Anemia:- Part 2 – Iron Deficiency Anemia, Microcytic and hypochromic anemia, Diagnosis and Management
Iron Deficiency Anemia
What sample is needed for Iron Deficiency Anemia?
- Take the blood in EDTA.
- Make a fresh peripheral blood smear.
- For iron, draw the first-morning blood sample because of the diurnal variation.
How will you define Iron Deficiency Anemia?
- Anemia is defined as a reduction in the mass of circulating RBCs and decreased hemoglobin concentration.
- Iron deficiency is the most common cause of anemia, and iron is the most common dietary deficiency globally.
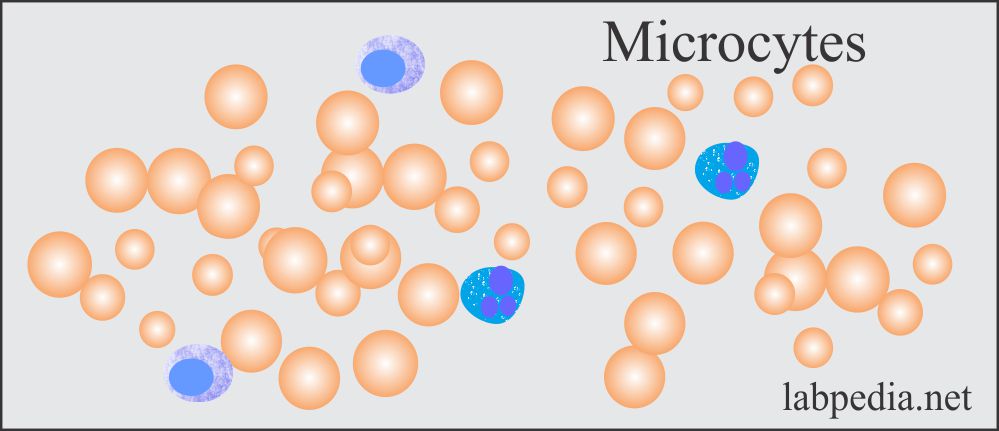
- Iron deficiency results in decreased quantity defects in hemoglobin production, which leads to small, pale microcytic, and hypochromic RBCs.
- DNA synthesis is normal.
- Iron-deficiency anemias are divided into three groups:
- Iron metabolism occurs when there is an iron deficiency.
- Disorders of heme synthesis are seen in sideroblastic anemia.
- Disorder of globin protein synthesis is seen in Thalassemia.
What are the causes of Iron deficiency anemia?
- Inadequate intake of iron:
- Meat, eggs, and green leafy vegetables are good sources of iron.
- Pregnant ladies and children need a more iron-rich diet.
- Pregnancy or increased blood loss in menstruation leads to iron deficiency.
- Internal bleeding in stomach ulcers and polyps of the gastrointestinal tract.
- Too much use of aspirin may cause internal bleeding.
- Esophageal varices.
- In the case of partial gastrectomy.
- Carcinoma of the stomach, caecum, colon, or rectum.
- Bleeding from the hemorrhoids.
- Rarely hematuria, hemoglobinuria, and self-inflicted blood loss.
- Parasitic infestation by the hookworm.
- Malabsorption includes Gluten-induced enteropathy and gastrectomy.
- Inability to absorb iron from the GIT, like in bypass surgery of the stomach or intestine, and Celiac disease.
- In the case of gastric, duodenal, or jejunal resection.
- People at risk of developing iron deficiency are:
- Ladies of childbearing age.
- People with a poor diet.
- People who frequently donate blood or professional donors.
- A vegetarian who does not eat meat or iron-rich foods.
- Infants or children who are mainly on milk do not take solid foods.
- Poor diet in poor people.
- Pregnancy and lactation are times when more iron is needed. In pregnancy, iron needs may be around 1000 mg. There is an increased maternal red cell mass of roughly 35%. There is the diversion of iron to the fetus.
- 300 mg of iron is transferred to the fetus.
- There is blood loss during the delivery.
- An iron supplement is needed if the Hb is below 10 g/dL or the MCV is <82 fL in the third trimester.
Another reference for iron deficiency anemia:
- Bleeding is the most common cause.
- Newborns and children have bleeding from Meckel’s diverticulum.
- A male <50 years of age has bleeding from a peptic ulcer (duodenal and gastric ulcers).
- A female <50 years of age has menorrhagia.
- Males and females>50 years of age have gastrointestinal bleeding from a polyp or colorectal cancer.
What are the causes of iron deficiency anemia in infants and adults?
| Infants/adults | Causes |
|
|
|
|
What are the causes of iron deficiency?
- Decreased Iron stores:
- Iron stores are depleted. There is decreased serum ferritin.
- Defective hemoglobin synthesis:
- There is a deficiency of iron, which will lead to defective hemoglobin synthesis.
- There will be decreased serum iron.
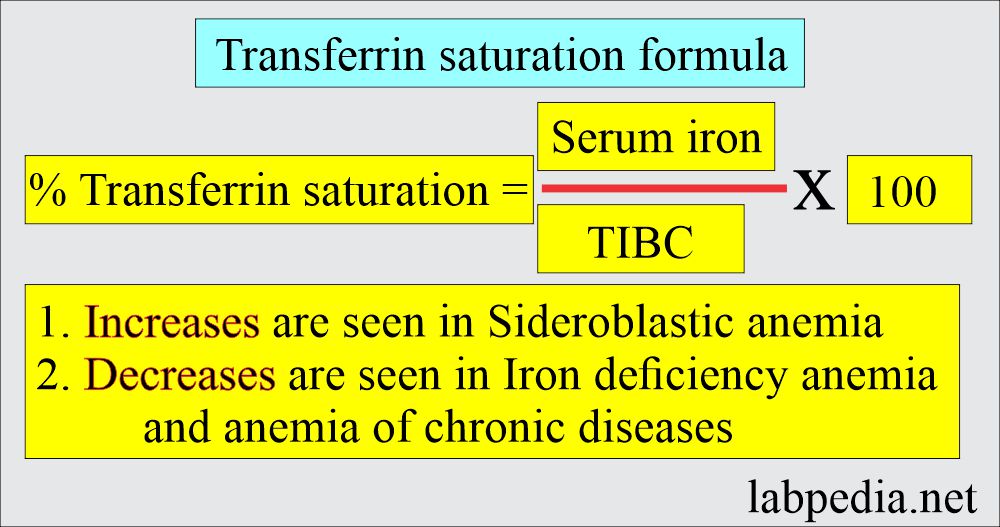
- There is decreased transferrin saturation.
- There is an increased RBC protoporphyrin.
- There is an increased total iron-binding capacity (TIBC);
- The patient will be anemic.
- Development of anemia:
- There will be hypochromic and microcytic anemia. The patient will show the following:
- Low Hb.
- Decreased Hct.
- Decreased RBC count.
- Decreased MCV.
- It increased serum soluble-transferrin receptors.
- Serum ferritin <15 ng/mL (more sensitive and specific).
What are the functions of iron?
- Iron is needed for some of the essential processes, like:
- Transport of oxygen.
- It plays a role in the development of RBCs.
- Iron is necessary for hemoglobin formation.
- Myoglobin function.
- It modulates the enzyme activity involved in cellular respiration and energy production with the help of ATP.
- Iron supports the immune system.
- It plays a role in promoting cognitive performance.
- It plays an important role in the nutrition of the epithelial cells.
- This is the property of iron to interact reversibly with O2, and it functions in electron-transfer reactions that will make it biologically important.
How will you discuss the Iron metabolism in the body?
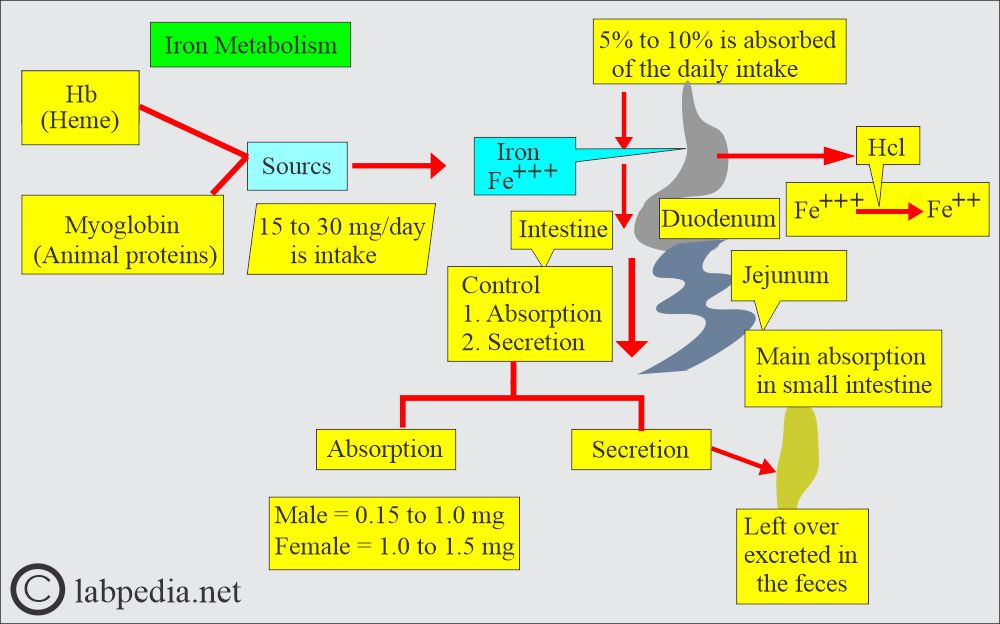
- The iron requirement for the body is dependent upon age, sex, and the physiology of the body.
- Iron is one of the most important components of hemoglobin.
- Most of the iron in humans is present in the porphyrin ring of heme, which will ultimately become part of hemoglobin, myoglobin, catalase, peroxidase, and cytochrome.
- Solubility of the iron depends upon the following factors:
- Gastric acidity and other substances, such as ascorbic acid, sugars, and amino acids, keep iron soluble.
- Decrease iron absorption by the following agents (form insoluble complexes):
- Phosphate in milk, eggs, and cheese.
- Oxalates and phytates in vegetables.
- Tannates in the tea.
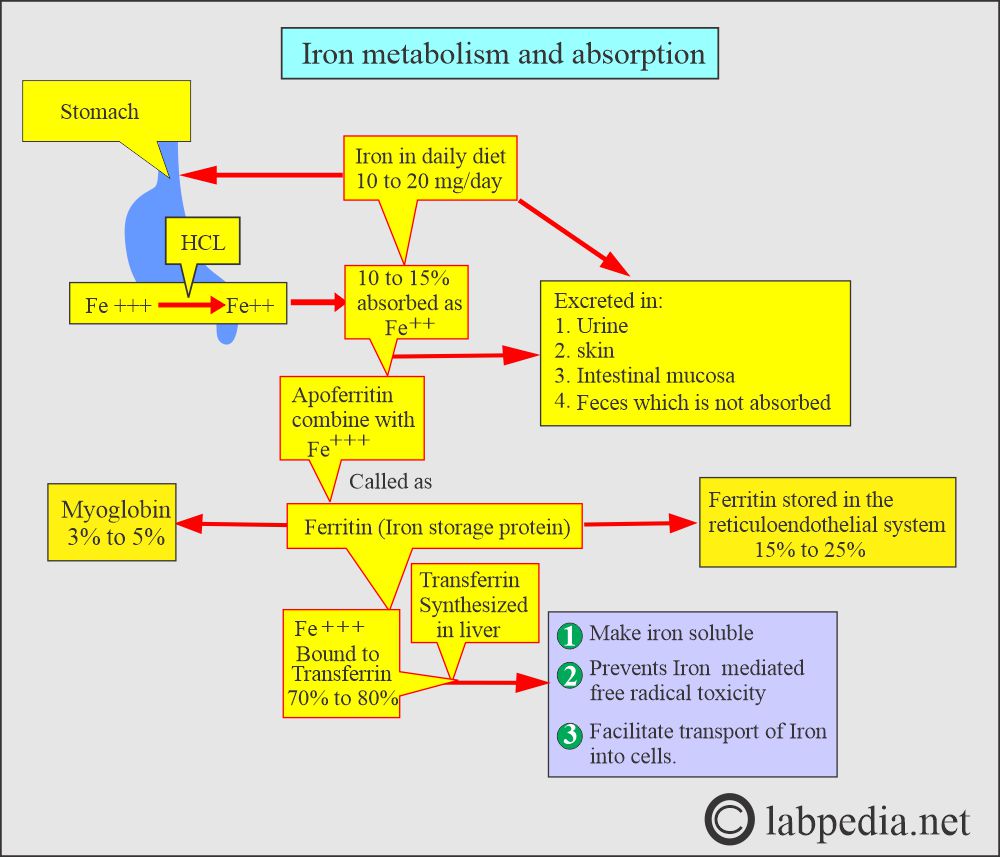
- Iron is taken in ferric form and changed to ferrous form in the stomach by Hydrochloric acid.
- It is then absorbed mainly in the small intestinal epithelial cells at the apical end, where the ferrireductase enzyme helps convert it from the Ferric (Fe +++) form to the ferrous (Fe ++) form.
- Iron absorption depends upon the following:
- Iron body stores.
- Rate of RBC cell production.
- In need, iron absorption can be increased threefold or more.
- Iron absorption is increased in times of need, like in pregnancy and some anemias.
- Iron absorption will decrease if a large amount of supplemental iron is used.
- Iron may be stored as ferritin.
How will iron be lost by the body?
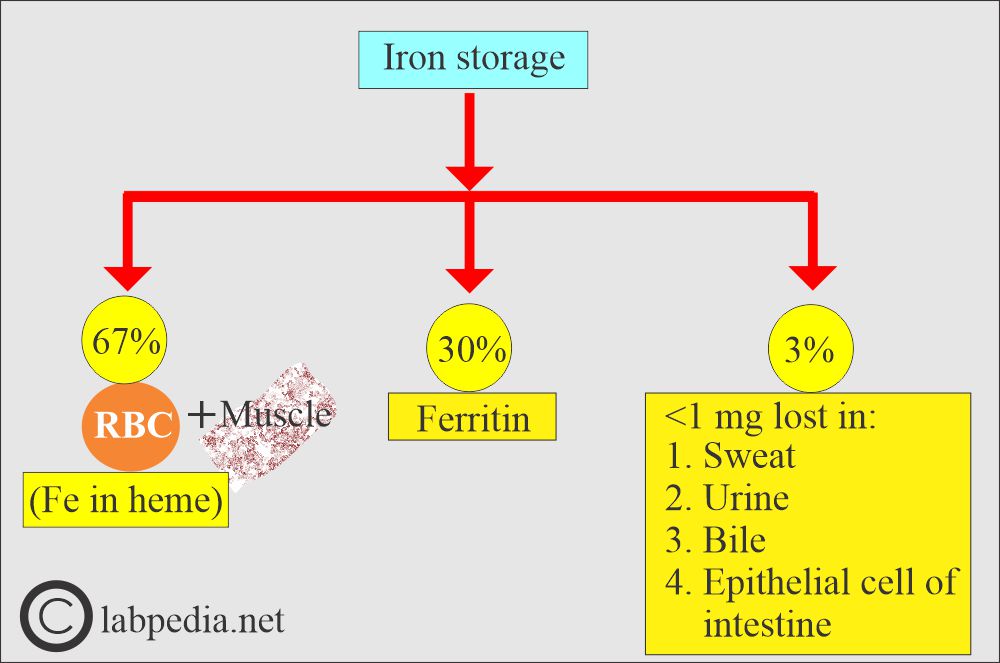
- There is a daily loss of iron of roughly 1 mg/day through:
- Shedding of the skin epithelial cells.
- Shedding of the lining epithelial cells of the gastrointestinal and urinary systems (most of the iron is lost by the shedding of the epithelial cells).
- The leftover is excreted in the feces.
- A small number of RBCs are lost in the urine and feces.
- Iron loss is continuous and is mostly an unregulated process, but the iron balance is controlled by absorption.
- It indicates that 1 mg of iron daily is sufficient for males and post-menopausal females.
- Females, during menses, needed 2 mg of iron/day.
- Iron is lost during the delivery, diverted to the fetus, and breastfeeding; this is an average of 900 mg.
- The increased demand for iron is roughly 3 to 4 mg/day in pregnancy and lactation.
What are the storage forms of iron?
- Iron is stored in two forms:
- Ferritin.
- Hemosiderin.
- Decreased iron in hemoglobin leads to anemia.
- Hemoglobin contains roughly 37% of iron by weight.
- Daily iron in the diet is approximately 10 to 20 mg/day.
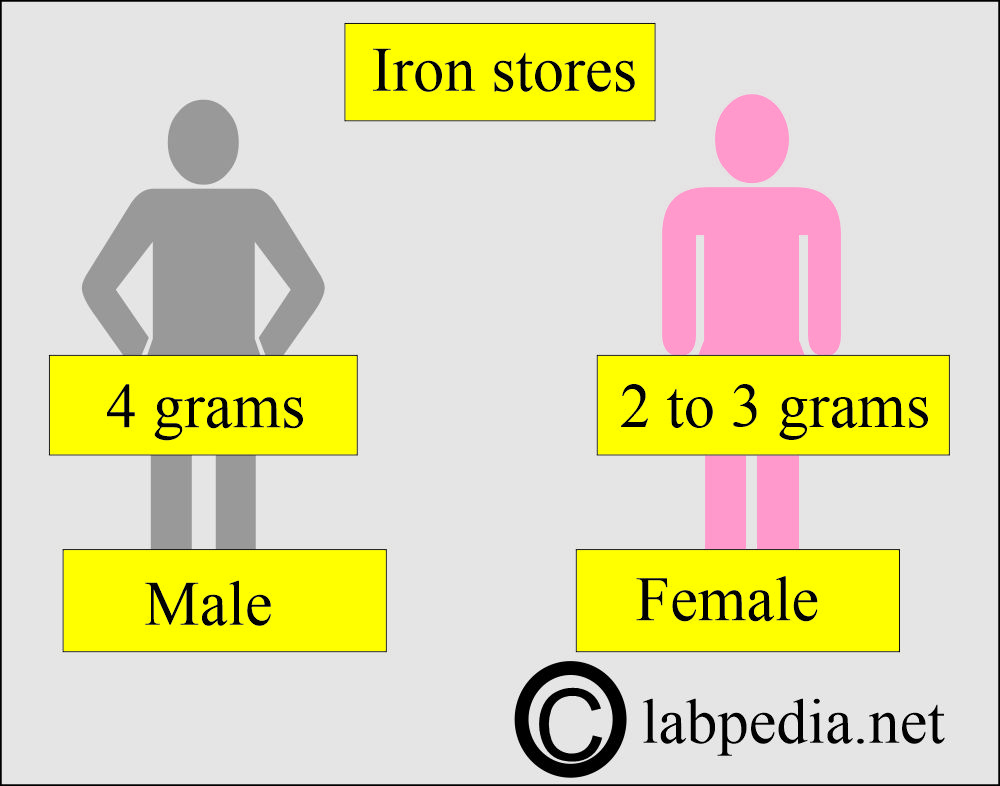
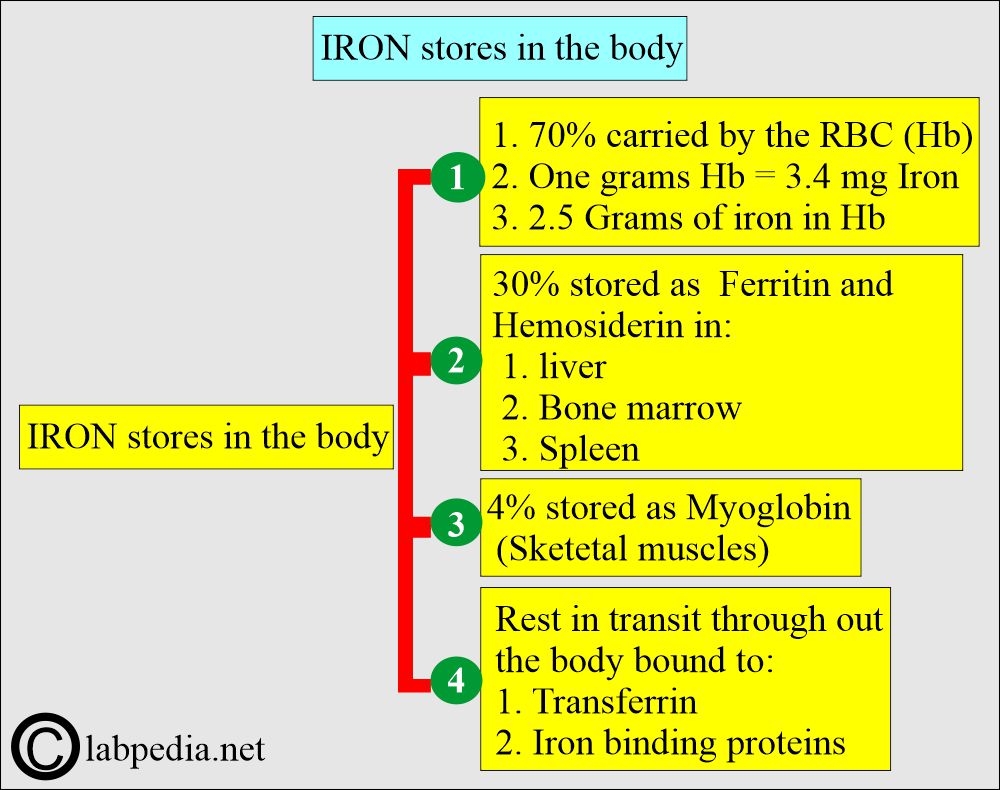
- An average male adult’s body contains 4 grams of iron.
- 10% are located in myoglobin and other iron-containing enzymes and proteins.
- 65% to 70% of iron is found in hemoglobin.
- The rest, 20% to 25%, is the iron storage pool.
- An average female adult contains 2 to 3 grams of iron in her body.
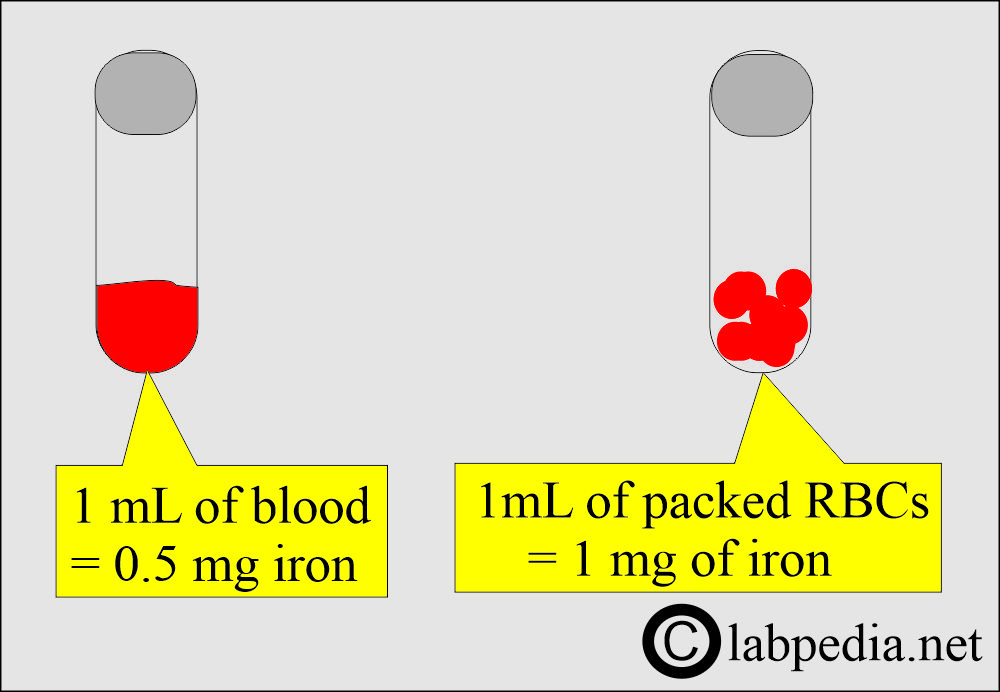
- One ml of whole blood contains 0.5 mg of iron, and one ml of packed RBCs contains 1 mg of iron.
- The body uses 1 mg of iron daily, and 1000 mg of iron is stored.
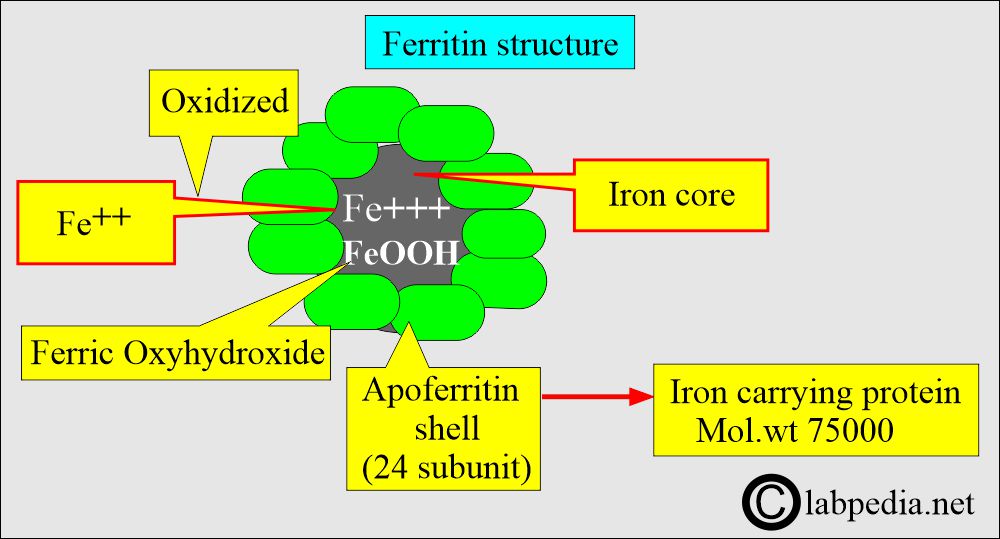
- It then combines apoferritin (protein) and makes a complex of ferritin.
- Iron is stored as ferritin in the body.
- Body Iron reserve is stored in the following:
- 1/3 in the liver.
- 1/3 in the bone marrow.
- Rest in the spleen and other tissues.
What is the role of Transferrin and Ferritin?
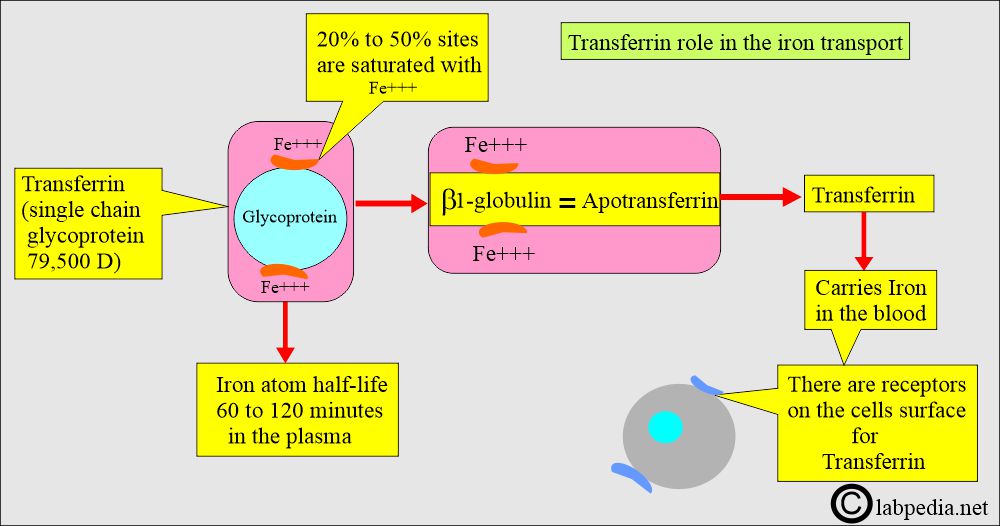
- Ferric ions combine with the Transferrin, which is synthesized in the liver.
- Transferrin helps:
- Make an iron-soluble form.
- It prevents iron-mediated free radical toxicity.
- This facilitates iron transport into the cells.
- Transferrin, a glycoprotein, is the transport protein for iron in the blood.
- Ferritin:
- Iron is stored as ferritin in hepatocytes, macrophagic cells (bone marrow), RBCs, and muscles.
- It releases iron for the formation of hemoglobin and heme protein.
- Ferritin consists of a multisubunit protein shell, known as apoferritin, surrounding a core of up to 4500 iron atoms.
- Iron in ferritin is deposited in its core as a ferric hydroxy phosphate complex.
- Ferritin is present in most cells and is readily available whenever needed as a mobilized form of storage iron.
- Hemosiderin is an insoluble form derived from ferritin.
- It is visible by light microscopy with special stains (Prussian blue dye).
- Hemosiderin has a higher iron concentration than ferritin, releasing iron slowly.
What are the signs and symptoms of Iron deficiency anemia?
- Iron deficiency anemia is more common in children, young females, and older people.
- There is an increased need for infants, children, and pregnant women.
- In females, iron deficiency occurs due to menstrual cycles.
- Chronic blood loss from the GI tract is the usual reason for iron deficiency.
- There is general fatigue and weakness.
- Skin is pale, and the conjunctivae will also be pale.
- The patient may feel dizzy.
- These patients, particularly children, crave to eat dirt, ice, or clay. Sometimes these children lick the walls.
- There may be a feeling of tingling or crawling in the legs.
- Patients have cold hands and feet.
- These patients may have tachycardia, a fast or irregular heartbeat.
- Sometimes have a headache.
- The nails are brittle.
- Nails have a spooning called koilonychia.
- The tongue has soreness or swelling (glossitis).
- There is a renal cell carcinoma case report with microcytosis and normochromic anemia.
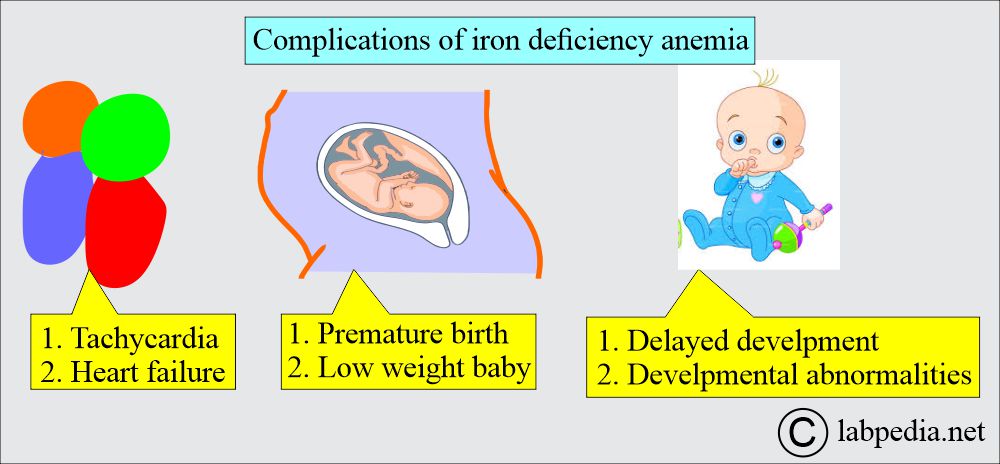
What are the complications of Iron deficiency anemia?
- There is tachycardia, which may lead to heart failure and an enlarged heart.
- In pregnancy, there may be premature birth and low birth weight of the baby.
- Children and infants may have delayed development and developmental abnormalities.
What are the lab findings in iron deficiency anemia?
Initial events:
- Decreased serum ferritin is the early sign, followed by a decrease in the % saturation of transferrin, decreased serum iron, and increased zinc protoporphyrin (ZPP), followed by:
- Fall in hemoglobin.
- MCV progressively drops, and ultimately below 80 fl.
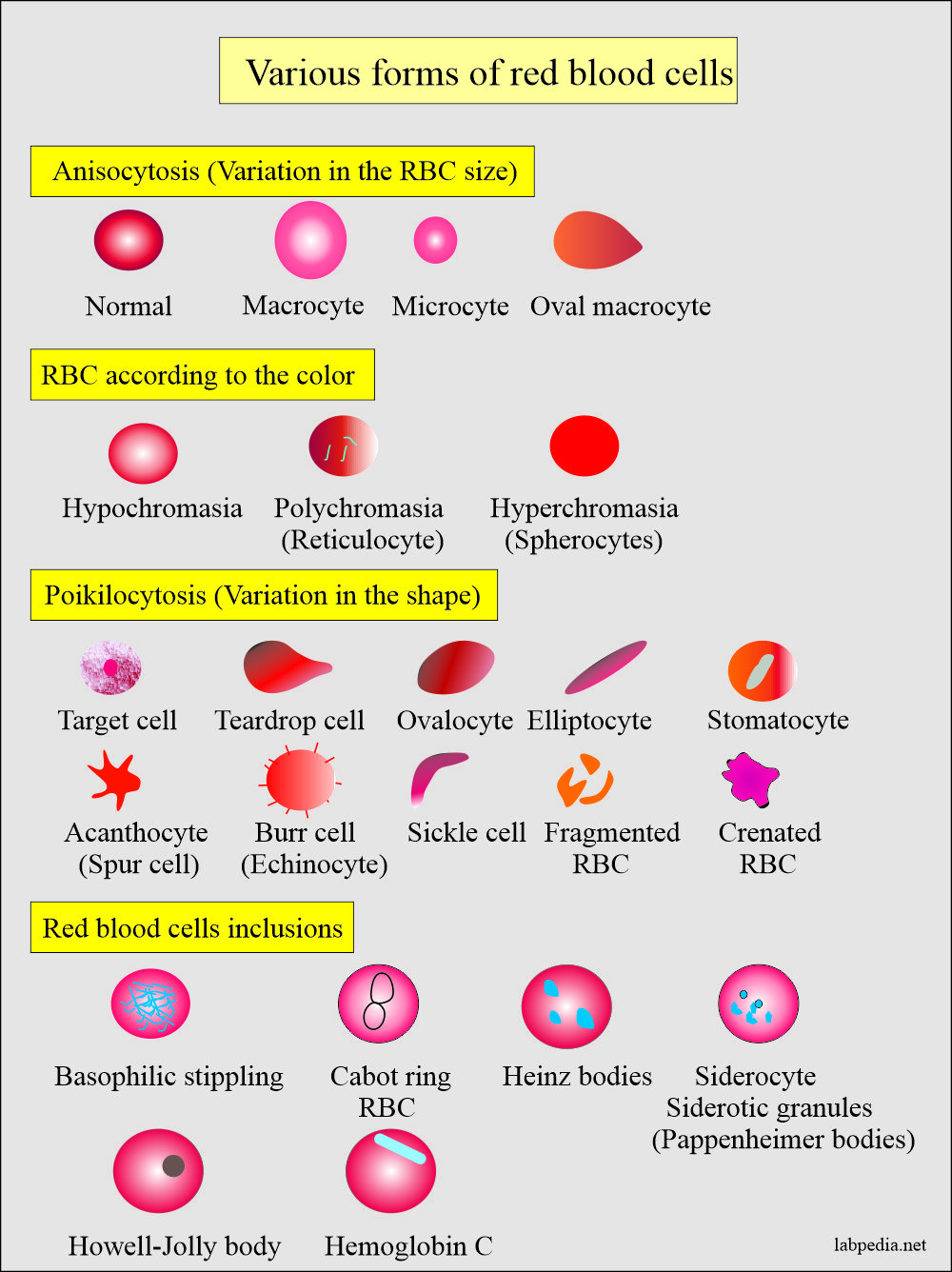
- RBCs become hypochromic microcytic and poikilocytosis.
- Other Laboratory findings are:
- MCV is reduced to 50 to 60 fl (where the normal value is 77 to 93 fl).
- MCH is reduced to 15 to 20 pg (where the normal value is 27 to 32 pg).
- MCHC is reduced to 20 to 25 g/dl (where the normal value is 31 to 35 g/dl).
- The serum iron level is decreased (very low). Normal serum iron is 50 to 150 µg/dL.
- The serum ferritin level is low, <10 ng/dL.
- Raised total iron-binding capacity (TIBC). Normal TIBC is 250 to 450 µg/dL.
- Percent transferrin saturation normal value is 20% to 50%, and normally transferrin is 33% saturated.
- RBC protoporphyrins increased.
- The peripheral blood smear shows anisocytosis and poikilocytosis in the presence of target cells.
- There are microcytic, hypochromic red blood cells.
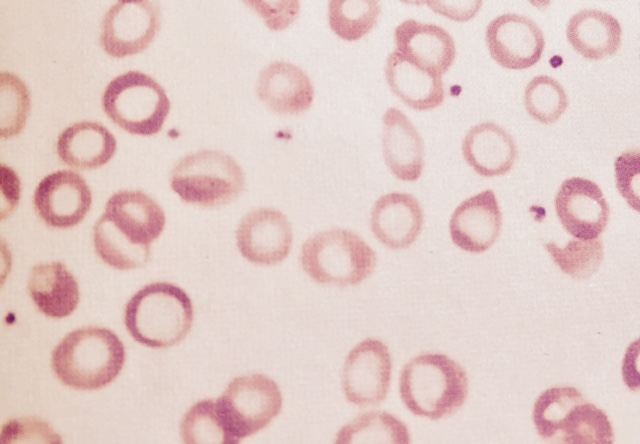
Microcytic and hypochromic anemia
- There may be leucopenia.
- The serum transferrin receptor is raised.
- Platelets count high.
- RDW is high.
- Bone Marrow shows erythroid hyperplasia, and this is polychromatic.
- Micro-normoblasts are seen.
- The cytoplasm is decreased and sometimes shows only the rim.
- Nuclei may be pyknotic.
- Erythroblast iron is absent.
- The Myeloid series is usually normal, and M: E ratio is reduced.
- Megakaryocytes are normal in number and morphology.
- The iron stain of bone marrow shows the absence of stainable iron in the reticulum cells, and normoblast looks like sideroblasts. This is a more reliable test by Prussian blue reaction.
- Micro-normoblasts are seen.
Anemia of iron deficiency and chronic diseases:
| Type of anemia | Ferritin | Serum iron | TIBC | % saturation transferrin |
| Iron deficiency anemia | Decreased | Decreased | Increased | <10% |
| Anemia of chronic diseases | Normal or increased | Decreased | Decreased | >15% |
Lab findings in iron deficiency anemia:
-
Test Result Hemoglobin Normal or low MCH Decreased MCV Decreased <80 fl MCHC Decreased RDW Increased Reticulocytes Decreased Total iron Decreased (normal =50 to 150 µg/dL) TIBC Increased (normal = 250 to 450 µg/dL) Ferritin Decreased (normal = 20 to 250 ng/mL) Transferrin receptor Increased % transferrin saturation Decreased (normal 20% to 50%) Platelet count High WBC Leucopenia Bone marrow iron store Decreased or absent Erythroblast iron Absent Free RBC protoporphyrin Increased
Summary of the lab findings of Iron-deficiency anemia:
| lab test | Lab findings |
| Blood |
|
| Bone marrow |
|
| Chemical tests |
|
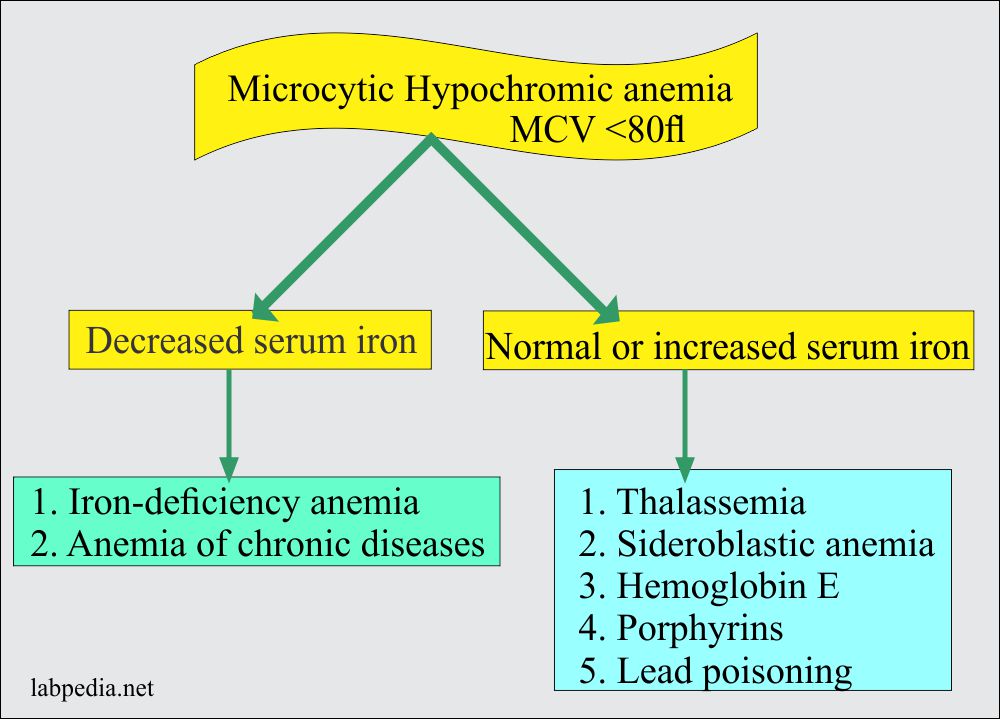
Differential diagnosis of Microcytic hypochromic anemia:
| Anemia type | MCV | Serum iron | TIBC | Ferritin | RDW | HbF | HbA2 | FEP |
| Iron-deficiency | Low | Low | High | Low | High | Normal to low | Normal | High |
| α-thalassemia | Low | High | Normal | High | High | Low | Normal | Normal |
| β-thalassemia | Low | High | Normal | High | High | High | High | Normal |
| Sideroblastic anemia | Low | High | Normal | High | High | Normal | Normal | Low |
| Chronic diseases | Low | Low | Low | High | Normal | Normal | Normal | High |
| Lead poisoning | Low | Increased | Decreased | Increased | Normal |
FEP = Free erythrocytes protoporphyrin.
TIBC = Total iron-binding capacity.
RDW = Red cell distribution width.
Important facts about iron:
- Iron deficiency and lead toxicity frequently coexist. Iron deficiency increases the toxic effect of lead.
- The quickest way to diagnose iron-deficiency anemia is serum ferritin level <10 µg/L.
- FEP (zinc protoporphyrin) is elevated in iron deficiency anemia, lead poisoning, and anemia of chronic diseases.
Questions and answers:
Question 1: What is MCV in microcytic hypochromic anemia?
Question 2: What is the value of RDW in iron deficiency anemia?

This very good and nice work, so may Allah bless you,protect your family wherever they are thanks.
Thanks for your comments.
Superb Effort Sir
Thanks for the encouragement..
I found a patients who has iron 1050 µ/dl and TIBC 902 µ/dl What is the main cause to much Iron and TIBC
There are so many possibilities.
1. Repeat serum iron.
2. High TIBC is seen in Thalassemia.
3. Patient may be on iron therapy.
4. Best advice to repeat both TIBC and serum iron.