Crigler-Najjar Syndrome
Crigler-Najjar Syndrome
(Hereditary Glucuronyl-Transferase Deficiency)
What sample is needed for the diagnosis of Crigler-Najjar Syndrome?
- The patient’s serum is needed.
What is the Definition of Crigler-Najjar Syndrome?
- There is a marked congenital deficiency or absence of the glucuronyl-transferase enzyme, which is needed for the conjugation of bilirubin.
- Crigler-Najjar type 1 has a complete deficiency of the Glucuronyltransferase enzyme.
- Unconjugated bilirubin is usually 25 to 50 mg/dL.
- Crigler-Najjar type II has a partial deficiency of the Glucuronyltransferase enzyme.
- Unconjugated bilirubin is usually 5 to 20 mg/dL.
How will you discuss the pathophysiology of Crigler-Najjar Syndrome?
- Crigler-Najjar syndrome is a rare familial autosomal recessive disease.
- This is rare, but it is a very severe disease; 50% of babies die within one year of birth.
- The rest (half) of the patients suffer from severe brain damage.
What is the Mechanism of Crigler-Najjar Syndrome?
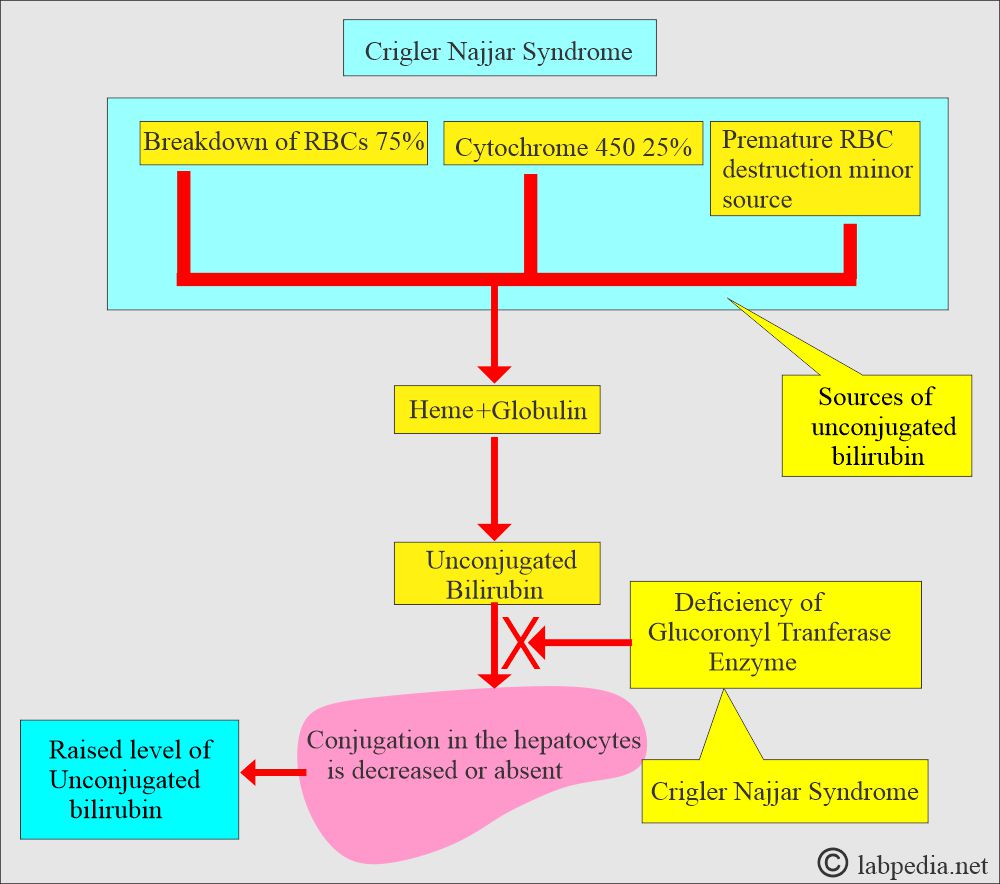
- There is a congenital marked deficiency or absence of the glucuronyl-transferase enzyme (GTE).
- GTE converts unconjugated bilirubin into bilirubin-glucuronide in the hepatocytes.
- The UGT1A1 gene coding has a severe deficiency of the enzyme.
- This is caused by gene mutation and deletion.
- Classification of Crigler-Najjar Syndrome:
- Type I has no glucuronyltransferase enzyme, leading to neonatal jaundice and kernicterus.
- Type 1 has almost no GTE and is a severe disease. There is a homozygous non-functional protein.
- There is no enzyme activity in the liver.
- Type II (Arias syndrome) contains some glucuronyltransferase enzyme activity, usually <10% of the normal, and jaundice appears later.
- Type II has a partial or reduced level. The disease is less severe than type 1.
- There is <10% of the normal enzyme activity, and survival to adulthood is possible.
- Now, unconjugated bilirubin (indirect bilirubin) can build up in the body and lead to jaundice.
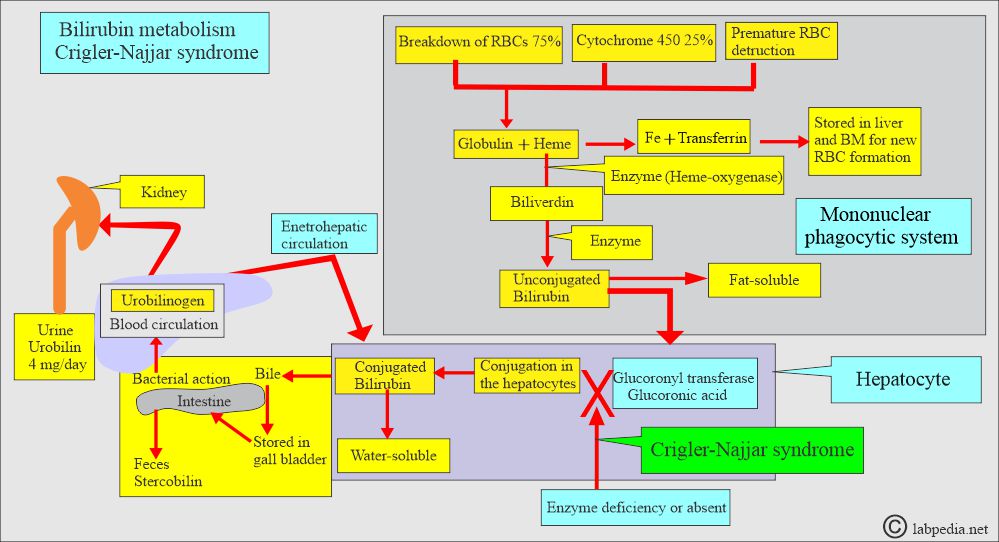
- The following diagram of bilirubin metabolism provides a good understanding of this disease and the mechanism of Crigler-Najjar syndrome.
What are the Side effects of unconjugated bilirubin (Crigler-Najjar Syndrome)?
- This unconjugated bilirubin can cause damage to the brain, muscles, and nerves.
- Crigler-Najjar syndrome has a partial or complete deficiency of the glucuronyl-transferase enzyme.
What are the Signs and Symptoms of Crigler-Najjar syndrome?
- These patients may have confusion.
- There is yellowness of the eyes and skin due to raised unconjugated bilirubin.
Crigler-Najjar syndrome type 1:
- This condition is inherited as an autosomal recessive trait.
- Jaundice develops in the first few days of birth and is severe by the second week.
- Bilirubin may be as high as 25 to 50 mg/dL.
- No conjugated bilirubin is present in the serum or urine.
- These patients may develop kernicterus due to brain damage.
- Unconjugated hyperbilirubinemia always exceeds 5 mg/dL, and time may exceed 20 mg /dL.
- Kernicterus, which occurs when bilirubin deposits in the brain, affects the basal ganglia, primarily the lenticular nucleus.
- Kernicterus may show hypotonia, deafness, lethargy, oculomotor palsy, and ultimately death.
- These patients may also have diarrhea, vomiting, fever, seizures, and difficulty swallowing.
- Early liver transplantation is the only effective treatment.
What are the Lab findings of Crigler-Najjar syndrome?
- Fecal urobilinogen is very low.
- Liver function tests are normal.
- The BSP test is normal.
- The liver biopsy is normal.
- There is no evidence of hemolysis.
What is the outcome of type 1 Crigler-Najjar syndrome?
- Untreated patients often die of kernicterus before they cross the age of 18 months.
- Type 1 can be considered when there is unconjugated hyperbilirubinemia of >20 mg/dL after one week of age, there is no evidence of hemolysis, and breast milk jaundice is ruled out.
How will you treat the Crigler-Najjar syndrome type 1?
- Phlebotomy and plasmapheresis will reduce the unconjugated bilirubin.
- However, encephalopathy usually develops.
- Early liver transplantation is the only hope.
How will you treat the type 2 Crigler-Najjar syndrome?
- This is a rare autosomal dominant disorder.
- There is a partial deficiency of the glucuronosyltransferase enzyme.
- Neurological complications are rare.
- Clinically, there are no signs and symptoms except mild jaundice.
- Bilirubin may be 5 to 25 mg/dL.
- There is roughly 10% of the normal activity of the enzyme.
- There is a possibility of the child surviving to adulthood.
- There is a good response to phenobarbitone therapy, and the patient may live longer than expected.
- With phenobarbitone therapy, bilirubin may be <5 mg/dL.
- Treatment:
- Phenobarbitone therapy may lead to normal life expectancy.
How will you differentiate between type 1 and type 2 Crigler-Najjar syndrome?
| Clinical/lab findings | Type 1 | Type 2 |
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
How will you diagnose Crigler-Najjar syndrome?
Crigler-Najjar syndrome Type 1:
- Indirect bilirubin is increased. It appears on the first or second day of life and may be raised to 12 to 45 mg/100 ml.
- Conjugated bilirubin is absent in the serum.
- Bilirubin is absent in the urine.
- Fecalurobilinogen is very low in amount.
- Liver function tests are normal.
- The BSP test is normal.
- The liver biopsy is normal.
- There is no evidence of hemolysis.
- These patients die by the age of 18 months due to raised unconjugated bilirubin, leading to kernicterus.
- Rule out causes of hemolysis in case of persistent unconjugated bilirubinemia of around 20 mg/dL after one week of the infant’s age.
Crigler-Najjar syndrome Type 2:
- The raised bilirubin level is low in the range of 7 to 20 mg/100 ml.
- Unconjugated bilirubin increases with fasting and the removal of fats from the diet.
- It may respond to phenobarbitone therapy, and the level may decrease to <5 mg/dL.
- Liver function tests are normal.
- The liver biopsy is normal.
- Fecal urobilinogen is very low.
What is the Treatment of Crigler-Najjar syndrome?
- These patients need phototherapy throughout their lives (blue LED light). This is difficult because patients need 10 to 12 hours of treatment daily.
- Phototherapy may not work in some patients after the age of 4 years due to the thickness of the skin.
- Drugs that may be given are phenobarbital and Vit. E, Vit. C, Coenzyme Q, Actigall, L-carnitine, and Creatine.
- Blood transfusion exchange or plasma exchange may help to lower the bilirubin level.
- Calcium may be given to bind the bilirubin in the gut.
- In type 1, liver transplantation may be done as early as possible, which is the only hope for longer survival.
How will you describe different types of inherited jaundice?
| Clinical parameters | Unconjugated Hyperbilirubinemia | Conjugated Hyperbilirubinemia | |||
| Gilbert’s disease | Type 1 Criggler-Najjar | Type II Criggler-Najjar syndrome | Rotor’s syndrome | Dubon-Jhonson syndrome | |
| Inherited mode | Autosomal dominant | Autosomal recessive | Autosomal dominant | Autosomal recessive | Autosomal recessive |
| Incidence | <7% of the population | Very rare | Uncommon | Rare | Uncommon |
| Age at onset | In adolescence | In infancy |
|
Early adulthood |
|
| Pathogenesis | Glucoronyl transferase enzyme deficiency (GTE) | GTE decreased | Marked decrease | Impaired conj. bilirubin excretion | Impaired cong. bilirubin excretion |
| Bilirubin level |
|
Mainly indirect | Mainly indirect |
|
|
| Clinical signs/symptoms |
|
|
|
Asymptomatic jaundice in young adults | Asymptomatic jaundice |
| Effect of phenobarbitone | Decreased to normal | There is no effect | Marked decrease | —– | —– |
| BSP (Dye excretion) test | May be mildly impaired in <40% of cases | It is absent | _____ | Positive, Initial rapid fall and then rise in 40 to 90 minutes | Positive, Slow clearance, and no rise |
| Oral cholecyctography | Normal | Normal | Normal | Normal | GB is usually not visualized |
| Liver biopsy | Normal | —- | —- | No pigments | Characteristic pigments |
| Treatment | Not needed | There is no treatment | Not needed | ||
Questions and answers:
Question 1: What is the difference between type 1 and type 2?
Question 2: What is kernicterus?