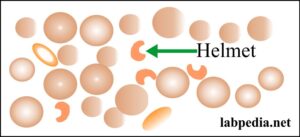
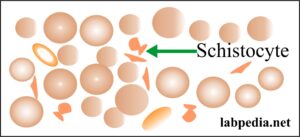
Abnormalities of RBCs morphology and their etiology:
Summary of lab findings in various anemias:
| Lab test | Iron-deficiency anemia | Pernicious anemia | Folic acid deficiency | Aplastic anemia | Thalassemia | Sideroblastic anemia | Hemolytic anemia | Post hemorrhagic anemia | Anemia of chronic diseases |
| Hemoglobin | Low | Low | Low | Low or normal | Low | Low | Low | Normal or low | Low |
| Hematocrit | Low | Low | Low | Low or normal | Low | Low | Low | Normal or low | Low |
| MCV | Low | High | High | A normal or mild increase | Low | Low | Normal or high | Slightly low | Low or normal |
| Reticulocytes count | A normal or mild increase | Low | Low | Low | Increased | A normal or mild increase | High | Increased | Normal |
| Plasma Iron | Low | Increased | Increased | Increased | Increased or normal | Increased | Normal or high | Normal | Low |
| TIBC | Increased | Normal | Normal | Normal | Normal | Normal | Normal | Normal | Low |
| Ferritin level | Low | Increased | Increased | Normal | Increased or normal | Increased | Normal | Normal | Normal |
| Folate level | Normal | Normal | Low | Normal | Normal | Normal | Normal | Normal | Normal |
| Serum B12 level | Normal | Low | Normal | Normal | Normal | Normal | Normal | Normal | Normal |
| Transferrin | Low | Mild increase | Mild increase | Normal | Increased | Normal | Normal | Mildly low | |
| Bilirubin | Increased |
Questions and answers:
Question 1: What is peripheral blood picture of sideroblastic anemia.
Question 2: What is the mechanism of anemia due to chronic diseases?.