Adrenal Gland Hormones Interpretation, (Cortisol and Aldosterone)
Adrenal Gland Hormones
What sample is needed for Adrenal Gland Hormones?
- The serum of the patient is required.
- A urine sample may be used.
- For catecholamines (Epinephrine and Norepinephrine), plasma in heparin or EDTA is needed.
- Transport this plasma on ice, centrifuge at 4 C within 30 minutes, and separate the plasma. Now, freeze till the test is run.
- Urine may be collected for 24 hours. Add 6 M HCl and Refrigerate during collection.
- For Cortisol, Serum is needed. Can use heparinized plasma.
- Urine for 24 hours is collected with the addition of boric acid.
- The serum is stable for 2 days at 2 to 8 °C.
- For aldosterone, a test can be done on plasma (heparin, EDTA, or citrate).
- The serum can also be used.
- The patient must be upright for 2 hours before the sample is taken.
- Urine is collected for 24 hours with boric acid, and during collection, it is refrigerated.
- For Estrogen can be estimated in the serum.
- The serum needs to be frozen immediately after collection.
- A urine 24-hour sample is collected with the addition of boric acid.
What are the precautions before performing the Adrenal gland tests?
- A fasting sample is needed.
- Avoid exercise or physical activity.
- Reduce stress before performing this test.
- Avoid herbal medicines and any medication that interferes with the test.
- Avoid a nuclear scan before this test.
- The aldosterone AM sample is higher than PM.
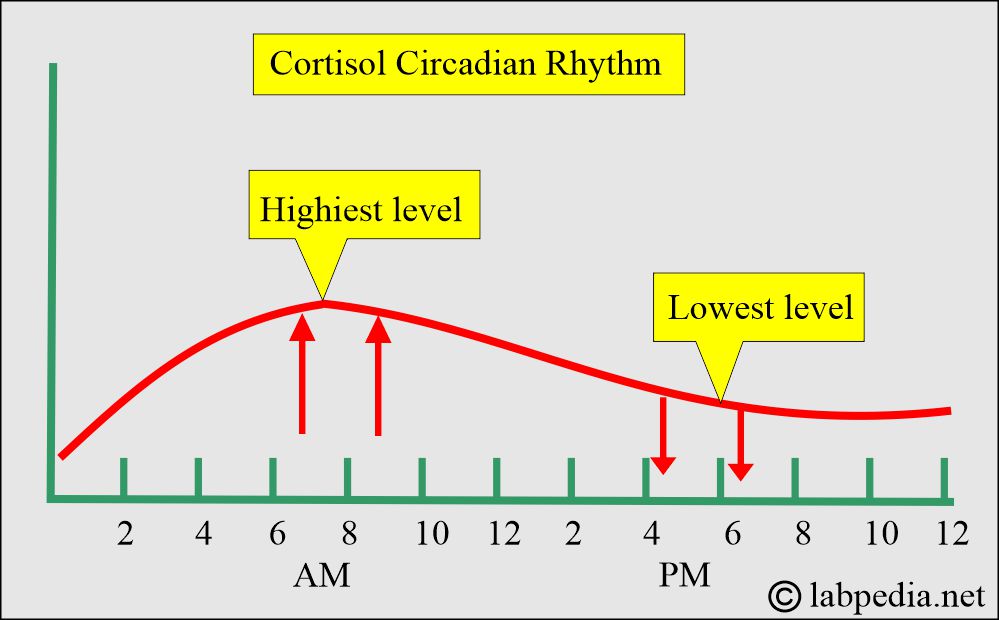
- Cortisol’s highest level is 8 AM and >50% less at 8 PM.
- Transport the plasma on ice to the lab.
- Centrifuge at 4 °C.
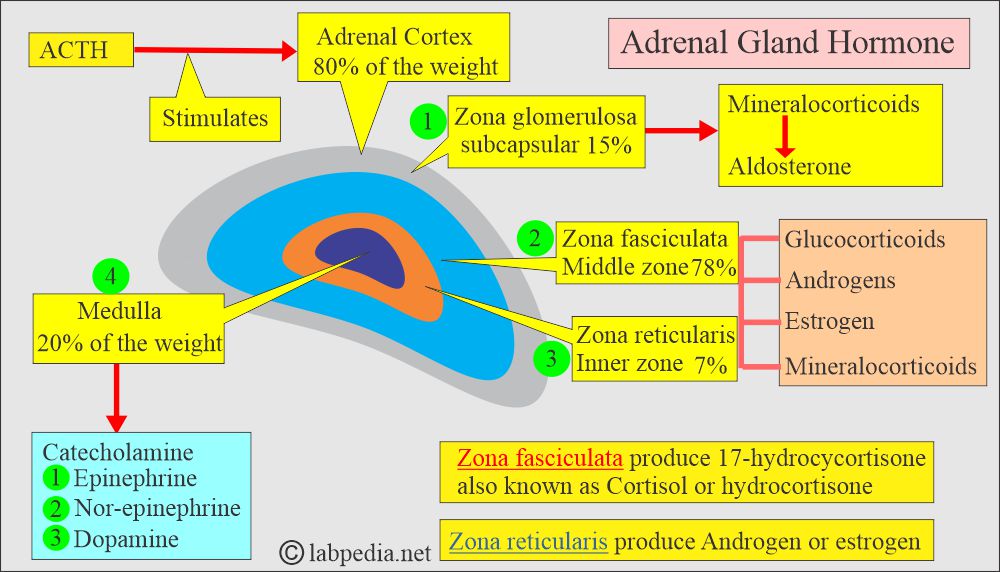
What is the anatomy of adrenal glands?
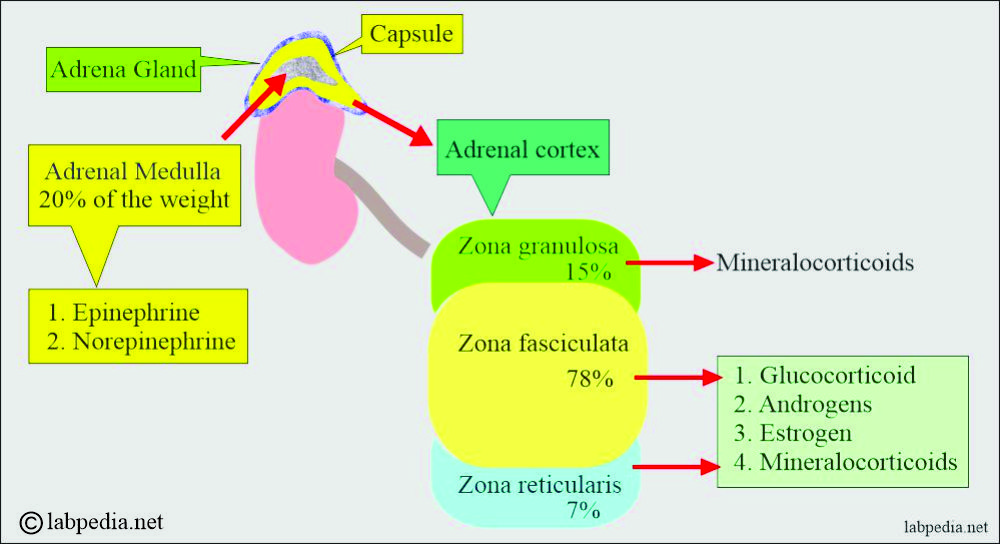
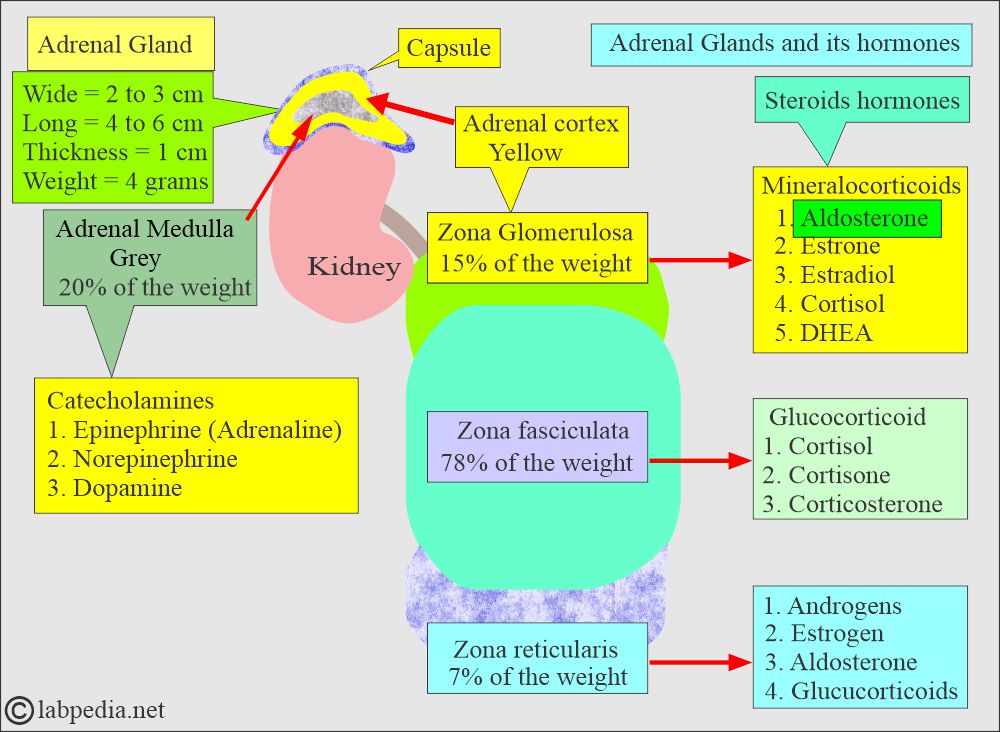
- Adrenal glands consist of the following:
- The adrenal medulla is grey.
- The adrenal cortex is yellow.
- The adrenal cortex is derived from the mesoderm.
- These hormones maintain the homeostasis of the body.
- The adrenal medulla is derived from the ectoderm.
- Adrenal gland measure:
- Wide = 2 to 3 cm.
- Length = 4 to 6 cm.
- Thickness = 1 cm.
- Weight approximately = 4 grams (regardless of age and sex).
What are the adrenal cortex hormones?
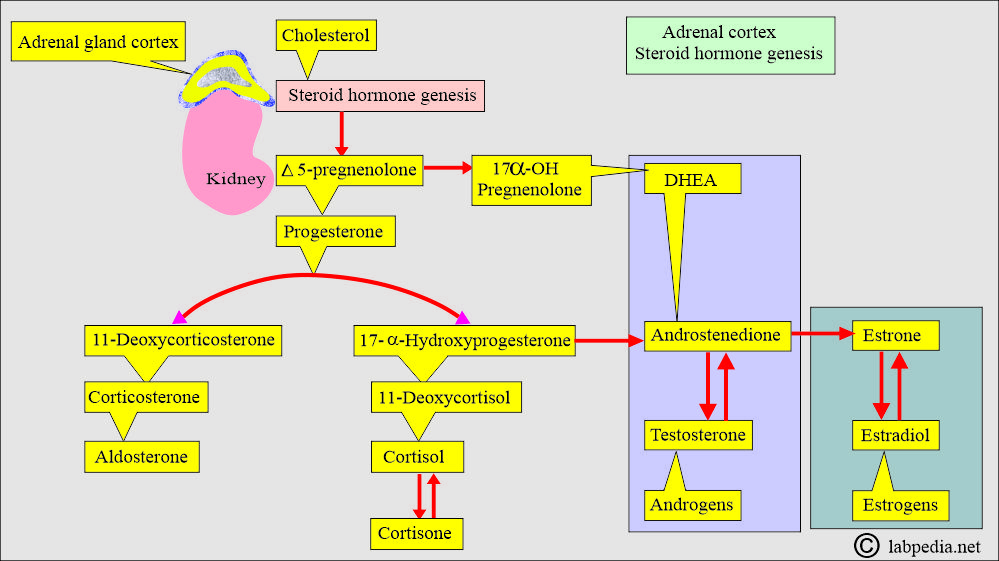
What is the fate of Steroid hormones?
- These are synthesized from the cholesterol in the adrenal glands and gonads.
- The nature and quantity of the steroid hormone produced by the adrenal glands and gonads differ.
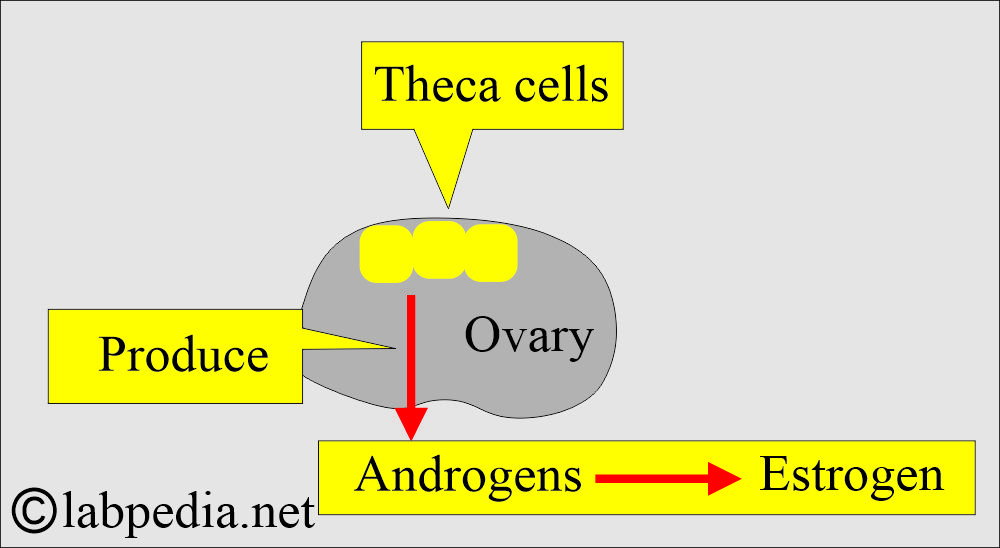
- The ovaries and testes contain enzymes synthesizing male and female sex hormones.
- Steroid hormones circulate in the blood in free and bound forms.
- In plasma, these are bound to the carrier protein or albumin.
- Steroid hormones conjugate to glucuronide or sulfate and are excreted by the kidneys or gastrointestinal tract.
- 90% to 96% of steroids have a high affinity for the carrier protein globulin.
- 60% to 70% of the circulating steroids are bound to albumin, which has a low affinity for carrier protein.
- Androgens produced by the theca cells of the ovary are converted to estrogen.
What is the origin of mineralocorticoid?
- The primary example of mineralocorticoid is aldosterone.
- It is produced in the zona glomerulosa of the adrenal cortex.
- Aldosterone regulates sodium and potassium.
- Other examples of endogenous mineralocorticoids are progesterone and deoxycorticosterone.
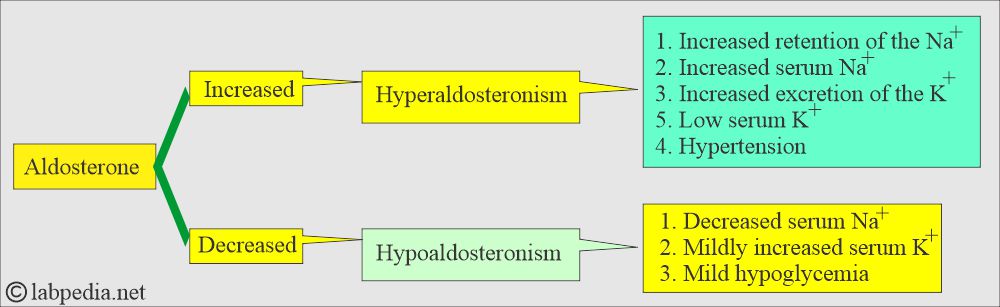
Discuss the Aldosterone?
- It is the major Mineralocorticoid produced by the adrenal cortex, 200 µg/day.
- It promotes renal K+ excretion and increases water retention by increasing renal Na+ retention.
- It increases the plasma concentration of the Na+ by increasing the Na+ absorption in the renal tubules.
- Aldosterone is present in a very minute amount in the plasma, making it difficult to measure accurately.
- If someone stands for a long time, his plasma aldosterone level will be between 5 and 20 ng/dL.
- If the person is lying for several hours, the aldosterone level will fall and maybe 10% to 40% less than in the upright position.
- What is the metabolism of Aldosterone?
- The liver converts aldosterone into glucuronide and tetrahydro-glucuronide; this will be excreted in the urine.
- Kidneys also inactivate aldosterone by changing it into water-soluble glucuronide.
- How would you describe Hyperaldosteronism?
- It is usually due to an adrenal tumor that has S/S of:
- Increased serum Na+.
- Decreased K+.
- Hypertension.
- Plasma aldosterone level is increased.
- Urine excretion of aldosterone is also increased.
What are the causes of Primary aldosteronism?
- Adrenal tumor, usually adenoma of the adrenal cortex.
- Bilateral nodular hyperplasia.
What are the causes of Secondary aldosteronism?
- Low serum Na+ level.
- ACTH
- High serum K+ level.
How will you differentiate Primary aldosteronism from secondary aldosteronism.?
| Lab test | Primary aldosteronism due to | Secondary aldosteronism | ||
| Hyperplasia | Adenoma | Edema (CCF and Cirrhosis) | Accelerated Hypertension | |
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
What is the differential diagnosis of adrenal adenoma, carcinoma, and idiopathic hyperplasia?
| Lab test | Adenoma | Adrenal carcinoma | Idiopathic hyperplasia |
| Plasma renin activity | Suppressed/ very low | Suppressed/ very low | Not markedly suppressed |
| Plasma /urine aldosterone | Increased | Markedly increased | Usually mild increase |
| Hypokalemia | Increased | More marked increase | Not markedly increased |
| Aldosterone response to posture | Decreased or not increased (70% to 80%) | Often unchanged /or random increase | Increased in all cases |
| Excess hormone production |
|
|
|
Discuss the Glucocorticoids?
- Cortisol is the most potent glucocorticoid.
- It is like cortisol, which is gluconeogenic.
- Cortisol is produced at 25 mg/day by the adrenal cortex.
- It regulates intermediary carbohydrate metabolism.
- What are the functions of glucocorticoids?
- It has a metabolic function.
- It has an inflammatory function.
- This is also anti-inflammatory.
- It has a growth-suppressing effect.
- It influences the level of awareness and sleep patterns.
- Glucocorticoids have a direct effect on glucose levels, and it increases the glucose level.
- Glucocorticoids’ main function is in Carbohydrate metabolism.
- There is gluconeogenesis in the liver.
- There is a decrease in glucose levels in the muscle, adipose tissue, and lymphatic tissue.
- In extrahepatic tissue, Glucocorticoids antagonize insulin.
Discuss the Cortisol?
- Cortisol is the most potent naturally occurring glucocorticoid.
- The daily secretion of cortisol is 25 mg/day.
- But the plasma shows a level of 6 to 25 µg/dL.
- Cortisol is formed from the cholesterol in the zona fasciculata and zona reticularis of the adrenal cortex.
- When cortisol is released into the circulation, it binds with corticosteroid-binding globulin and is transported as such.
- What are the metabolic functions of cortisol?
- Cortisol is metabolized and conjugated in the liver into several inactive forms.
- >90% of cortisol and its metabolite cortisone is conjugated with glucuronic acid and excreted in the urine as a conjugate.
- <2% of cortisol, which is not metabolized, is excreted in the urine as free cortisol.
- Cortisol and its oxidation product, cortisone, are inactivated in the liver by two separate processes:
- The reduction process is hydrogenation to tetrahydro derivatives.
- These products are conjugated with glucuronic acid and excreted in the urine.
- 30% to 50% of these appear as glucuronide conjugates of tetrahydro-derivates of cortisol and cortisone.
- All these compounds contain a dihydroxyacetone group in the side chain, known as 17-hydroxycorticosteroid (17-OHCS).
- The RIA kits can chemically estimate 17-hydroxycorticosteroid (17-OHCS). In the past, the Porter-Silber reaction was used, but it is now obsolete.
- Determining plasma cortisol is useful in diagnosing both hypo- and hyperconditions adrenocortical diseases.
- Not >1% of the total cortisol synthesized in the body daily is excreted as such in the urine.
- What are the functions of the cortisol?
- Cortisol acts on the target cells by penetration and transport to the cell nucleus.
- It will bind the DNA and alter the transcription of RNA.
- Cortisol alters the various metabolic processes.
- It accelerates the enzymatic breakdown of muscle proteins and the conversion of their amino acids into glucose.
- Fat is metabolized for the provision of energy.
- Cortisol acts antagonistic to insulin action by inhibiting glucose uptake by the muscles.
- It decreases the cellular reaction to the inflammatory agents.
- It decreases antibody formation, leading to poor immune response.
- This is the main hormone of the adrenal cortex that maintains life and protects the body from stress.
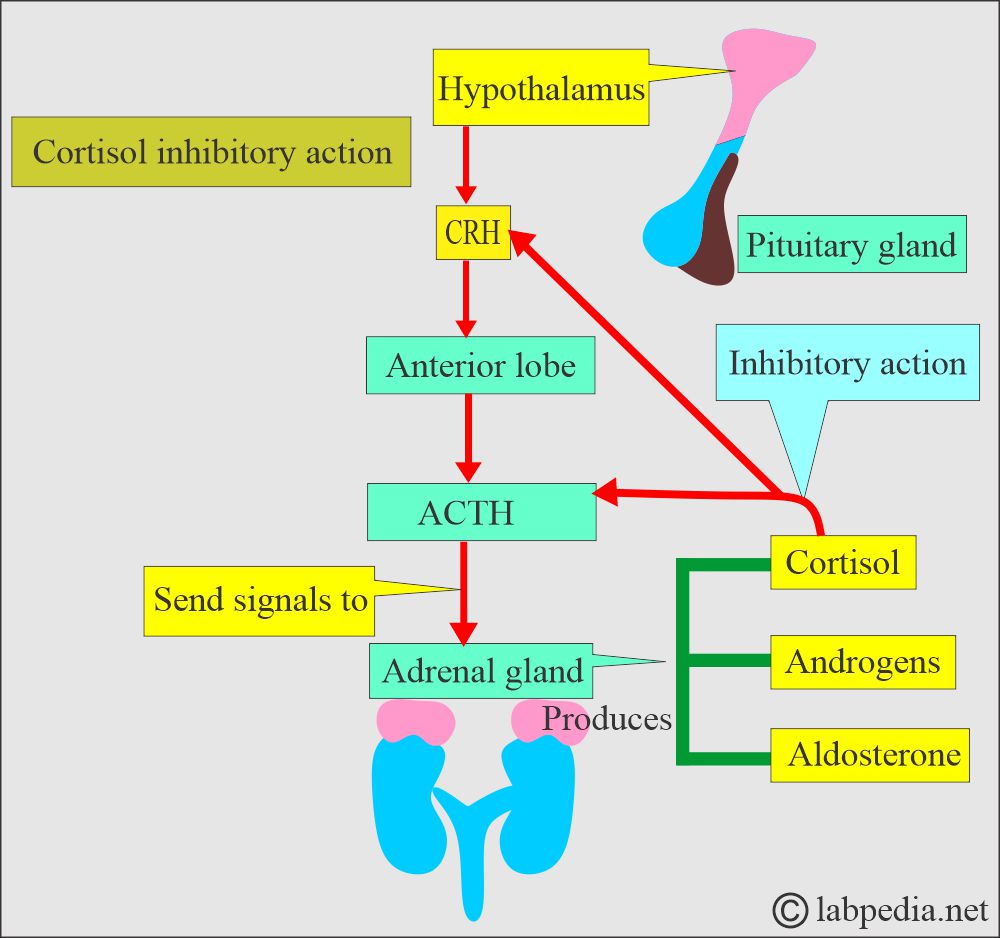
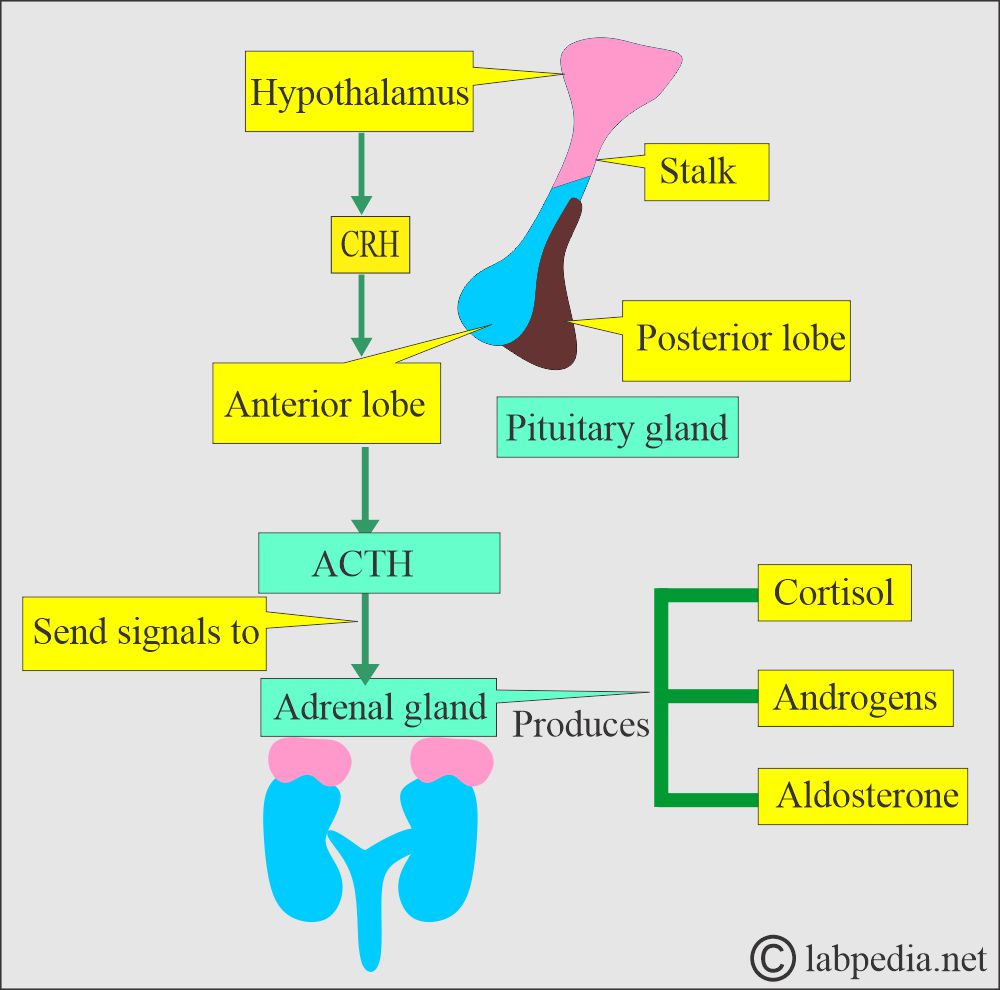
- Hypothalamus hormone CRH travels through the portal circulation to stimulate the production of ACTH, β-lipoprotein, γ-lipoprotein, endorphins, and enkephalins by the anterior pituitary.
- Cortisol secretions follow ACTH stimulation of the adrenal cortex, and ACTH is the main regulator of cortisol secretion and adrenocortical growth.
- How is Cortisol transported in the plasma?
- 85% is transported by corticosteroid-binding globulin (CBG called transcortin).
- 10% bound to albumin.
- 5% is in free form (not bound to proteins).
- The cortisol follows the ACTH pattern; it is high early in the morning and lowest at midnight.
- Cortisol inhibits the secretion of ACTH from the pituitary gland and also inhibits CRH from the hypothalamus.
What are the Adrenal androgens?
- It is like such as dehydroepiandrosterone (DHEA) and androstenedione. These are also called sex hormones.
- The adrenal androgens include:
- DHEA is the principal androgen, secreted at 20 mg/day.
- Testosterone (converted to estradiol).
- DHEA is converted to Androstenedione, which in turn is converted to estrone.
The adrenal medulla
What are the hormones of the adrenal medulla?
- It is a neuroendocrine gland that secretes:
- Epinephrine.
- Norepinephrine.
- Both act on the sympathetic nervous system.
- These hormones regulate the acute response of the body to external stimuli.
Discuss the ACTH hormone?
- ACTH (Adrenocorticotropin hormone) from the pituitary gland stimulates the adrenal cortex.
- After the stimulation of the adrenal cortex by the ACTH, the process of steroidogenesis starts with cholesterol.
- The pituitary gland (ACTH) is stimulated by the Hypothalamic hormone (Corticotropin-releasing factor (CRH).
- Serum ACTH level has a diurnal variation:
- The peak level is at 7 AM at about 200 pg/ml.
- ACTH level declines and the lowest level is around 100 pg/ml at midnight.
- What are the factors for ACTH secretion?
- High circulating levels of cortisol suppress ACTH and CRH.
- At the same time, the low level of cortisol stimulates their secretion.
- There is diurnal variation in the secretion of ACTH and cortisol levels. There is a sleep-wake pattern.
- ACTH peak is 3 to 5 hours after sleep begins and declines throughout the day. Cortisol follows the same pattern.
- Stress increases ACTH secretion, which leads to increased cortisol levels.
- The peak level is from 8.00 to 9.00 AM. The highest level is early morning, and the lowest is midnight.
What are the normal levels of adrenal gland hormone?
- Epinephrine = <50 pg/mL
- Urine epinephrine = 0 to 20 µg/ day
- Norepinephrine = 110 to 410 pg/mL
- Urine norepinephrine = 15 to 80 µg/ day
- Dopamine = <87 pg/mL
- Urine dopamine = 65 to 400 µg/ day
- Cortisol Total
- Cord blood = 5 to 17 µg/dL
- Infants = 2 to 11 µg/dL
- Child 1 to 16 years at 8 am = 3 to 21 µg/dL
- adult 8 am = 5 to 23 µg/dL
- 4 pm = 3 to 16 µg/dL
- Urine cortisol (free) =
- Adult = 20 to 90 µg/ day or (<100 µg/day)
- Child = 2 to 27 µg/day
- Aldosterone
- Cord blood = 40 to 200 ng/dL
- Full-term infant 3 days = 7 to 184 ng/dL
- Infants 1 to 12 months = 5 to 90 ng/dL
- Children 1 to 2 years = 7 to 54 ng/dL
- Children 2 to 10 years =
- Supine position = 3 to 35 ng/dL
- Upright position = 4 to 48 ng/dL
- Adult
- Supine position = 3 to 16 ng/dL
- Upright position = 7 to 30 ng/dL
- Estrogen Total
- Male = 20 to 80 pg/mL.
- Female
- Luteal phase = 160 to 400 pg/mL.
- Follicular phase = 60 to 200 pg/mL.
- Postmenopausal = <130 pg/mL
What is the outcome of Adrenal Hyperfunction?
- Excess of Cortisol causes Cushing’s syndrome.
- Excess of Aldosterone causes Hyperaldosteronism.
- Excess of Androgens causes Virilizing syndrome.
What are the findings of Primary Hyperadrenalism?
- The cortisol level is raised.
- ACTH level decreases.
What are the lab findings on primary adrenal insufficiency (Addison’s disease)?
- This is due to the diseases of the gland.
- The cortisol level is decreased.
- Serum sodium is low.
- The glucose level is decreased.
- ACTH level is raised.
- Potassium, calcium, and blood urea are raised.
What are the lab findings of Secondary Hypoadrenalism (secondary or tertiary Adrenal insufficiency)?
- This is due to external factors that lead to the under-activity of the glands.
- Cortisol level is decreased.
- ACTH level is low.
What are the lab findings of Cushing’s syndrome?
- There is no diurnal variation of ACTH, and it is absent.
- There is an elevated level of Cortisol, Glucose, and Sodium.
- There is a decreased Potassium level.
What are the lab findings of Adult adrenogenital syndrome?
- There is an elevated level of:
- DHEA
- Urine 17- ketosteroids
- ACTH
- There is a decreased level of:
- Cortisol
What are the lab findings of Congenital Adrenal Hyperplasia:
- There is an elevated level of:
- ACTH
- Androgens level
- Decreased level of:
- Cortisol
- Aldosterone
What are the lab findings of Primary Hyperaldosteronism (Conn’s syndrome)?
- There is an elevated level of:
- Aldosterone urine and blood
- Serum sodium
- There is a decreased level of:
- Potassium.
- Renin.
- No response to the aldosterone suppression test.
Questions and answers:
Question 1: What are the lab findings in Cushing's syndrome?
Question 2: What are the lab findings of Addison's diseases?

Informative content.. thx
Thanks.
Useful in sexual development & sexual disorder
Thank you for your useful information
Thanks.