Chapter 14: Hypersensitivity Reaction Type IV, Cell Mediated Delayed Reaction
Type – IV DELAYED OR CELL MEDIATED HYPERSENSITIVITY REACTION (CMI)
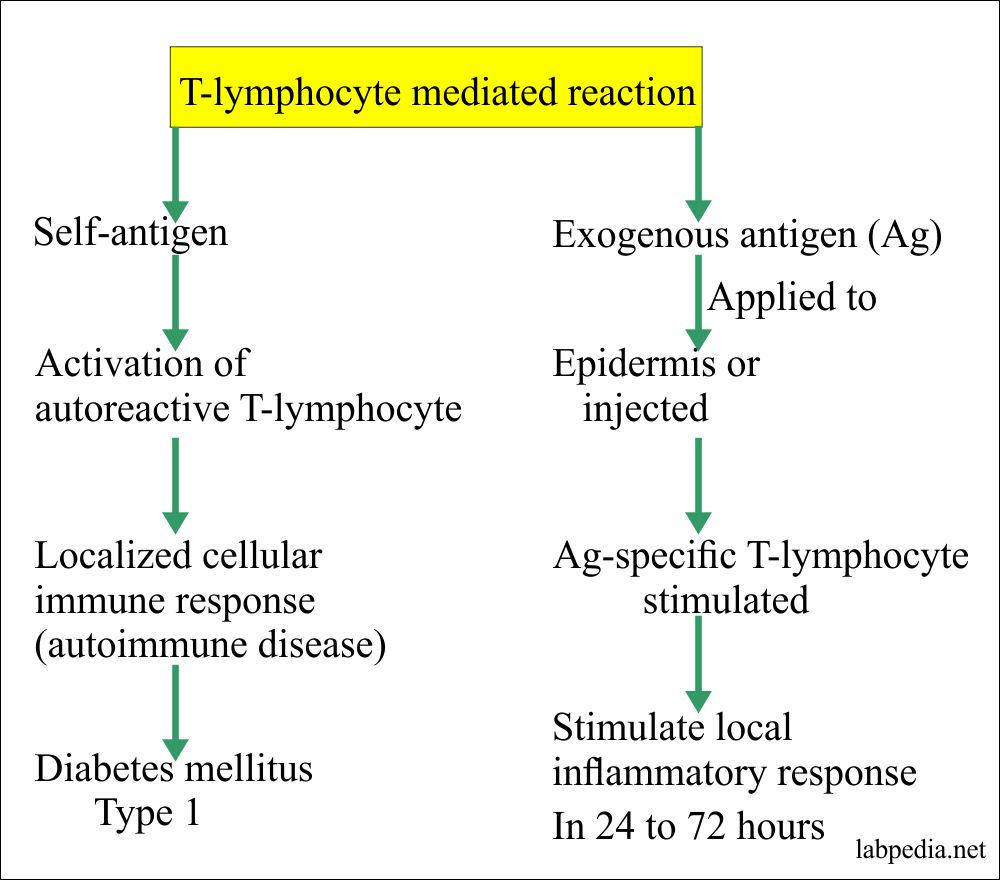
In Type-IV Hypersensitivity, there is no role of Ab and no role of complement.
This is mainly dependant on T-lymphocytes activity.
Definition
According to Coombs and Gel, type IV or delayed hypersensitivity reactions occur in more than 12 hours to develop and involve cell-mediated immune response (through T-lymphocytes). They are not dependant upon the antibody formation.
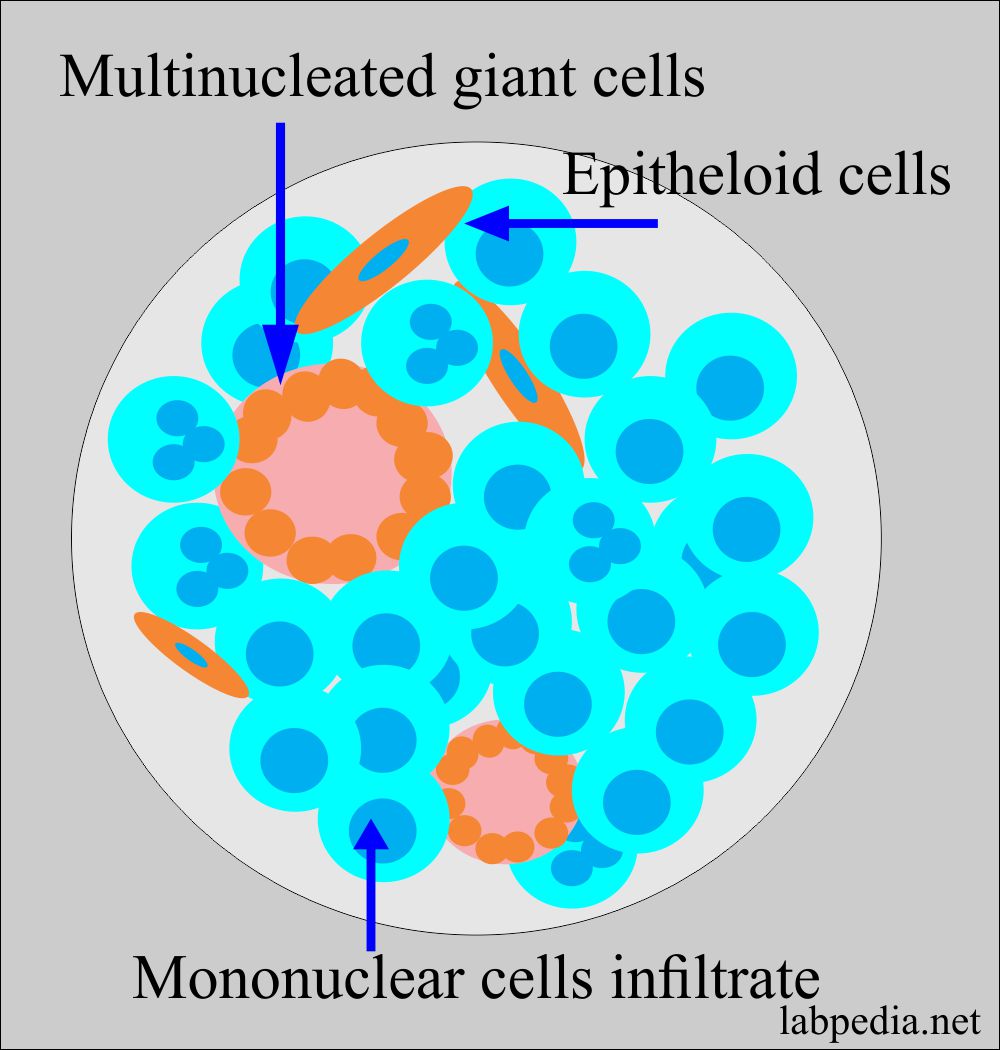
Type – IV reaction is characterized by cellular infiltrate, composed mainly of lymphocytes and macrophagic cells. This inflammatory infiltrate appears at least 24 hours after the challenge with the provoking stimulus. The macrophagic cells in this lesion frequently fuse to form giant cells and epitheloid cells.
- This reaction can not be transferred from one animal to another by the serum but can be transferred by T-lymphocytes (T-L), particularly by T-helper cells CD4+ (TH1 cells).
This reaction is mostly due to organisms that grow in the cell and resists killing, e.g., T. bacilli, viruses, and fungus.
This reaction may take place by the Single Antigen (Ag) challenge.
Abbreviations used are:
| Abbreviation | Actual name |
| IL | Interleukin |
| IFN | Interferon |
| TNF | Tumor necrosis factor |
| TGF-α | Transforming growth factor – α |
| TGF-β | Transforming growth factor-β |
| GF | Growth factor |
| CSF | Colony-stimulating factor |
| ICAM-1 | Intercellular adhesion molecule |
| GM-CSF | Granulocyte-macrophage colony-stimulating factor |
| M-CSF | Macrophage-colony stimulating factor |
Classification of a delayed cell-mediated hypersensitivity reaction:
The delayed reaction may be divided into the following four categories and Reaction appearing within 72 hours.
- Jone- Mote phenomenon: – This reaction appears within 24 hours. Peak 1-6 days. There is swelling of the skin. Microscopic examination shows the presence of basophils predominantly.
- Contact hypersensitivity reaction: – The sensitization takes 10 to 14 days.
- This reaction appears after contact with Ag, and the peak reaction is at 48-72 hours (first sensitization is needed).
- Clinically the picture is like eczema. Antigens can react to, e.g., Nickle, Chromate, Rubber industry, and poison IVY.
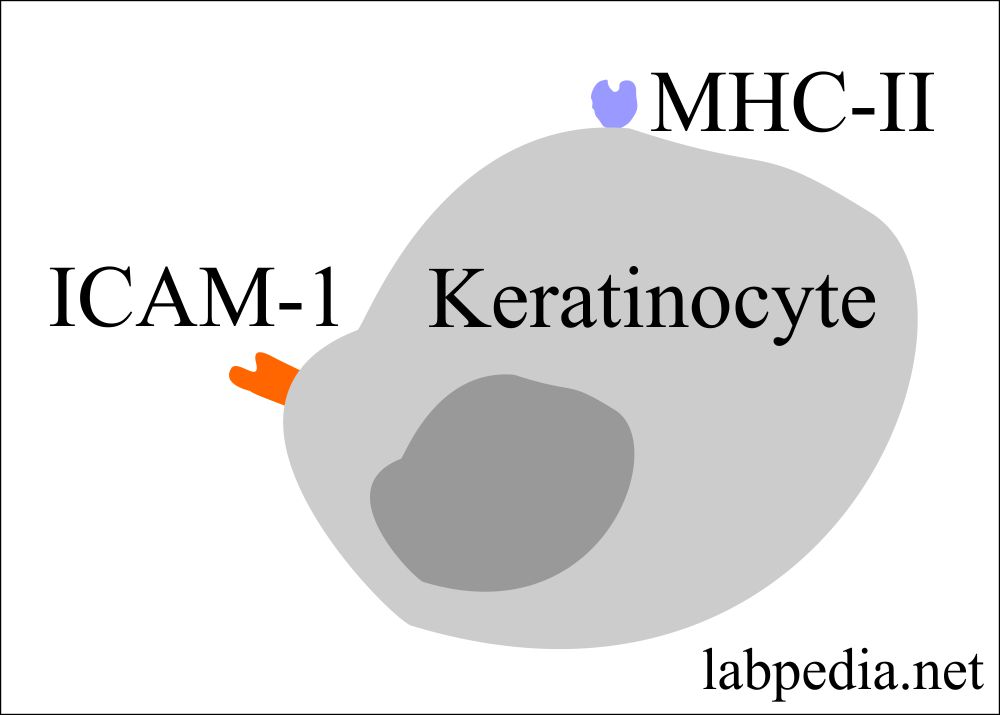
- Keratinocytes, when stimulated then they produce cytokines:
- IL-1
- IL-3
- IL-6
- IL-8
- GM-CSF
- M-CSF
- TNF-α
- TGF-α
- Keratinocytes have in their cell membrane the presence of:
- MHC-II molecule
- Intercellular adhesion molecule-1 (ICAM-1)
- The reaction wanes after 48 to 72 hours. Suppression of this reaction takes place by different cytokines produced by the macrophagic cells and keratinocytes like:
- PGF will inhibit IL-1 and IL-2 production.
- Migratory inhibition lymphokines prevent the spread of the inflammatory processes.
- TGF-β from the dermal mast cells activated keratinocytes and lymphocytes, inhibit the inflammation and block the proliferative effect of the IL-1 and IL-2.
- Microscopically there are lymphocytes infiltrate with the presence of macrophagic cells accompanied by edema. Microvesicles may be seen in the epidermis.
- Tuberculin hypersensitivity: – This reaction was first described by Robert Koch, where Purified protein derivatives (PPD) were injected subcutaneously.
- The patient developed a fever and generalized signs and symptoms.
- The reaction peak appears after 48 to 72 hours. This reaction gives the status of previous sensitization. There is local induration at the site of injection.
- Microscopically there are lymphocytes, and macrophagic cells infiltrate.
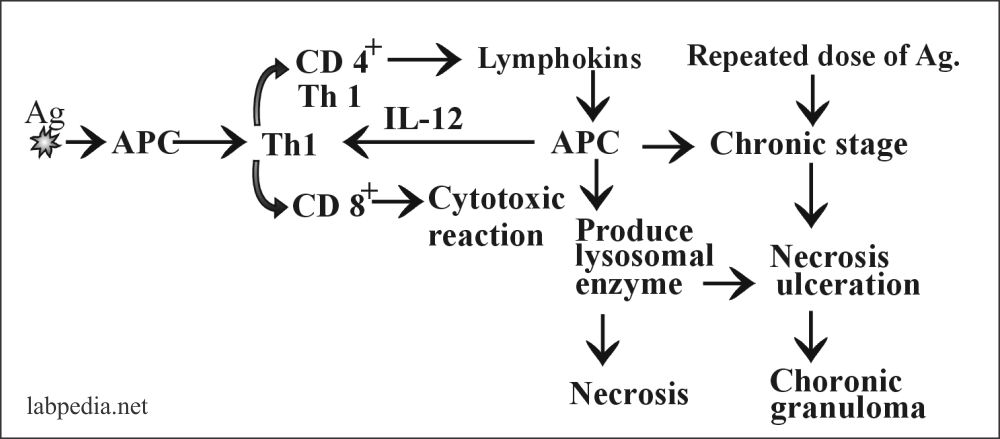
Summary of the tuberculin hypersensitivity reaction:
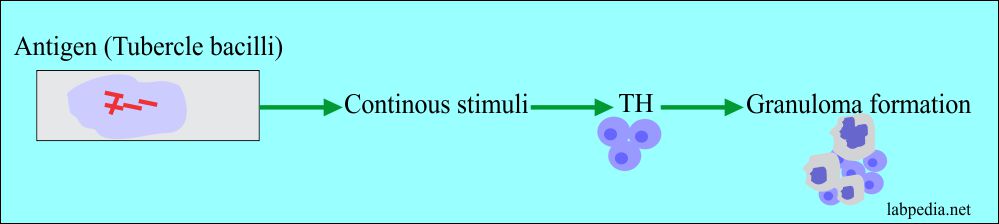
- Granulomatous type:- This is a more serious condition. This is the most important type of type IV hypersensitivity reaction and causes many pathological effects, depending upon the T-lymphocytes immunity.
- It results from the persistence of the intracellular microorganisms in the macrophagic cells or other agents that cannot be destroyed by these cells.
- Rarely by the immune complexes seen in allergic alveolitis.
- The result is epithelioid cell granuloma formation.
- Its peak level is seen after at least 14 days. Skin shows induration and even sometimes ulceration. This may be due to tuberculosis or chemical like talc.
- Microscopic appearance:
- There is the presence of typical epithelioid cells. These are the large and flattened cells with the increased endoplasmic reticulum.
- These are derived from the activated macrophagic cells under the chronic stimulation of cytokines; they continue to secrete TNF and thus continue the inflammation.
- Giant cells are formed by the fusion of the epithelioid cells to give multinucleated giant cells; these may be referred to as Langerhan’s giant cells.
- The multi nuclei are not in the center of the cells.
- There is the little endoplasmic reticulum.
- Lysosomes are undergoing degeneration.
- So the giant cells represent the terminal differentiation stage of the monocytes/macrophagic cells.
- In tuberculosis, there is a central area of necrosis.
- Lymphocytes surround Epitheloid/macrophagic cells. There is fibrosis caused by the proliferation of fibroblast and increased collagen synthesis.
Type IV hypersensitivity reactions and their appearance:
| Type of reaction | The maximum time for the reaction to appear |
| Contact hypersensitivity | 48 to 72 hours |
| Tuberculin | 48 to 72 hours |
| Granuloma formation | 21 to 28 days (peak level is after at least 14 days) |
| Jone – Mote phenomenon | Appears within 24 hours and peak 1 to 6 days |
Robert Koch’s Phenomenon
This phenomenon was first observed in 1810 by Jenner in response to cowpox reinoculation and was later developed by Koch and Von Pirquet in response to tuberculosis.
Robert Kock in (1843 -1910) injected Tubercle bacilli into Rabbit. The rabbit developed signs and symptoms after 2 – 3 weeks as follows:-
- Fever.
- Enlargement of lymph nodes.
- Enlargement of the liver.
- Local ulcer.
- Healing took 4 – 6 weeks.
- A localized hardening and swelling develop at the site of injection.
When later on, this immunized Rabbit was exposed to tuberculous bacilli. He showed only induration after 24 hours, and peak reaction was between 48 to 72 hours.
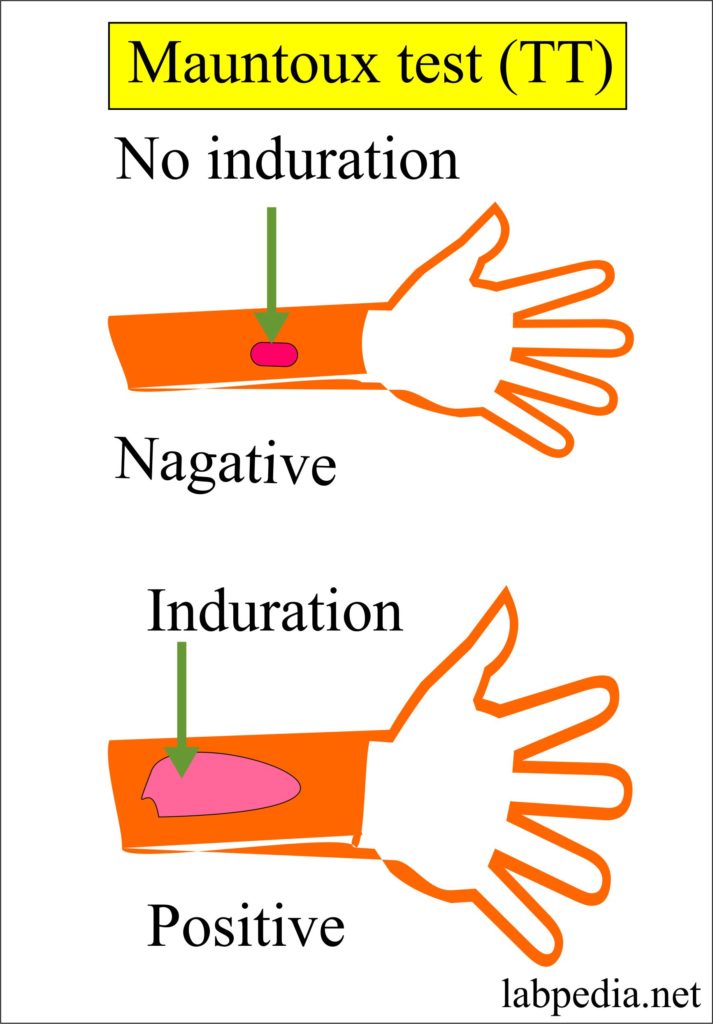
Mantoux Test or Tuberculin Test (TT)
This test is based on Robert Koch’s phenomenon. It gives an idea of immunization or the status of immunization and the possibility of active tuberculous disease.
Procedure
- Tuberculin (PPD = 0.1 mL)) is injected intradermally. The reaction appears after 4 to 8 hours, and the peak is 48 to 72 hours.
- Read the result between 48 to 72 hours.
- Initially, there is erythema and neutrophil infiltration. This is followed by mononuclear cells (lymphocytes and macrophage) infiltrate, causing induration at the injection site.
Results
- Induration (palpable, hard, swelling, raised area), 5-10 mm is positive.
- Ignore the reading area.
- A positive result means that the person has previous exposure to tuberculous bacilli or has a history of immunization.
Grading of the tuberculin test:Induration of 5 mm or more Induration of 10 mm or more Induration of 15 mm or more - HIV patients
- Recent contact with an active case of TB
- Patient with prior H/O TB
- Patient with organ transplantation
- Patient with immunosuppressant therapy
- People from the high prevalent area
- Drug addicts who inject themselves
- Residents and employees of a high-risk area
- Laboratory worker handling TB culture
- Children <4 years of age
- Infants, children, and adults exposed to the high-risk group
Considered positive in any type of person, without any known risk factors
- Negative means = There is no history of previous exposure to tuberculosis.
- False-positive = There may be a false-positive reaction in patients on cortisone therapy.
False-positive results are seen in:
- Previous BCG vaccination.
- Incorrect interpretation of the result.
- Infection with nontuberculous mycobacteria.
- The bad technique of the test performed.
- An incorrect antigen is used.
- patients on cortisone therapy.
False-negative results are seen in:
- Recent history of TB infection within 8 to 10 weeks.
- Cutaneous anergy where the immune system is very week.
- Younger age group less than 6 months of age.
- History of recent vaccination like measles and smallpox.
- In patients with a history of very old TB.
- In an exaggerated tuberculous patient.
- Incorrect injection of the tuberculin.
- Incorrect interpretation of the result.
Mechanism of Cell-Mediated Immunity:
The mechanism can be explained in two ways:
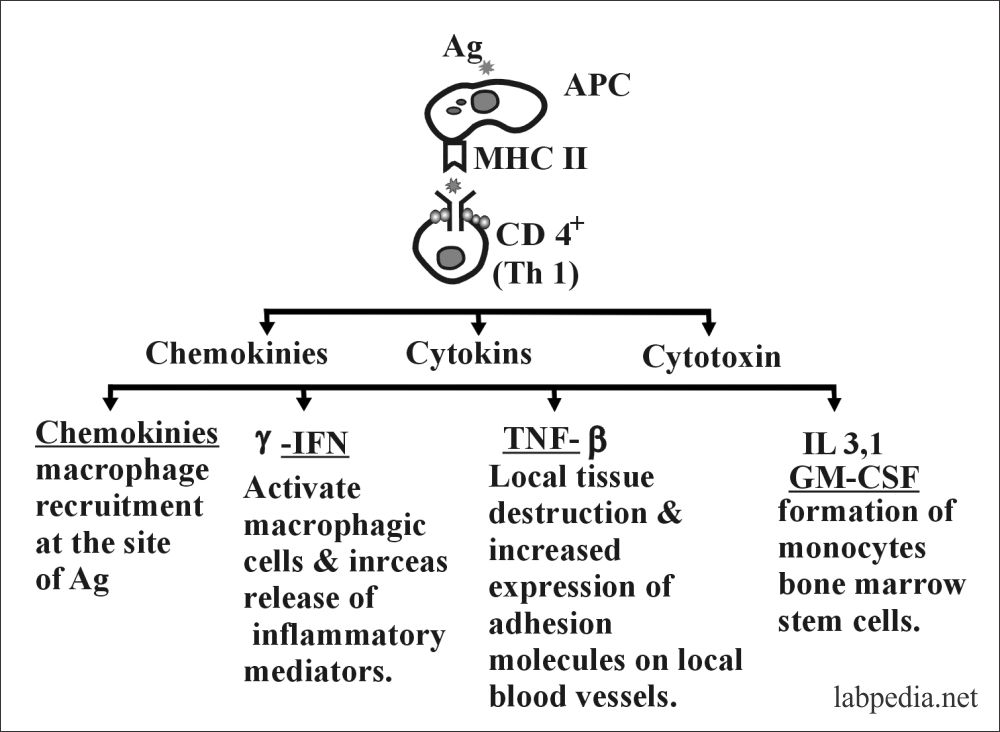
A. This was described by Dumond, who gave the name to different lymphokines produced by the activated CD4+ T-lymphocytes (Inflammatory cells – Th1).
Activated CD4+ cell produces lymphokines, named as follow:
- Macrophage chemotactic factor (MCF)
- Macrophage inhibition factor (MIF).
- Macrophage activating factor (MAF).
- Specific macrophage activating factor (SMAF).
- Neutrophil chemotactic factor. This attracts polys, monocytes, eosinophils, and lymphocytes.
- IL-2 called the T-cell growth factor.
- Skin reactive factor.
- Interferon-γ. This activates macrophagic cells, and it is antiviral.
- Lymphotoxin (TNF- b) It can lyes the tumor cells.
- TNF-α- it affects the endothelial cells.
- TF (Transfer Factor), this will transfer the memory of the exposed Ag.
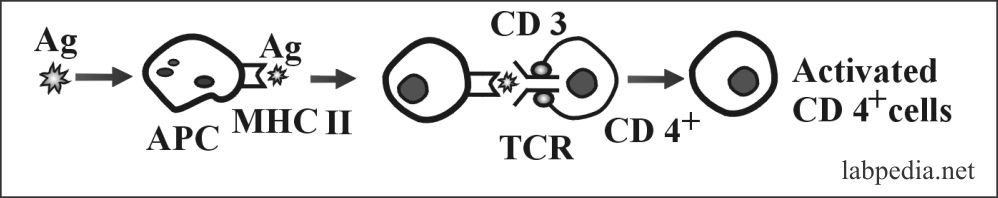
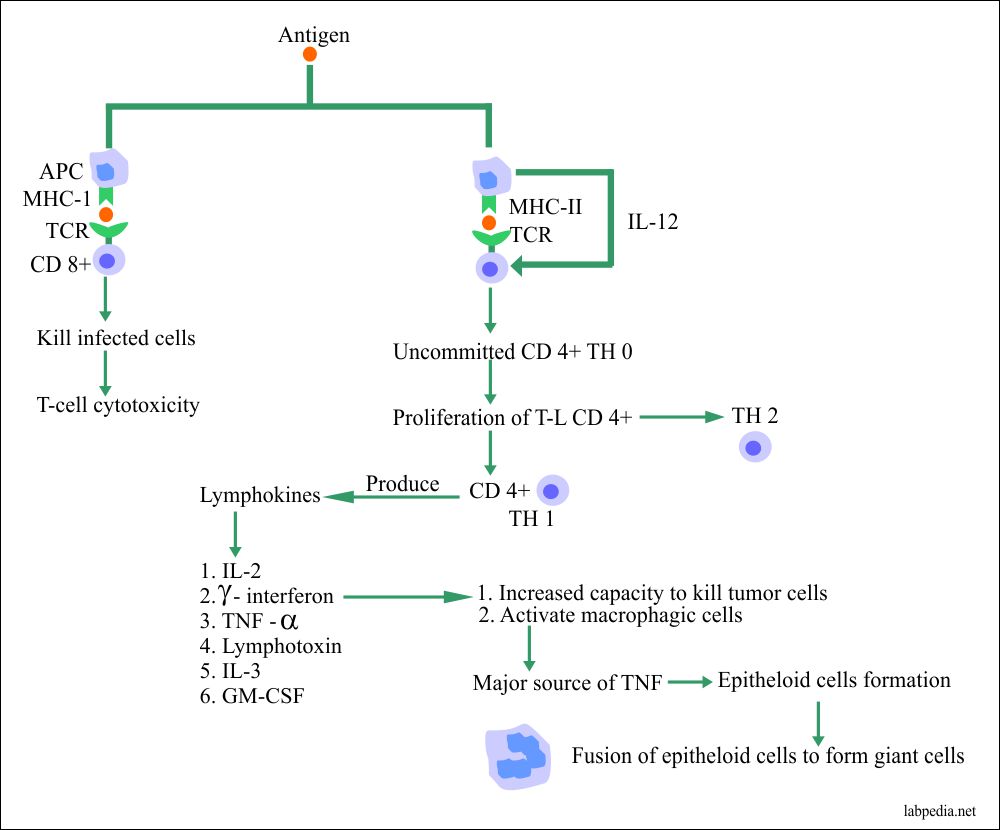
B. Antigens, after processing by APC when presented along with MHC-II molecule, stimulates CD4+ (Th0), which in turn transforms to Th1, which gives CMI and Th2, which stimulate B-L. Another possibility is that if APC presents Ag along with MHC-I, then CD8+ cells are stimulated. These events can be summarized:
TNF-α and Lymphotoxin
- Increase secretion of prostacyclin, which leads to vasodilatation.
- Increase expression of E- selectin.
- Chemotactic factor.
All the above (1, 2, 3) functions ultimately lead to extravasation of lymphocytes and monocytes at the site.
Summary: The Mechanism of Type IV CMI can be summarized as Follows.
Mainly type IV CMI is by activation of CD4+ Th1 cell, which gives rise to granuloma formation, by the release of lymphokines. The major role is by the TNF. In the absence of TNF, granuloma fails to develop.
T-L (CD8+Tc) Cytotoxicity
Tc cells cause lysis on cell contact, and there is no killing of bystander cells. Because the lytic molecules are released only at the site of TCR contact.
Tc-cell Cytotoxicity is important in:
- Graft rejection
- Viral infection
- Tumor immunity
Mechanism of killing:
There is a killing of the target without phagocytosis.
This may take place by means of:-
- Perforin, granzyme dependant killing, which drills holes in the cell membrane in the presence of calcium (just like C9).
- Proteolytic enzyme production: (lymphotoxin) activates an enzyme in the target cells to cleave DNA in the Nucleus. There is the presence of clumps of nuclear DNA. This looks to be a consequence of the process of programmed cell death or apoptosis.
Causes of Type IV Hypersensitivity reaction:
- Bacterial causes are Mycobacterium tuberculosis, Brucellosis, Leprosy, and Syphilis.
- Viral causes are Smallpox, Measles, Herpes simplex.
- The fungal cause is Candidiasis, Histoplasmosis, and Coccidioidomycosis.
- The protozoal cause is Leishmaniasis.
- Chemical causes are hair dyes, nickel salt, chromium, potassium dichromate, silicosis, and berylliosis.
- Drugs causes are penicillin and neomycin.
- Crohn’s disease.
- Schistosomiasis.
- Sarcoidosis.
Tuberculosis:
In tuberculosis, there is a balance between the activated macrophagic cells in two ways:
- Controlling the infection.
- At the same time causing tissue damage in the infected tissue.
- In the lung, there is a granulomatous reaction with cavitation and the spread of the bacteria.
- These lesions may be accompanied by fibrosis.
- Granuloma consists of:
- Central caseous necrosis (looks like cheezy necrosis).
- Surrounded by epithelioid cells.
- There are few multinucleated giant cells.
- There are mononuclear cells infiltrate at the edge.
Various types of Cell-mediated Type IV hypersensitivity:
| Type of reaction | Type of antigen |
Time period | Clinical presentation | Histological findings |
| Contact hypersensitivity |
|
48 to 72 hours | Eczemas like signs and symptoms | Infiltrate of lymphocytes, later macrophagic cells, and edema of the epidermis |
| Tuberculin reaction | Intradermal injection of tuberculin | 48 to 72 hours | Local induration | Infiltrate of lymphocytes, monocytes, and macrophagic cells |
| Granuloma formation | Persistent antigen, or non-immunoglobulin stimuli like talc powder | 21 to 28 days | Granuloma formation in the lung, or skin | Macrophagic cells, Epitheloid cells, multinucleated giant cells, and fibrosis |
What is the Difference between Necrosis of Type – III Immune Complex Disease and Type – IV CMI?
Type – III necrosis is dependant on complement and neutrophils, while type IV is dependant upon T-lymphocytes and macrophages.
Treatment
- A corticosteroid may be given.
- Antibodies like anti-lymphocytes and anti-thymocytes may be tried.
- Cytotoxic drugs like azathioprine, cyclosporin, and cyclophosphamide may also be used.
- Treatment of specific disease like Tuberculosis, need anti-tuberculous therapy.
The Differentiation of the hypersensitivity reactions:
Comparison of the hypersensitivity reactions:
| Type-I, anaphylactic, immediate, and atopy | Type-II cytotoxic | Type-III immune- a complex disease | Type-IV delayed-type, cell-mediated immunity | |
| Depends | IgE | IgG, IgM | IgG. IgM, IgA | T-lymphocytes |
| Immune cell | B-Lymphocytes | B-L | B-L | T-L |
| Passive transfer with | IgE, cytotropic Ab | Ab | Ab | T-L |
| Antigen | Heterologous | Autologous | Auto or heterologous | Auto or heterologous |
| Complement | No | Yes or No | Yes | No |
| Cells involved in the initiation | Mast cells basophil | None | None | APC, T-L, macrophages |
| Target tissue | Vascular endothelium, bronchi, smooth muscle, | Blood or tissue cells | vascular and epithelial cells | Modified self infected cells |
| Mechanism | Ag + IgE mast cells basophils and chemical mediators | Ig + tissue Ag = C-activation = lysis , opsonization, and ADCC | Ag + Ab =C-activation,Mast cells and Neutrophil activation | CD4+ activated =mediators, CD8+= cytotoxic |
| Inflammatory cells attracted | Eosinophils and neutrophils | Neutrophils | neutrophil | monocytes and macrophage |
| Primary results | Increase vascular permeability, increase transudation erythema, edema, wheal, bronchospasm | cell lysis, phagocytosis, inflammation, and decreased C | vasculitis, necrosis, thrombi, vasoconstriction, decreased C | Erythema, induration, granuloma formation |
| Treatment | Avoidance, antihistamine, steroids | Immunosuppressant, steroids | Immunosuppressant, steroids | Anti-inflammatory, steroids |
| Example | Drugs, hay fever, bees, food, vaccines | Glomerulonephritis, SLE, HD of newborn, blood transfusion reaction, autoimmunity | Arthus reaction, serum sickness, chronic GN, SLE, Rheumatoid arthritis, vasculitis | Contact dermatitis, tuberculosis fungal and viral infection, Graft, rejection |
| General beneficial effects | IgE secretions, resistance to the parasite, the expulsion of inhaled pathogens by wheezing, and GI secretions | Antibacterial, and antiviral | Acute inflammation, neutrophil activation | Immunity to T.B, virus, and fungus |
Table XXI – Comparison of Hypersensitivity Reactions
Type of Hypersensitivity reactions and their immunologic mechanism:
| Hypersensitivity reaction | Type of reaction | Time of development | Type of Antibody | Type of cells involved | Role of complement | Example of the disease |
| Type 1 | IgE dependent reaction | Immediate | IgE | Mast cells | No |
|
| Type II |
|
Immediate | IgG and IgM | Macrophagic cells | Frequently involved |
|
| Type III | Immune-complex mediated reaction | Immediate | IgG and IgM | Neutrophils | Yes |
|
| Type IV | Cell-mediated reaction | Delayed | None |
|
None |
|
Go Back to Elementary Immunology