ACTH (Adrenocorticotropic Hormone), Cushing’s Syndrome
ACTH (Adrenocorticotropic Hormone)
What sample is needed for Adrenocorticotropic Hormone (ACTH)?
- The Patient’s plasma is needed.
- Place blood immediately in ice water and freeze plasma for 15 min.
- The sample should be collected in a prechilled plastic test tube with EDTA or heparin.
- Transfer the sample immediately to the lab on ice.
- For the diagnosis of Cushing’s syndrome, the sample should be taken between 6 to 11 pm.
- Centrifuge the sample at 4 °C and store it at -20 °C immediately within 15 minutes of collection.
What are the precautions for Adrenocorticotropic Hormone (ACTH)?
- A stressful collection of blood will raise the level.
- Stress, mental or physical, and obesity can increase the value.
- Ask the patient to relax and reduce environmental stress.
- Avoid physical activity 10 to 12 hours before taking the sample.
- Physical activity increases the value.
- Ask the patient not to eat or drink after midnight on the night before samples are taken.
- Stop medication like corticosteroids 48 hours before this test.
- Collect the sample in a chilled plastic vial with EDTA or Heparin.
- ACTH is very labile and requires antiprotease in the collecting vial.
- The ACTH level is not measured in the routine because it degrades in the plasma.
- Put the patient on a low-carbohydrate diet.
- Oral contraceptives can decrease their value.
- Glucocorticoids and estrogen decrease the value.
- Blood glucose interferes with the accurate value.
- A radioactive scan within one week of the test will interfere with accurate results.
What are the Indications for Adrenocorticotropic Hormone (ACTH)?
- This hormone is estimated in various conditions like Adrenal insufficiency, Cushing’s syndrome, and Acromegaly.
- For the diagnosis of Addison’s disease (level is>1000 pg /ml).
- Its level decreases in Secondary Adrenocortical Insufficiency, Adrenal carcinoma, and adenoma.
- This is the test of the anterior pituitary gland.
How will you define adrenocorticotropic hormone (ACTH)?
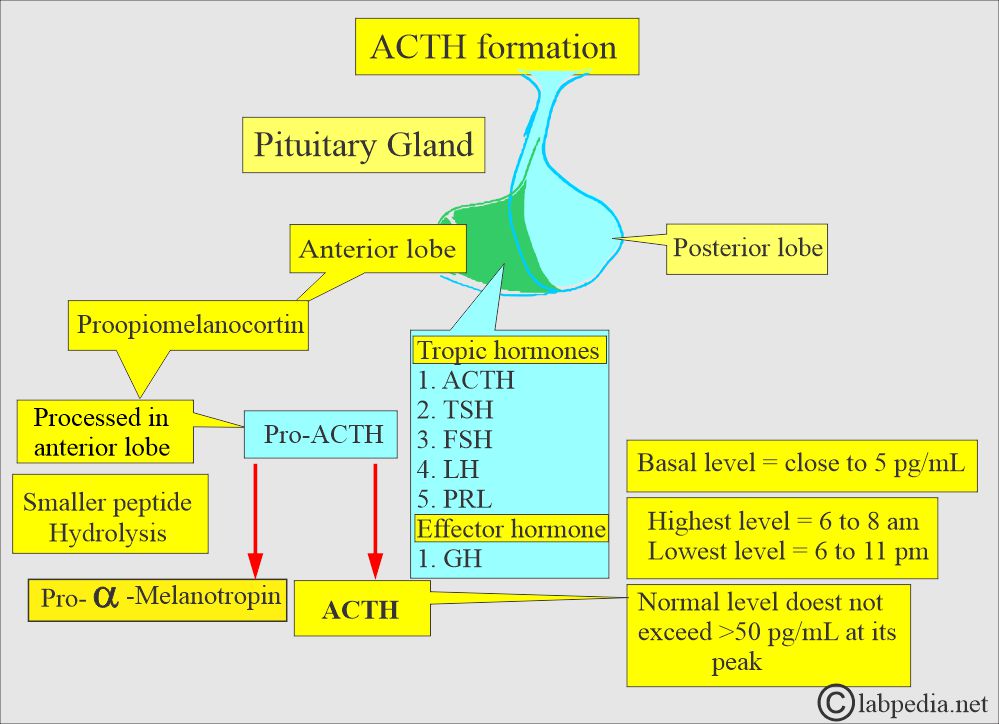
- Adrenocorticotropic hormone (ACTH) is a peptide hormone produced and secreted by the anterior pituitary gland.
- Its primary functions are:
- Stimulate adrenal glands to produce and secrete cortisol.
- Cortisol is a glucocorticoid hormone that plays an important role in metabolism, immune response, and stress.
- The anterior pituitary gland is considered the master gland due to the many hormones secreted by this gland.
- The hormones secreted are TSH (Thyrotropin), ACTH, and reproductive hormones like FSH, LH, and many others.
What are the anterior pituitary lobe hormones?
| Hormone | Chemical nature | Target organ | Main function |
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
What are the main functions of the Adrenocorticotropic Hormones (ACTH):
- These hormones maintain a constant internal environment in the body fluid, leading to homeostasis.
- It will regulate the growth and development of the body as a whole.
- It will regulate energy production and stabilize the metabolic rate (system).
- It will help the body to adjust to a stressful or emergency state.
- It will promote sexual maturation, maintain the sexual rhythm, and help the reproductive process.
- Summary of the ACTH hormone functions:
- Stimulate cortisol production.
- It regulates the body’s stress response.
- It maintains blood pressure.
- It maintains body metabolism.
What is the ACTH hormone solubility?
- Hormones that are soluble in plasma are from:
- Hypothalamus.
- Anterior and posterior pituitary.
- Pancreas.
- Parathyroid.
- Hormones that are poorly soluble in plasma and will need plasma proteins as a carrier are from:
- Adrenal cortex.
- Gonads.
- Thyroid.
- Pituitary glands consist of:
- Anterior lobe (adenohypophysis).
- Posterior lobe (neurohypophysis).
Adrenocorticotropin hormone (ACTH):
What is the significance of the Adrenocorticotropin hormone (ACTH)?
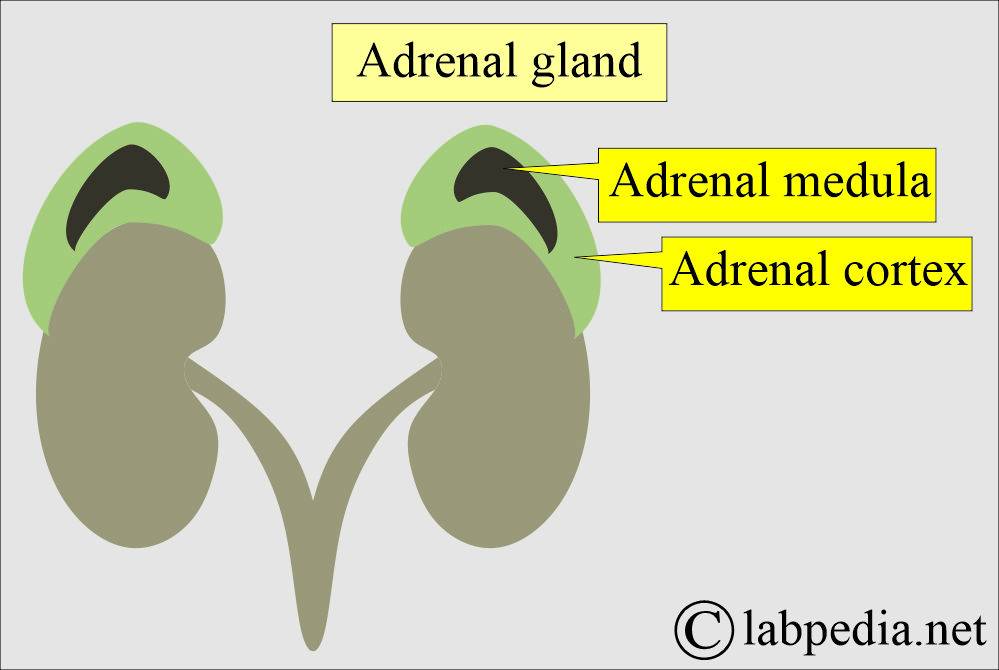
- The adrenal gland is present at the upper pole of the kidneys.
- It consists of the adrenal cortex and adrenal medulla.
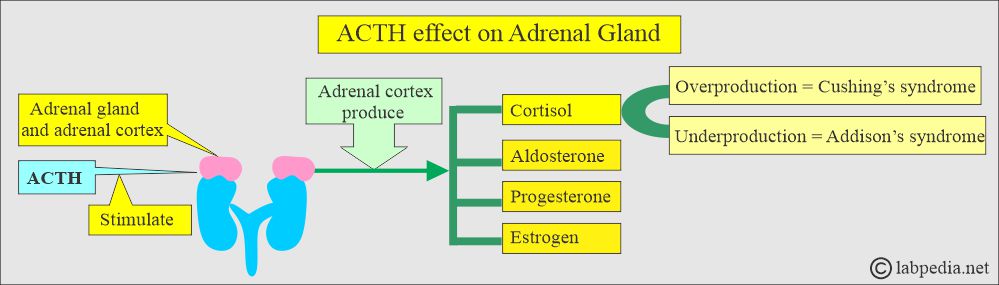
- ACTH is a tropic hormone. It is a long-chain polypeptide that binds to adrenal cortex cells and influences their activities.
- ACTH is a 39 amino acid peptide hormone secreted by the anterior pituitary gland.
- The anterior pituitary hormones are produced in a pulsatile pattern.
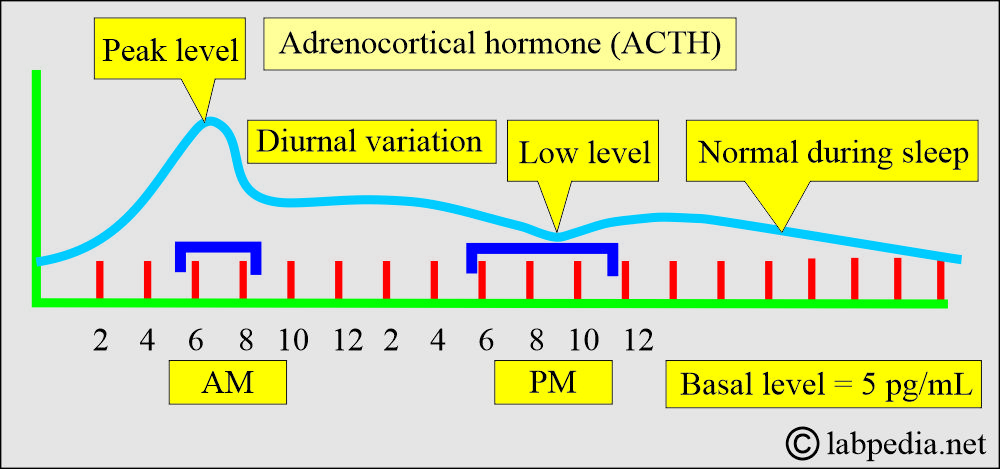
- Basal level = close to 5 pg/mL.
- Highest level = 6 to 8 A.M.
- Lowest level = 6 to 11 P.M.
- The plasma level of ACTH does not exceed 50 pg/mL.
- Anterior pituitary hormones are either tropic, which means their action is specific for another endocrine gland, or are direct effectors because they act directly on the peripheral tissue.
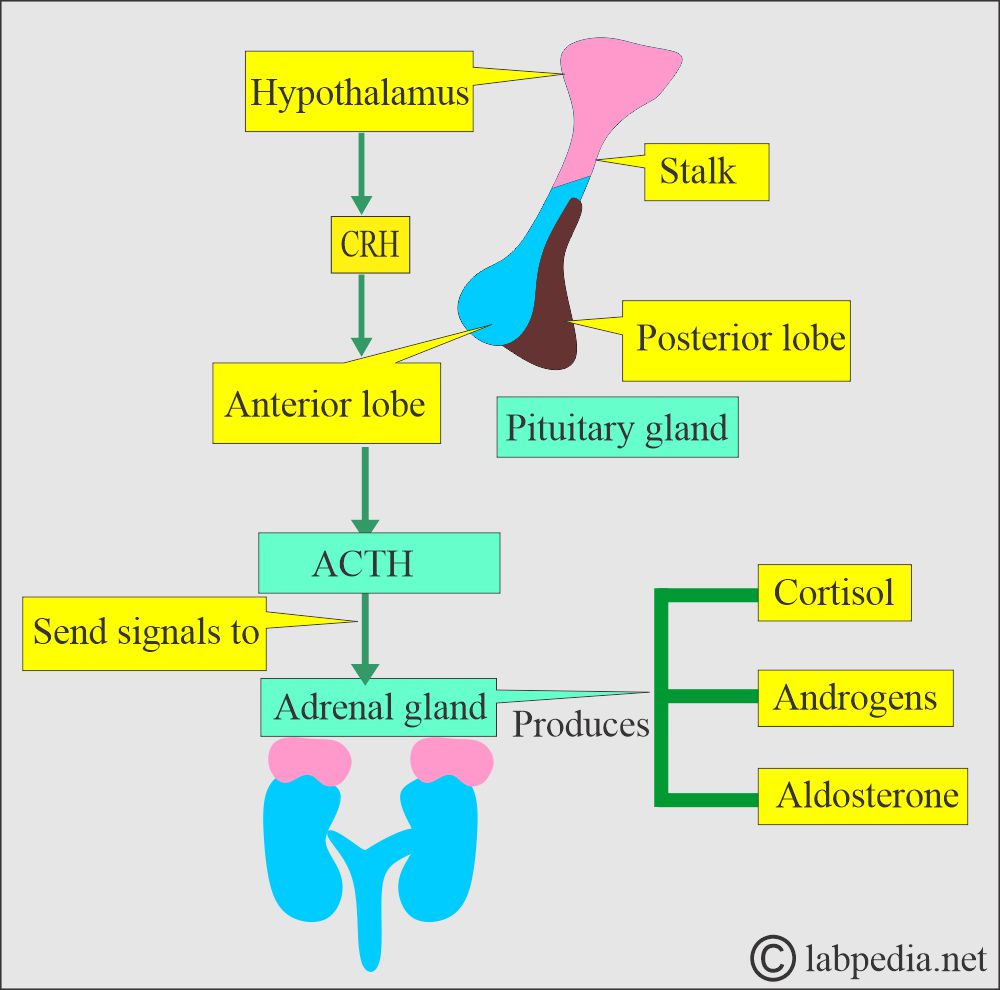
- Corticotropin-releasing hormone (CRH) is made and released from the hypothalamus, giving rise to ACTH release from the pituitary glands.
- CRH stimulates ACTH production in the anterior pituitary gland.
- Now, ACTH sends signals to the adrenal gland (cortex), which secretes steroids (cortisol, androgen, and aldosterone).
- The rising cortisol level is a negative feedback mechanism that stops CRH and ACTH production.
What are the peaks of adrenocorticotropic hormone (ACTH) secretion?
- ACTH is released in a burst, so its level can vary from minute to minute.
- Highest between 6 to 8 AM.
- The lowest level is between 9 to 10 (6 to 11) PM.
- During sleep, it is at the normal level.
- Pregnancy, menstrual cycle, and stress increase secretion.
- ACTH is released in response to many stresses.
- ACTH is advised for investigating disorders of the hypothalamic, pituitary, and renal systems.
- ACTH is secreted by the anterior pituitary gland, which signals the adrenal gland to produce steroids (androgens, cortisol, and aldosterone). These are needed for the body’s normal functioning.
- With adrenal insufficiency, the pituitary gland releases proopiomelanocortin, increasing ACTH.
- ACTH is unstable in the blood. Most commercial RIA kits are insensitive and nonspecific when measuring ACTH.
What is the normal Adrenocorticotropic Hormone (ACTH)?
Source 2
- 6 to 8 a.m = <80 pg / mL or <18 pmol /L (SI units).
- 6 to 11 p.m = <50 pg /mL or <11 pmol /L (SI units).
- or less than 120 pg/ml
Another reference gives the following values:
- 8 AM ( unrestricted activity) = <120 pg/mL
- 4 to 8 PM <85 pg/mL
- Cord blood = 50 to 570 pg/mL
- Newborn = 10 to 185 pg/mL
Another reference gives the following values:
Adults, Adolescents, children, and elders
- 8 A.M. fasting = 15 to 100 pg/mL (10 to 80 ng/L)
- 4 P.M. nonfasting = 10 to 50 pg/mL (10 to 50 ng/L)
- Newborn = 10 to 185 pg/mL
Cushing’s Syndrome
How will you define Cushing’s syndrome?
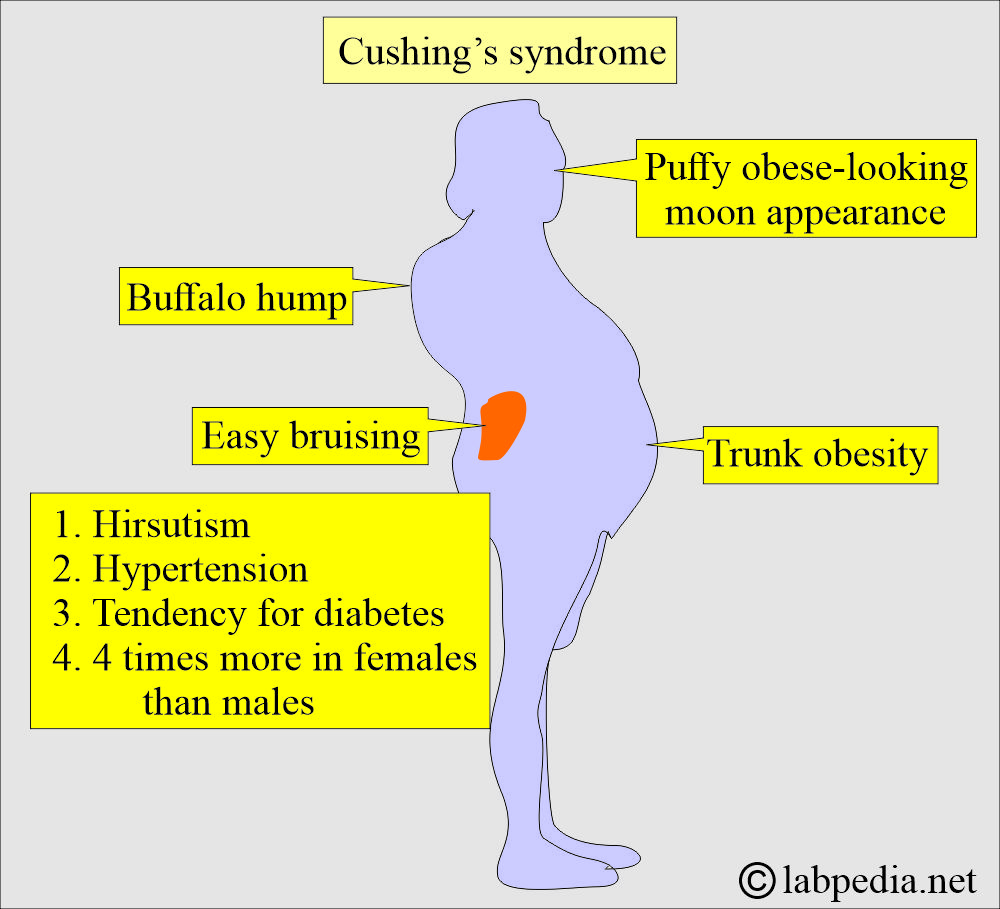
- Cushing’s syndrome is named after the name of Dr. Harvey Cushing, who was the surgeon.
- Cushing’s syndrome is a hormonal imbalance caused by prolonged exposure to increased cortisol levels.
- Cushing’s syndrome may be caused by:
- Endogenous overproduction of cortisol by the adrenal glands.
- Exogenous when there is overuse of corticosteroids.
What are the causes of Cushing’s Syndrome?
- As a result of treatment with corticosteroids, this is the nonadrenal cause.
- Secondary to a benign hormone-secreting pituitary adenoma. These are ACTH-secreting adenomas (68%).
- Cortisol production from the adrenal tumors or nodules (17%).
- Excess ACTH ectopic production (15%). Mostly, there are malignant tumors.
- Chronic alcoholism, stress, and obesity.
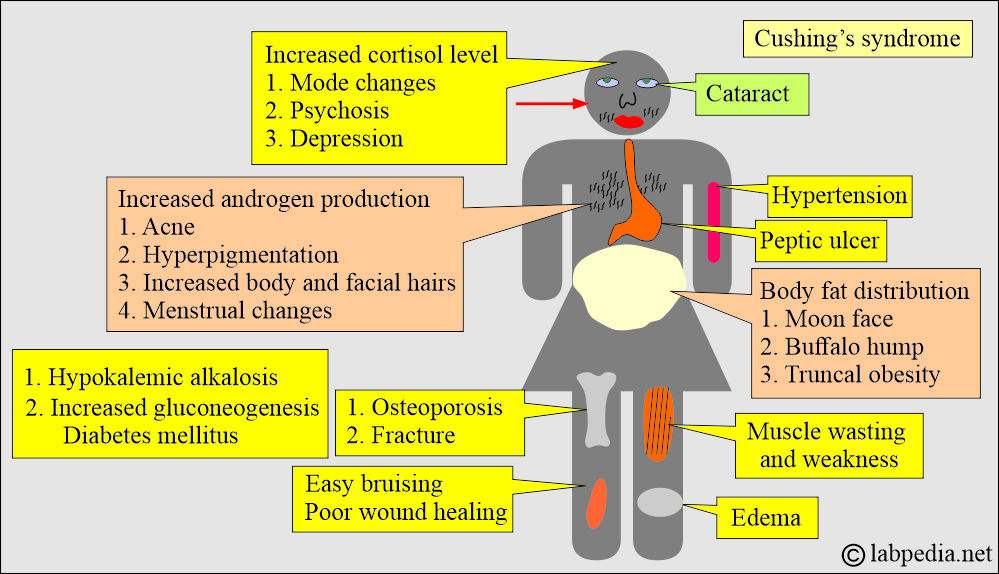
What is the clinical presentation of Cushing’s syndrome?
- This may be a form of Hyperadrenalism or Hypercortisolism with common clinical presentations.
- These patients have similarities like diabetes mellitus type 1 (insulin resistance).
- There are 4 times increased mortality even after successful treatment.
- Patients have cardiovascular diseases. There is left ventricular hypertrophy.
- There are changes in the ECG and nocturnal hypotension.
- Blood pressure changes were seen in 85% to 90%.
- Central obesity is seen in 90%.
- Glucose intolerance is seen in 80%.
- Hirsutism is seen in 65%.
- There are abnormal menses by 60%.
- There may be muscle weakness in 60%.
- Untreated cases have a 50% mortality for 5 years.
How will you diagnose Cushing’s syndrome?
- The abnormal Overnight Dexamethasone suppression test and 24-hour urinary cortisol test are diagnostic of Cushing’s Syndrome.
- The free urinary cortisol level (24-hour sample) is the most sensitive, 95% to 100%, and specificity is 98%.
- Random plasma cortisol level is of little value for diagnosing Cushing’s syndrome.
- There is a loss of diurnal rhythm because late-night values remain high.
- The ideal time for collecting ACTH and cortisol is between 11.00 p.m. and 12.00 a.m.
- A single midnight serum sample concentration >7.5 µg/dL is diagnostic of Cushing’s syndrome with a sensitivity of 90% to 96% and specificity of 100%.
- The salivary cortisol level at 11.00 p.m., when combined with the 8.00 a.m. salivary cortisol concentration after the 1 mg overnight dexamethasone suppression test, had a sensitivity and specificity of 100%.
- Radiological work-up:
- Adrenal gland CT distinguishes hyperplasia vs. tumor.
- Adrenal MRI distinguishes the carcinoma.
- Pituitary CT diagnoses 85% of microadenoma.
- CT scan finds ectopic ACTH sources like bronchial adenoma, medullary thyroid carcinoma, and squamous cell carcinoma.
- The ACTH level is high when Cushing’s syndrome is due to a Pituitary or ectopic source.
- When the source is the Adrenal gland, the ACTH is low.
How will you differentiate between Cushing’s syndrome and Addison’s disease?
| Disease | ACTH value | Cortisol value |
|---|---|---|
| Cushing’s syndrome |
|
|
|
|
|
|
|
|
|
|
|
|
|
|
| Addison disease | ||
|
|
|
|
|
|
|
|
|
What are the causes of increased ACTH levels?
- Addison disease (primary adrenal insufficiency).
- Ectopic ACTH syndrome.
- Cushing’s syndrome. This is dependent upon adrenal hyperplasia due to the pituitary gland.
- Stress.
What are the causes of decreased ACTH levels?
- Hypopituitarism.
- Secondary adrenal insufficiency is due to pituitary insufficiency.
- Adrenal adenoma or cancer.
- Exogenous steroid administration.
What is the value of ACTH for the Layman?
- This test is advised if the patient has diabetes mellitus, reduced glucose tolerance, and muscle wasting to rule out Cushing syndrome.
- If there are truncal obesity and thin extremity.
- In case of abnormal lipid metabolism.
Questions and answers:
Question 1: What is the basic mechanism of Cushing's syndrome?
Question 2: What is the source of ACTH?