alpha-1-antitrypsin Deficiency, (α1-antitrypsin or AAT Deficiency)
alpha-1-antitrypsin Deficiency
What sample is needed for alpha-1-antitrypsin Deficiency?
- The patient needs to fast for several hours before giving the sample.
- This test is done in the serum or plasma.
- Separate the serum immediately and store it properly.
- Take 3 to 5 ml of blood in the disposable syringe.
- Keep the syringe for 15 to 30 minutes, then centrifuge for 2 to 4 minutes. This will yield a clear serum.
- Serum or plasma is stable for ≥ 7 days at 4 °C.
- At -70 °C, it is stable for 3 months.
What are the Indications for alpha-1-antitrypsin Deficiency?
- This helps in the diagnosis of juvenile and adult cirrhosis of the liver.
- For neonatal respiratory distress syndrome.
- For emphysema (there is a deficiency or absence of this enzyme).
- This is useful for the diagnosis of familial chronic obstructive lung disease.
- This enzyme may be deficient in a protein-losing disorder.
- This is also an acute-phase protein raised in inflammation, infections, and malignancy.
What are the precautions for alpha-1-antitrypsin Deficiency?
- This is raised during pregnancy.
- Oral contraceptives increase the level of AAT.
- Any inflammatory process will raise the AAT level because it is raised by inflammation.
How will you define alpha-1-antitrypsin deficiency?
- Alpha-1-anti-trypsin deficiency is a genetic disorder that affects the production of a protein called alpha-1-anti-trypsin.
- It protects the lungs from the damage caused by an enzyme released during inflammation.
How will you discuss the pathophysiology of alpha-1-antitrypsin Deficiency?
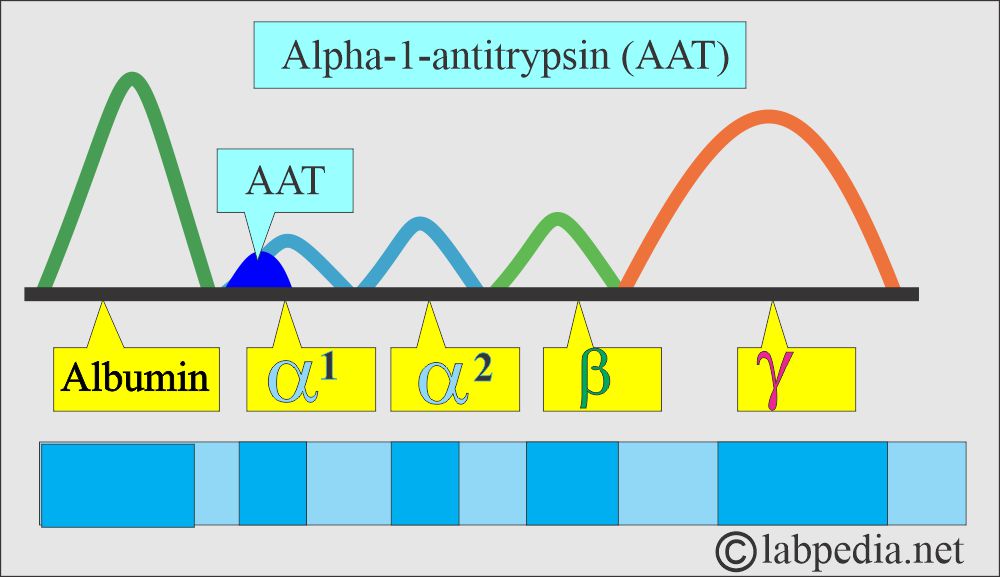
- This is present in the alpha-globulin fraction, mainly consisting of the glycoprotein.
- AAT deficiency is autosomal recessive, present on chromosome 14.
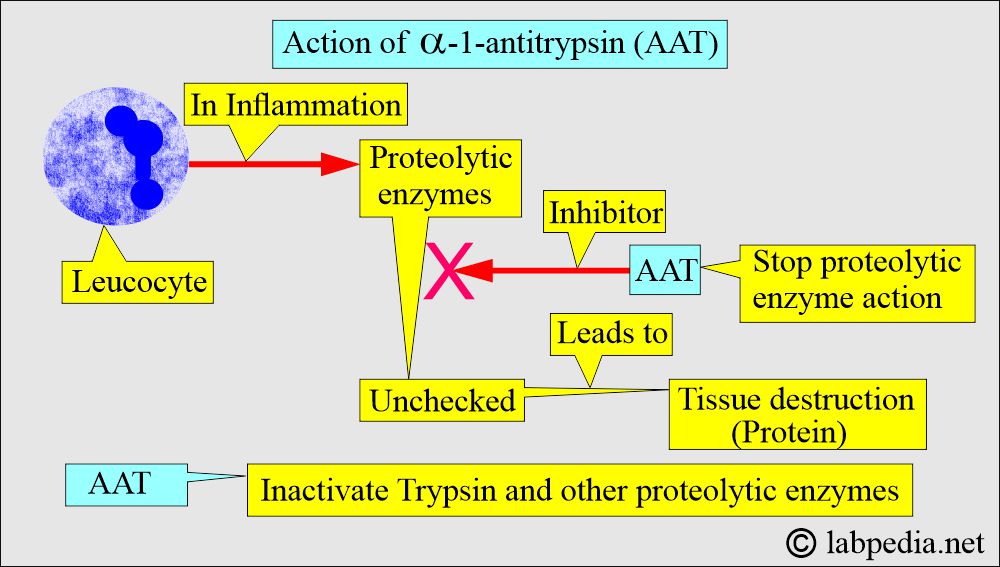
- This is a serine protease inhibitor; the main substrate is neutrophil elastase, which, when unchecked, is associated with familial pulmonary emphysema and liver diseases.
- The heterozygous state occurs in 10% to 15% of the general population, with a serum level of AAT ∼60% of the normal.
- Homozygous patients are seen in 1:2000 persons with a serum level ∼of 10% of the normal.
- AAT is a relatively small size and can diffuse into the tissues. It is important in preventing loss of elastic recoil.
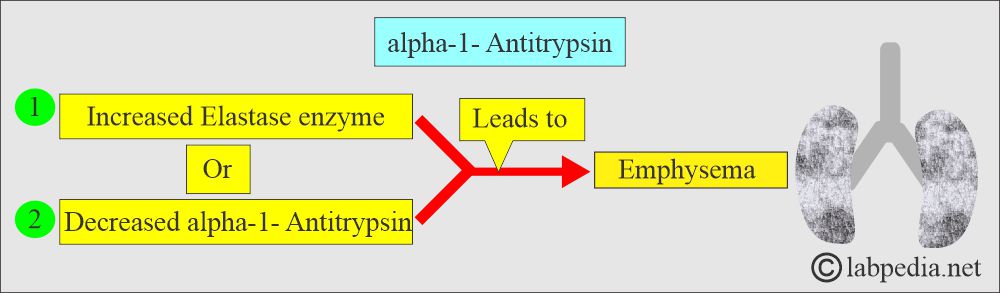
- The deficiency of AAT or excess of elastase in uninhibited elastase in the bronchial tree leads to emphysema.
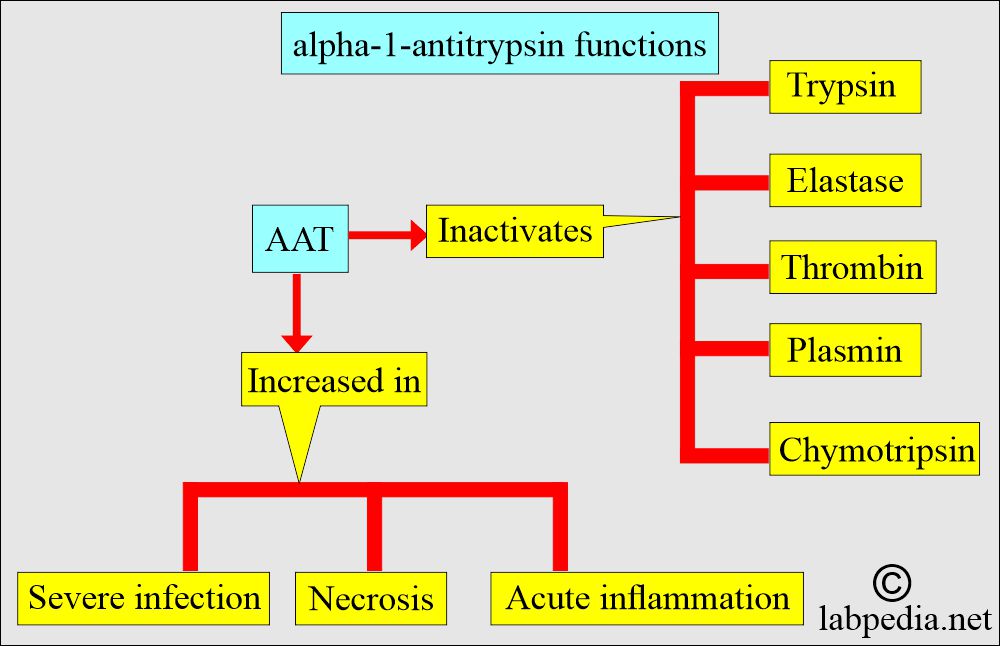
- This is the most potent protein (AAT), which inhibits proteolytic enzymes produced by neutrophils during inflammation and the phagocytic process.
- This is also called an α-1 proteinase inhibitor.
- AAT is the highest concentration proteinase inhibitor in the plasma on a molar basis.
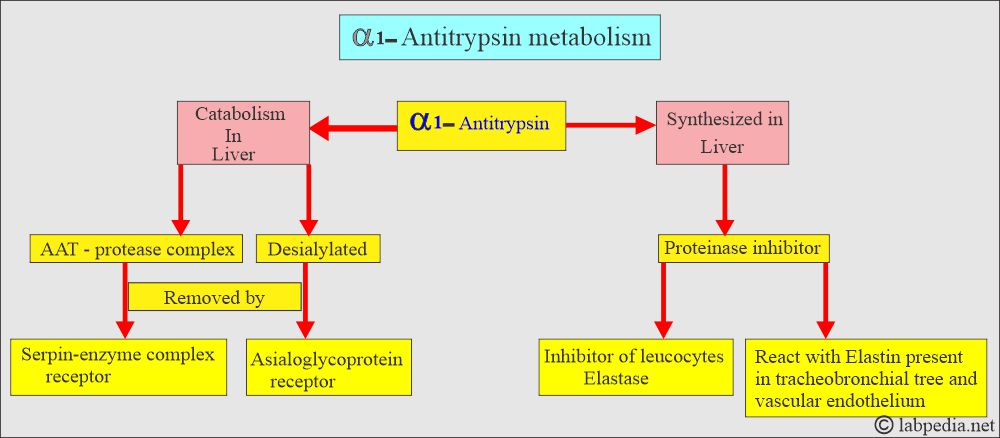
- This is the most important inhibitor of the leucocyte elastase, which is produced in inflammation for phagocytosis.
- This enzyme reacts with elastin in the tracheobronchial system and the vascular endothelium.
- This is synthesized in the liver by hepatocytes.
- Catabolism is also taken by the liver parenchymal cells. This takes two routes:
- The serpin-enzyme complex receptor removes the AAT-protease complex.
- The asialoglycoprotein receptors remove desialylated AAT.
- It breaks enzymes like Trypsin, Chymotrypsin, Elastase, Thrombin, and Plasmin.
- Its level rises non-specifically in acute inflammations, severe infections, and necrosis.
What is the etiology of α1-Antitrypsin Deficiency?
- Genetic.
- Acquired.
- There are 75 known variants of the AAT, some of which are associated with a low concentration of AAT.
- Pi MM’s most common phenotypes and the most common deficiency of phenotypes are Pi ZZ and Pi SZ.
- Its deficiency gives rise to lung and liver diseases.
- This enzyme protects the lungs from the elastase enzyme action.
- Acquired deficiency may be seen in protein deficiency, such as malnutrition, liver diseases, Nephrotic syndrome, and neonatal respiratory distress syndrome.
What is the clinical presentation of the Alpha-1-antitrypsin deficiency?
- People with a1a (AAT) deficiency develop emphysema in the 3rd or 4th decades of life.
- Congenital deficiency of ATT results in premature emphysema.
- An inherited AAT deficiency is associated with symptoms in early life, unlike the acquired AAT deficiency.
- Inherited AAT deficiency is associated with liver and biliary diseases.
- Homozygous people have severe pulmonary and liver disease very early in life.
- 5% to 14% of the adult population is in the heterozygous state and is considered at greater risk for developing emphysema.
- Chronic bronchitis is prominent with a1a (AAT) deficiency who smoke.
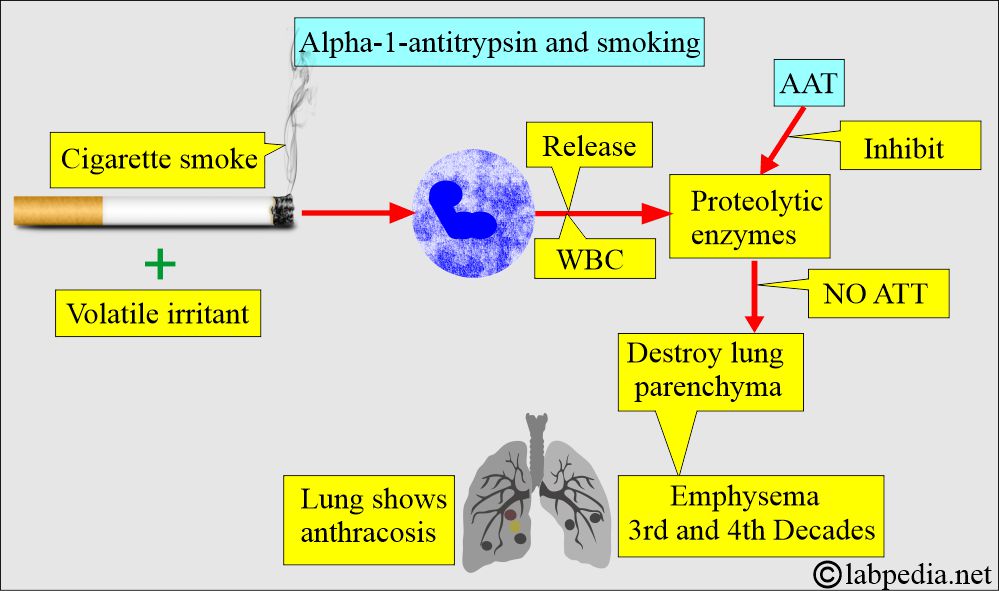
- Cigarette smoking and other volatile irritants stimulate the release of enzymes from the white blood cells in the lung.
- Without the presence of ATT, these enzymes destroy the lung parenchyma.
- There will be Severe emphysema, usually seen in the 3rd or 4th decades.
- This is a positive acute-phase protein.
- This enzyme deficiency is an inherited disorder that gives rise to liver and lung diseases.
- There are 75 known genetic variants of AAT associated with deficiency.
- The most common phenotype is Pi MM, and the deficiency of AAT is Pi ZZ and SZ.
- The congenital decrease may cause the early onset of:
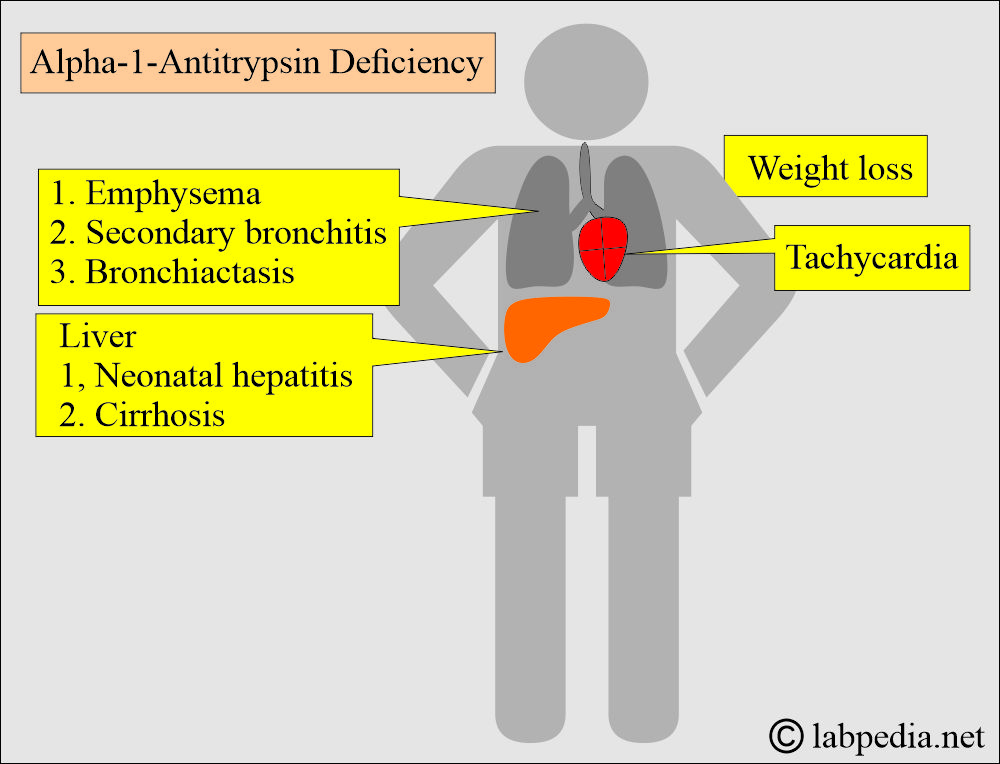
- Emphysema.
- Infantile hepatitis ultimately leads to cirrhosis.
- Neonatal cholestasis or hepatitis is present most commonly at 3 to 8 weeks of age.
- Extrahepatic and intrahepatic bile ducts may be small because of decreased bile flow.
- Hepatocellular carcinoma.
- This is inherited as an autosomal codominant trait.
- There is a mutation in the gene SERPINA1.
- There are two common diseases, emphysema and liver cirrhosis.
- This is also seen in liver diseases like:
- Neonatal cholestasis or hepatitis is common at the age of 3 to 8 weeks and regresses after a few weeks.
- Differentiation from the biliary atresia is significant.
- Because there is very high mortality if surgery is done in patients with Pi ZZ infants.
- Cirrhosis.
- Hepatocellular carcinoma.
- Neonatal cholestasis or hepatitis is common at the age of 3 to 8 weeks and regresses after a few weeks.
What is the presentation of the Alpha 1-Antitrypsin Deficiency?
- There is tiredness.
- Patients have shortness of breath and wheezing.
- Pulmonary emphysema is seen in heterozygotes and homozygotes.
- Secondary bronchitis and bronchiectasis may be seen in these patients.
How will you diagnose Alpha-1-antitrypsin deficiency?
- This disease can be diagnosed:
- Estimation of a1-antitrypsin in the blood.
- Genetic analysis (Genotype or phenotype of the blood).
- A sample of DNA from the mouth cell to detect α1-antitrypsin.
- Routine serum protein electrophoresis is a good screening test for AAT deficiency.
- 90% of the AAT is in the α1-globulin portion.
What are the normal alpha-1-antitrypsin levels?
|
|
|
|
|
|
Source 2
- Normal = 85 to 213 mg/dL (0.85 to 2.13 g/L).
Source 4
- 100 to 200 mg/dL (18.4 to 36.8 µmol/L) by nephelometry.
- The critical value for deficiency = is around 35 mg/dL
- The patient with serum AAT <70 mg/dL (<12.9 µmol/L) may have a homozygous deficiency and risk developing early lung disease.
What are the causes of raised alpha-1-antitrypsin Deficiency (AAT)?
- Inflammatory disorders.
- Cancers, especially cervical carcinoma and lymphomas.
- Hormonal effects.
- Systemic lupus erythematosus.
- Brain infarction.
- Hashimoto’s thyroiditis.
- Pregnancy.
- Oral contraceptive tablets.
What are the causes of decreased alpha-1-antitrypsin Deficiency (AAT)?
- Typically <50 mg/dL.
- Kidney diseases like Nephrotic syndrome.
- Prematurity.
- Malnutrition.
- Liver diseases like acute hepatitis.
- In the lungs as respiratory distress syndrome and Emphysema.
- Protein-losing gastroenteropathies.
- Pancreatitis.
- Congenital defects.
- AAT levels are secondarily low in patients like:
- Neonatal respiratory distress syndrome.
- Severe pancreatitis.
- Protein-losing disorders.
Questions and answers:
Question 1: What is the role of cigarette smoking in alpha-1-deficiency?
Question 2: AAT deficiency on which chromosome is present?